Abstract
Aim: To investigate protease activated receptor 2 (PAR-2) expression in human coronary atherosclerotic lesions because PAR-2 is involved in the modulation of inflammatory events and vascular function.
Methods: An immunohistochemical analysis was performed on serial arterial sections, using the following antibodies: MDA2, a murine monoclonal antibody against malondialdehyde lysine epitopes of oxidised low density lipoprotein (oxLDL); HAM-56, a monoclonal antibody against human macrophages/foam cells; B5, a rabbit polyclonal antibody against PAR-2; and SAM11, a mouse monoclonal antibody against human PAR-2. Sections containing at least one lesion showing substantial immunostaining were counted as positive, and results were expressed as per cent of all sections of the same artery.
Results: PAR-2 expression was enhanced in human coronary atherosclerotic lesions. This phenomenon correlated with an increase in oxLDL epitopes in the coronary artery.
Conclusion: This study shows for the first time that PAR-2 expression is enhanced in human coronary atherosclerotic lesions, and suggests that PAR-2 dependent cellular trafficking may be one of the regulatory signalling responses to vascular injury. Further pharmacological studies will establish whether modulation (and in which direction) of PAR-2 represents a possible therapeutic target for controlling the vascular response to injury.
Keywords: atherosclerosis, protease activated receptor 2, inflammation
Thrombin is one of the key molecules involved in the development of vascular diseases. Thrombin does not only serve as a coagulation factor, but it also exerts cellular effects by activating protease (proteinase) activated receptors (PARs), a family of seven transmembrane G protein coupled receptors activated by proteolytic cleavage.1 The pathophysiological role in vivo of protease activated receptor 2 (PAR-2) remains poorly understood.1,2 PARs are vascular sensors for signalling of the trypsin-like coagulation serine proteases.1,2 PAR-2 is expressed in arteries3–7 and in the heart,8–10 and plays a role in the regulation of vascular tone4,7,11–14 and tissue inflammation.6–8,10,11,15–17 Endothelial cells have a primary role in mediating the vascular effects of PARs under physiological conditions, whereas PARs can be induced in smooth muscle cells under pathological conditions, and therefore play a more pathophysiological role.
“Targeting inflammatory cell signalling events of the coagulation system may become an important aspect of efforts to improve antiatherothrombotic treatment”
Because proteases are activated during pathological states such as haemorrhage, tissue damage, and inflammation, PARs have been suggested to play a crucial role in the development of functional and structural abnormalities in vascular lesions. Indeed, inflammation is a well established component of the vulnerable atherosclerotic plaque.18 Targeting inflammatory cell signalling events of the coagulation system may become an important aspect of efforts to improve antiatherothrombotic treatment. Because we hypothesised that PAR-2 activation is involved in inflammatory and injury response events,1 here, we attempt to verify whether PAR-2 plays a role in human coronary atherosclerotic lesions.
METHODS
Human subjects
Arteries were collected from adult (mean age, 41.8 years; SD, 5.6; n = 8) and elderly (mean age, 70.5 years; SD, 5.1; n = 6) men subjected to necropsy at the University of Naples, who had died in traumatic accidents. They were included in our study only if they were men (to avoid sex related differences) and had no classic risk factors for atherosclerosis (family history of coronary heart disease, diabetes, smoking, hypertension, or dislipidaemia), which were assessed by detailed medical history of clinical records, as described previously.19 Our study protocol was approved by the local human ethical committee.
