An association between ampullary adenoma and adenocarcinoma has been reported previously.1 However, we believe that this is the first report of the synchronous occurrence of adenocarcinoma of the ampulla of Vater and a gastrointestinal stromal tumour (GIST).
A 41 year old woman was admitted to our hospital for the evaluation of jaundice. Her liver function tests were as follows: alanine aminotransferase, 37 U/litre (normal range, 0–31); aspartate aminotransferase, 32 U/litre (normal range, 0–32); alkaline phosphatase, 598 U/litre (normal range, 0–240); total bilirubin, 203.2 mg/litre (normal range, 1–11); direct biluribin, 151.6 mg/litre (normal range, 0–3).
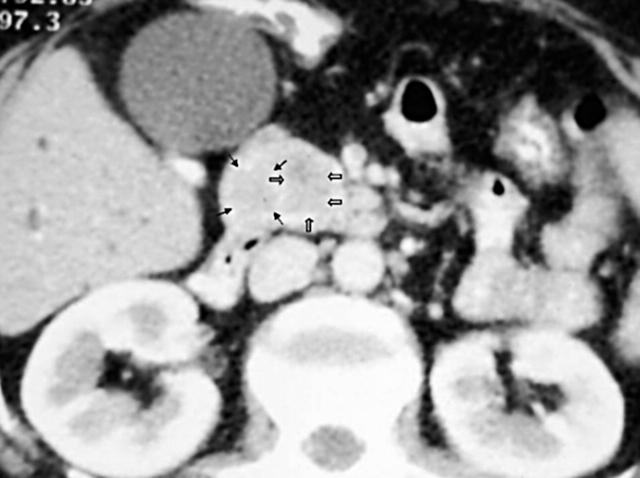
Ultrasonography, computed tomography, and magnetic resonance imaging studies showed intrahepatic and extrahepatic bile duct dilatation. Termination of the common bile duct at the distal end by a mass was noted (fig 1). The initial radiological differential diagnosis included pancreatic head tumour and periampullary carcinoma.
Figure 1.
Computed tomography (CT) showed a solid mass, located inferiorly to the pancreatic head and uncinate process. The mass enhanced similarly with pancreatic parenchyma at the early arterial phase. Preoperatively, the mass was interpreted as being located in the pancreatic head. CT images were evaluated retrospectively with the findings at surgery and two different lesions were differentiated (arrows).
Endoscopic procedures were not performed before surgery. Pancreaticoduodenectomy, cholecystectomy, and distal gastrectomy with lymph node dissection were performed.
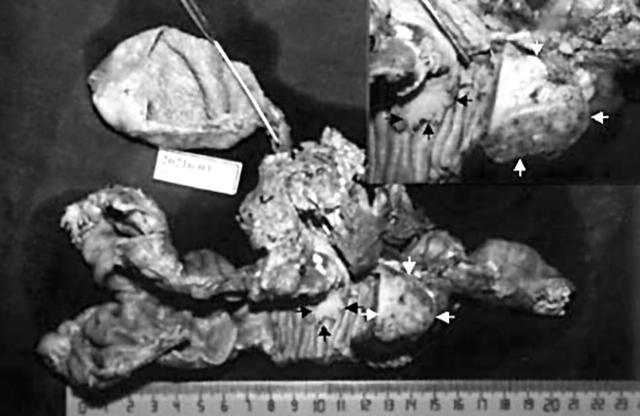
Grossly, there was a polypoid tumour (1.5 × 1.5 × 1 cm) at the duodenal ampulla with a solid subserosal tumour (3 × 3 × 2 cm) in the second portion of the duodenum (fig 2). On cut section, there was no transition between these two different tumours and no invasion of surrounding tissues and pancreas.
Figure 2.
Grossly, a polypoid tumour is located at the duodenal ampulla (black arrows) and an another solid subserosal tumour is seen in the second portion of the duodenum (white arrows).