Preparation of arterial sections, histological analysis, and immunohistochemical analysis
Using a stereo microscope, the entire left anterior descending and the right coronary arteries were dissected from each patient, cut open, washed thoroughly with cold sterile phosphate buffered saline (PBS), and placed in ice cold PBS containing 50μM butylated hydroxytoluene, 0.001% aprotinin, 50mM EDTA, 1μM deferoxamine, and 0.008% chloramphenicol, equilibrated with nitrogen. One of these segments was immersed in ornithine transcarbamoylase, flash frozen in liquid nitrogen, and 30–40 sections (7 μm thick) were prepared for computerised morphometric determination of lipid rich lesions by oil red O staining, as described previously.19–21 Next, we determined the cumulative area of all lipid accumulations for each section. Alcian blue staining was used to evaluate nuclear smooth muscle cell density.19 Another arterial segment was fixed in buffered 10% formalin, paraffin wax embedded, and 12–15 serial sections (5–7 μm thick) were prepared for immunohistochemistry, as described previously.19–21 Alternate serial sections were immunostained with: (1) MDA2, a murine monoclonal antibody against malondialdehyde lysine epitopes of oxidised low density lipoprotein (oxLDL)19–21; (2) HAM-56, a monoclonal antibody against human macrophages/foam cells (Axcel Accurate, Westbury, New York, USA)19–21; (3) B5, a rabbit polyclonal antibody against PAR-28,10,22; and (4) SAM11, a mouse monoclonal antibody against human PAR-2 (Zymed Laboratory, San Francisco, California, USA). All antibodies were used at a dilution between 1/500 and 1/100. Unless otherwise specified, epitopes recognised by the primary antibody were detected by an avidin–biotin–peroxidase method.19–21 Immunohistochemical colocalisation using two antibodies was performed and analysed by computer assisted imaging software.19–21
Statistical analysis
Results were analysed by one way ANOVA, followed by Bonferroni’s, and a p < 0.05 was considered to be significant. Numerical data obtained from immunohistochemistry were analysed for mean, variance, SD, kurtosis, and skew. Correlations between the results were also evaluated by linear regression analysis. All data were analysed by SPSS statistical package (SPSS Inc, San Diego, California, USA).
RESULTS
Extent and maturity of atherosclerotic lesions
Based on computer assisted imaging analysis of histological oil red O stained sections, we divided coronary atherosclerotic lesions into early class I lesions (fatty streaks), class II lesions (fibrous lesions), and advanced class III (fibroatheromatous lesions) and class IV (calcific lesions) lesions. The mean (SD) lumen stenosis of the lesions was 45% (6%) in adults and 65% (8%) in elderly men (p < 0.05). Mean intimal thickness increased with age in coronary arteries (p < 0.05). The nuclear density of the smooth muscle cells in the media, as an index of the maturity of the lesions,19,20 varied with the stage of the lesions, and ranged from a mean (SD) of 752 (123) smooth muscle cell nuclei/mm2 in adult coronary arteries to 1233 (227) in those from elderly men (p < 0.01). Data were not normally distributed in the lesions (cumulative skew of 2.04) and were therefore analysed by the Wilcoxon test.
Immunohistochemistry
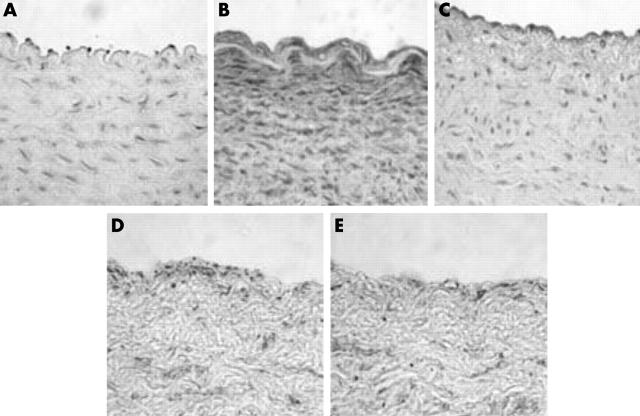
Paraffin wax embedded serial sections of coronary arteries from the study population were immunostained and assessed for the intimal presence of oxLDL, macrophage derived foam cells, and PAR-2. Sections containing at least one lesion showing positive immunostaining were counted as positive, and results were expressed as per cent of all sections of the same artery, as described previously.19–21 The early and transitional lesions (class I and II) contained significantly higher staining for PAR-2 than those of class IV (fig 1A–E). PAR-2 immunostaining was typically seen at the subendothelial space (table 1). Results obtained with both antibodies were highly correlated when all the lesions were considered (r = 0.72; p < 0.001).
Figure 1.
Representative immunostaining for protease activated receptor 2 (PAR-2; B5 antibody, 1/250 to 1/500 dilution) of human coronary arteries. (A) Control healthy tissue (oil red O negative staining) of coronary artery of an adult subject; (B) PAR-2 positive immunostaining in an early transitional coronary lesion of an adult subject; (C) faint immunostaining in the subendothelial space from a calcific coronary lesion in an elderly subject. Colocalisation in serial sections of a coronary lesion of an adult subject immunostained with (D) B5 and (E) MDA-2 antibodies. Original magnification, ×640.
Table 1.