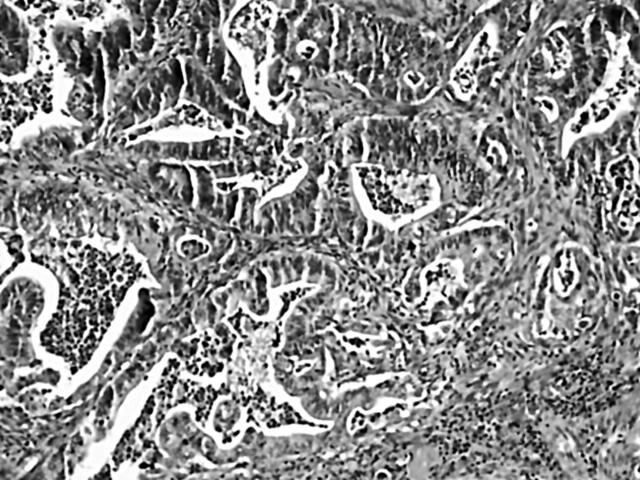
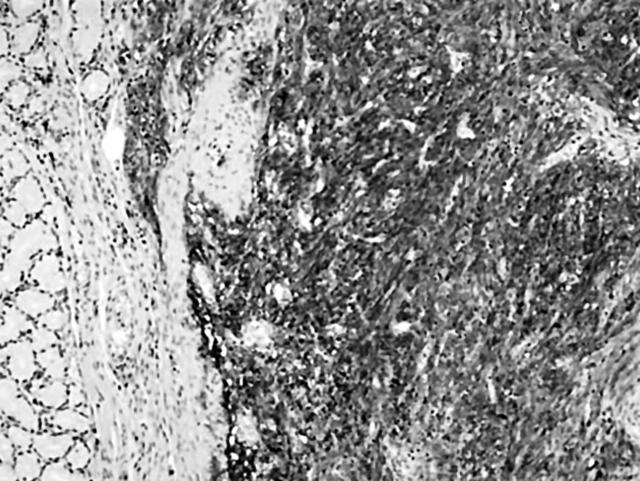
Histologically, the tumours showed a moderately differentiated adenocarcinoma associated with a villous adenoma, which was limited to the ampulla of Vater and a GIST (figs 3 and 4). The GIST was sharply demarcated from the surrounding tissue and it was mainly located at the serosa and muscular layers. Cytologically, the tumour cells had spindle shaped, blunt ended or oval nuclei, with evenly distributed chromatin and moderate pleomorphism; the cells exhibited a fascicular or storiform growth pattern, and had invaded the submocosal layer. Nine atypical mitotic figures for each 10 high power fields (HPF) were present. Immunohistochemically, the tumour cells of the GIST showed diffuse and strong positive immunoreactivity against CD117 (T595; 1/20 dilution; Novacastra, Newcastle, UK), CD34 (QBEND/10; 1/50 dilution, Dako, Glostrup, Denmark).
Figure 3.
Histological examination of the ampullary tumour revealed moderately differentiated adenocarcinoma; haematoxylin and eosin stain; original magnification, ×100.
Figure 4.
Tumour cells showed a diffuse and strong positive immunoreaction for CD117 in the gastrointestinal stromal tumour; original magnification, ×100.
Stromal tumours involving the small intestine are far less common but seem to have greater malignant potential.2 The expression of CD117 has emerged as the most important defining feature and probably the gold standard for diagnosing GISTs.2 High mitotic index (more than five mitoses/10 HPF) and larger tumour size (> 5 cm) are generally accepted as the best indicators of malignancy in GIST.2 Despite the small size of the tumour, nine atypical mitotic figures/10 HPF, submucosal invasion, and mild pleomorphism of the tumour cells were present in our case.
The possible cause of multiple malignancies include: reduced immunological competence, constitution, genetic factors, chemotherapy, radiation exposure, surgery, or smoking.3 In our patient, a family history of malignancy and other risk factors were not present. It can also be hypothesised that the duodenum was influenced by the same unknown carcinogen, resulting in a simultaneous proliferation of different cell lines (epithelial and stromal cells).4
The literature includes case reports of gastric collision tumour composed of GIST intermixed with adenocarcinoma, synchronously occurring GIST and carcinoid tumour, GIST and lipoma, and GIST and mucosa associated lymphoid tissue lymphoma.4,5 To our knowledge, our case is the first report of the synchronous occurrence of adenocarcinoma of the ampulla of Vater with a GIST.
References
- 1.Qizilbash AH. Duodenal and peri-ampullary adenomas. Curr Top Pathol 1990;81:77–90. [DOI] [PubMed] [Google Scholar]
- 2.de Silva CM, Reid R. Gastrointestinal stromal tumors (GIST): C-kit mutations, CD117 expression, differential diagnosis and targeted cancer therapy with Imatinib. Pathol Oncol Res 2003;9:13–19. [DOI] [PubMed] [Google Scholar]
- 3.Nakayama H , Masuda H, Ugajin W, et al. Quadruple cancer including bilateral breasts, Vater’s papilla, and urinary bladder: report of a case. Surg Today 1999;29:276–9. [DOI] [PubMed] [Google Scholar]
- 4.Liu SW, Chen GH, Hsieh PP. Collision tumor of the stomach: a case report of mixed gastrointestinal stromal tumor and adenocarcinoma. J Clin Gastroenterol 2002;35:332–4. [DOI] [PubMed] [Google Scholar]
- 5.Al-Brahim N , Radhi J, Gately J. Synchronous epithelioid stromal tumour and lipoma in the stomach. Can J Gastroenterol 2003;17:374–5. [DOI] [PubMed] [Google Scholar]