Number of sections positive for PAR-2 staining (% of positive sections with two independent antibodies) in relation to the stage of the atherosclerotic lesions
| Stage of lesion | ||||
| Class I | Class II | Class III | Class IV | |
| PAR-2 (B2 antibody) | 56% (8%) | 69% (11%) | 43% (12%) | 25% (9%)* |
| PAR-2 (SAM11 antibody) | 43% (10%) | 58% (14%) | 46% (14%) | 28% (11%)†‡ |
We examined 72 class I and class II atherosclerotic lesions, 49 from arterial serial sections of 8 adults and 23 from arterial serial sections of 6 elderly men. Moreover, we studied 96 class III and class IV atherosclerotic lesions, 43 from arterial serial sections of 8 adults and 53 from arterial serial sections of 6 elderly men. *p<0.01 v class I and II lesions; †p<0.01 v class II lesions; ‡p<0.05 v class I lesions.
PAR-2, protease activated receptor 2.
Computer assisted imaging analysis of colocalisation (fig 1D, E) showed a positive immunohistochemical correlation between oxLDL and PAR-2 (B5 antibody) in class I and II lesions (r = 0.48 and 0.41, respectively; p < 0.01). The correlation between PAR-2 and oxLDL was also significant in class III lesions using the SAM11 antibody (r = 0.51; p < 0.01). Thus, as vascular inflammation increased the correlation between oxLDL and PAR-2 increased—the correlation between oxLDL and PAR-2 was stronger in class III lesions than in class I and II lesions. However, there were no correlations in class IV lesions (p = NS for both B5 and SAM11 antibodies), probably because multiple inflammatory pathways are simultaneously activated in such advanced atherosclerotic lesions. These immunostaining data reflected a simultaneous increase for both antibodies in the same areas and not increased numbers of nuclei in serial sections.
DISCUSSION
This is the first evidence that the PAR-2 protein is present in early coronary atherosclerotic lesions in humans without confounding risk factors for atherosclerosis. We have shown that calcific atherosclerotic lesions in coronary arteries (class IV) have reduced PAR-2 expression. The results are particularly consistent because the immunohistochemical data from the two independently prepared antisera (B5 and SAM11 antibodies) were the same.
The details of the complex framework of pathological processes leading to the formation of atherosclerotic lesions are well documented. Atherosclerosis based diseases are the leading cause of death and disability in the world. Because classic risk factors may increase per se the degree of coronary atherosclerosis and vascular inflammation, here, we selected prospectively only men who did not have the classic risk factors for the disease.19 We showed that the presence of PAR-2 protein in lesions was significantly related to oxidation specific epitopes of oxLDL (MDA-2 antibody) in class I, II, and III lesions. Clearly, the relative contribution of these potential mechanisms to atherogenesis and vascular inflammation, the functional relevance of changes in PAR-2 expression, and their interactions need to be investigated in experimental models of the disease, rather than in postmortem tissues. Although this does not represent a causal association, differences in intracellular and extracellular oxidative processes could exist in human coronary arteries, which in turn may affect PAR-2 dependent gene expression. Obviously, it is well recognised that atherogenesis is a complex inflammatory disease.18 It is therefore possible that a broad spectrum of inflammatory and oxidation sensitive genes could be activated,23,24 especially in class II and III lesions. Thus, the mechanism involving PAR-2 activation and oxidation sensitive pathways in the arterial wall could perpetuate the condition of “oxidative stress and inflammation”. We cannot establish whether increased in situ PAR-2 activity is a primary phenomenon or whether it is secondary to the atherogenic and/or inflammatory process; however, when atherogenesis affects coronary arteries, this may induce activation of PAR-2 in a vicious cycle. Further studies are also needed to establish whether the changes in protein concentrations are the result of increased gene expression or stabilisation of the protein.
Previous data also indicate that PAR-2 plays an important role in myocardial ischaemia–reperfusion injury,8,10 an inflammatory state in which a large amount of oxygen radicals are generated at reflow. This further suggests a broad spectrum of oxidation sensitive PAR-2 activities in the cardiovascular system. Thus, the PAR-2 dependent network may play a pivotal role in the inflammatory response and oxidative injury to tissue.1,2 In this context, vascular inflammation linked to atherosclerosis may represent an additional scenario for the action of PAR-2.
“We showed that the presence of protease activated receptor 2 in lesions was significantly related to oxidation specific epitopes of oxidised low density lipoprotein (MDA-2 antibody) in class I, II, and III lesions”
Previous data in other models,1,8,10,11,13 recent data on the angiogenesis promoting effects of PAR-2,25,26 and our results indicate that PAR-2 may not necessarily play a pathological role in vascular inflammation. It could reflect a more complex pathophysiological situation, where arteries try to counterbalance the vascular damage caused by atherogenesis by inducing a protective response. In line with this assumption, bacterial proteinases activate PAR-2 on neutrophils,27 suggesting that PAR-2 may constitute one of the first protective mechanisms that signal invasion of bacterial pathogens by activating a primary inflammatory response. This last consideration might also fit in with the hypothesis that infection and inflammation trigger acute coronary syndromes.18,28 Once it is established whether PAR-2 expression is a primary or a secondary response and whether this expression is harmful or just a compensatory mechanism, inducing a protective response, modulation of PAR-2 may represent a possible therapeutic target for controlling vascular response to injury.
Take home messages.
We show for the first time that protease activated receptor 2 (PAR-2) expression is enhanced in human coronary atherosclerotic lesions from humans with no classic risk factors for atherosclerosis
PAR-2 dependent cellular trafficking may be one of the regulatory signalling responses to vascular injury
Further pharmacological studies will establish whether modulation of PAR-2 represents a possible therapeutic target for controlling the vascular response to injury
Acknowledgments
Supported by PRIN 1999 and 2001 from the Ministero della Università e Ricerca Scientifica e Tecnologica, Italy, and in part by a grant (to MDH) from the Canadian Institutes of Health Research–Heart and Stroke Foundation of Canada. We thank Dr FP D’Armiento (Naples, Italy) for helpful comments on the immunohistochemical analysis.
Abbreviations
oxLDL, oxidised low density lipoprotein
PAR-2, protease activated receptor 2
PBS, phosphate buffered saline
REFERENCES
- 1.Cirino G, Napoli C, Bucci MR, et al. Inflammation–coagulation network: are serine protease receptors the knot? Trends Pharmacol Sci 2000;21:170–2. [DOI] [PubMed] [Google Scholar]
- 2.Hirano K, Kanaide H. Role of protease-activated receptors in the vascular system. J Atheroscler Thromb 2003;10:211–25. [DOI] [PubMed] [Google Scholar]
- 3.Hwa JJ, Ghibaudi L, Williams P, et al. Evidence for the presence of a proteinase-activated receptor distinct from the thrombin receptor in vascular endothelial cells. Circ Res 1996;78:581–8. [DOI] [PubMed] [Google Scholar]
- 4.Hamilton JR, Nguyen PB, Cocks TM. Atypical protease-activated receptor mediates endothelium-dependent relaxation of human coronary arteries. Circ Res 1998;82:1306–11. [DOI] [PubMed] [Google Scholar]
- 5.Molino M, Raghunath PN, Kuo A, et al. Differential expression of functional protease-activated receptor-2 (PAR-2) in human vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 1998;18:825–32. [DOI] [PubMed] [Google Scholar]
- 6.Hamilton JR, Frauman AG, Cocks TM. Increased expression of protease-activated receptor-2 (PAR2) and PAR4 in human coronary artery by inflammatory stimuli unveils endothelium-dependent relaxations to PAR2 and PAR4 agonists. Circ Res 2001;89:92–8. [DOI] [PubMed] [Google Scholar]
- 7.McLean PG, Aston D, Sarkar D, et al. Protease-activated receptor-2 activation causes EDHF-like coronary vasodilation: selective preservation in ischemia/reperfusion injury: involvement of lipoxygenase products, VR1 receptors, and C-fibers. Circ Res 2002;90:465–72. [DOI] [PubMed] [Google Scholar]
- 8.Napoli C, Cicala C, Wallace JM, et al. Protease-activated receptor-2 modulates myocardial ischemia–reperfusion injury in the rat heart. Proc Natl Acad Sci U S A 2000;97:3678–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sabri A, Muske G, Zhang H, et al. Signaling properties and functions of two distinct cardiomyocyte protease-activated receptors. Circ Res 2000;86:1054–61. [DOI] [PubMed] [Google Scholar]
- 10.Napoli C, de Nigris F, Cicala C, et al. Protease-activated receptor-2 improves efficiency of experimental ischemic preconditioning. Am J Physiol 2002;282:H2004–10. [DOI] [PubMed] [Google Scholar]
- 11.Cicala C, Pinto A, Bucci MR, et al. Protease-activated receptor-2 involvement in hypotension in normal and endotoxemic rats in vivo. Circulation 1999;99:2590–7. [DOI] [PubMed] [Google Scholar]
- 12.Damiano BP, Cheung WM, Santulli RJ, et al. Cardiovascular responses mediated by protease-activated receptor-2 (PAR-2) and thrombin receptor (PAR-1) are distinguished in mice deficient in PAR-2 or PAR-1. J Pharmacol Exp Ther 1999;288:671–8. [PubMed] [Google Scholar]
- 13.Sobey CG, Moffatt JD, Cocks TM, et al. Evidence for selective effects of chronic hypertension on cerebral artery vasodilatation to protease-activated receptor-2 activation. Stroke 1999;30:1933–41. [DOI] [PubMed] [Google Scholar]
- 14.McGuire JJ, Dai J, Andrade-Gordon P, et al. Proteinase-activated receptor-2 (PAR2): vascular effects of a PAR2-derived activating peptide via a receptor different than PAR2. J Pharmacol Exp Ther 2002;303:985–92. [DOI] [PubMed] [Google Scholar]
- 15.Nystedt S, Ramakrishnan V, Sundelin J. The proteinase-activated receptor 2 is induced by inflammatory mediators in human endothelial cells. Comparison with the thrombin receptor. J Biol Chem 1996;271:14910–15. [DOI] [PubMed] [Google Scholar]
- 16.Kawabata A, Kuroda R, Minami T, et al. Increased vascular permeability by a specific agonist of protease-activated receptor-2 in rat hindpaw. Br J Pharmacol 1998;125:419–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vergnolle N, Hollenberg, MD, Sharkey KA, et al. Characterization of the inflammatory response to proteinase-activated receptor-2 (PAR2)-activating peptides in the rat paw. Br J Pharmacol 1999;127:1083–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ross R. Atherosclerosis—an inflammatory disease. N Engl J Med 1999;340:115–26. [DOI] [PubMed] [Google Scholar]
- 19.D’Armiento FP, Bianchi A, de Nigris F, et al. Age-related effects on atherogenesis and scavenger enzymes of intracranial and extracranial arteries in men without classical risk factors for atherosclerosis. Stroke 2001;32:2472–80. [DOI] [PubMed] [Google Scholar]
- 20.Napoli C, D’Armiento FP, Mancini FP, et al. Fatty streak formation occurs in human foetal aortas and is greatly enhanced by maternal hypercholesterolemia. Intimal accumulation of LDL and its oxidation precede monocyte recruitment into early atherosclerotic lesions. J Clin Invest 1997;100:2680–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Napoli C, Glass CK, Witztum JL, et al. Influence of maternal hypercholesterolemia during pregnancy on progression of early atherosclerotic lesions in childhood: fate of early lesions in children (FELIC) study. Lancet 1999;354:1234–41. [DOI] [PubMed] [Google Scholar]
- 22.Al-Ani B, Saifeddine M, Kawabata A, et al. Proteinase-activated receptor 2 (PAR(2)): development of a ligand-binding assay correlating with activation of PAR(2) by PAR(1)- and PAR(2)-derived peptide ligands. J Pharmacol Exp Ther 1999;290:753–60. [PubMed] [Google Scholar]
- 23.Napoli C, de Nigris F, Palinski W. Multiple role of reactive oxygen species in the arterial wall. J Cell Biochem 2001;82:674–82. [DOI] [PubMed] [Google Scholar]
- 24.de Nigris F, Lerman A, Ignarro LJ, et al. Oxidation-sensitive mechanisms, vascular apoptosis and atherosclerosis. Trends Mol Med 2003;9:351–9. [DOI] [PubMed] [Google Scholar]
- 25.Milia AF, Salis MB, Stacca T, et al. Protease-activated receptor-2 stimulates angiogenesis and accelerates hemodynamic recovery in a mouse model of hindlimb ischemia. Circ Res 2002;91:346–52. [DOI] [PubMed] [Google Scholar]
- 26.Jin E, Fujiwara M, Pan X, et al. Protease-activated receptor (PAR)-1 and PAR-2 participate in the cell growth of alveolar capillary endothelium in primary lung adenocarcinomas. Cancer 2003;97:703–13. [DOI] [PubMed] [Google Scholar]
- 27.Lourbakos A, Chinni C, Thomson P, et al. Cleavage and activation of proteinase-activated receptor-2 on human neutrophils by gingipain-R from Porphyromonas gingivalis. FEBS Lett 1998;232:84–89. [DOI] [PubMed] [Google Scholar]
- 28.Danesh J, Collins R, Peto R. Chronic infections and coronary heart disease: is there a link? Lancet 1997;350:430–6. [DOI] [PubMed] [Google Scholar]