Abstract
Rhodococcus equi, a Gram positive organism, is a cause of infections in immunocompromised individuals. In humans, it mainly causes disease in those infected with human immunodeficiency virus (HIV), and generally presents as chronic pulmonary infection. It may also cause intracranial infections, which manifest as brain abscesses. This report describes a case of rhodococcus brain and pulmonary infection in a patient who did not have HIV or another disorder of cell mediated immunity. He was treated with intravenous imipenem, vancomycin, and rifampin for eight weeks and recovered from the infection.
Keywords: Rhodococcus equi, brain abscess, pneumonia
The aerobic Gram positive coccobacillus, Rhodococcus equi, is a well known cause of disease in animals. Human disease predominantly occurs in individuals with human immunodeficiency virus (HIV), or other immunocompromised states. There have been rare reports of brain abscesses caused by R equi in patients without HIV who have been immunocompromised as a result of chemotherapy.1–5 We report a case of Rhodococcus equi brain and lung abscesses in an HIV negative individual.
CASE REPORT
A 43 year old man with a history of chronic hepatitis C and alcohol abuse was admitted to the hospital with a five day history of haemoptysis and shortness of breath. He had no recent history of hospitalisation, fever with rigor, tuberculosis, or HIV exposure. He also denied contact with sick individuals, contact with animals, or recent travel. He had a history of heavy alcohol intake and a splenectomy after a motor vehicle trauma in the remote past.
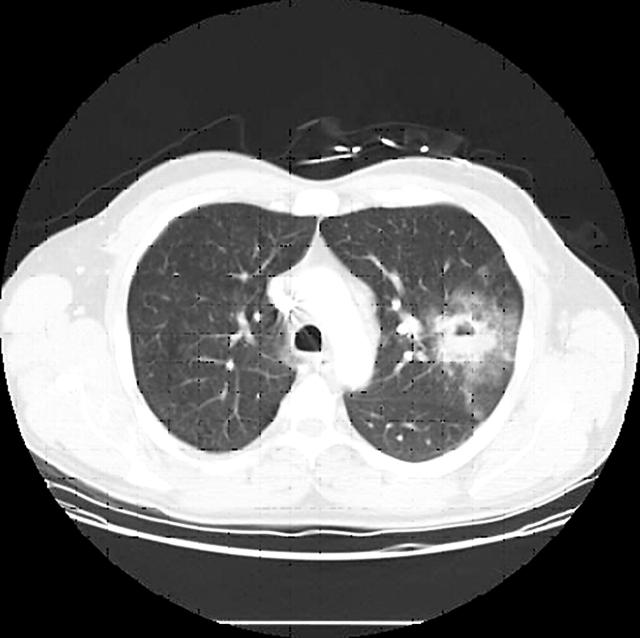
On initial examination he had a fever of 100°F, although his other vital signs were normal. His physical examination revealed mild bronchial breath sounds on the left upper lung field. The initial laboratory findings revealed his total white blood cell count to be 32.4 × 109/litre. A hepatic screen revealed raised liver enzymes (aspartate aminotransferase, 155 U/litre; alanine aminotransferase, 110 U/litre; and alkaline phosphatase, 134 U/litre). His chest x ray was suggestive of left upper lung field opacification. An empirical antibiotic regimen including ceftriaxone 2 g daily, levofloxacin 500 mg daily, and metronidazole 500 mg every eight hours was started and blood cultures, urine analysis, and sputum studies including acid fast bacillus stains and cultures were obtained; these were initially negative. A serological HIV test obtained after informed consent was negative. Subsequent radiological investigations (computer assisted tomography scan of lungs) revealed a cavity in the left upper lobe of the lung (fig 1). A bronchoscopic examination was performed and routine cultures obtained during the test were negative for mycobacterial, fungal, and bacterial pathogens. The patient subsequently became delirious and a magnetic resonance imaging scan of the brain was obtained, which showed four ring enhancing lesions in the cerebral cortex (fig 2). A neurosurgical consultation was obtained for a possible brain biopsy and the empirical antibiotic regimen was discontinued before the brain biopsy because of worsening liver function. A neurosurgical aspirate of one of the lesions in the parietal cortex revealed creamy pus on gross examination, with the Gram stain showing more than 100 white blood cells in each high power field, but no organisms. The routine cultures of the aspirate were also negative, as was an HIV test. A set of blood cultures was repeated because the patient developed fever and still had a persistently raised total leucocyte count. The blood samples were cultured aerobically and anaerobically by means of the BACTEC method, and there was a single positive blood culture, which was Gram stained and subcultured on blood agar. The blood agar plate showed large mucoid colonies with characteristic salmon pink pigmentation. The API Cornye system (Biomérieux, Marcy-L’Etoile, France) was used to characterise the Gram positive, coccoid, catalase positive organism, which was found to be R equi. The susceptibility of the organism to several antibiotics was checked using the E-test (AB Biodisk, Solna, Sweden), and the results are shown in table 1. The patient was treated with intravenous rifampin, imipenem, and vancomycin for eight weeks. The patient improved on the antibiotics: his chest x ray showed resolution of the cavitary lesion and there was also a decrease in the size of the ring enhancing lesions on follow up MRI performed three months later.
Figure 1.
Computer assisted tomography scan of the lung showing a cavity in the left upper lobe of the lung.
Figure 2.

Magnetic resonance imaging scan of the brain showing four ring enhancing lesions in the cerebral cortex.
Table 1.
Minimum inhibitory concentration (MIC) of the isolate to the antibiotics tested
| Antibiotic | MIC (μg/ml) |
| Imipenem | 0.064 |
| Ciprofloxacin | 0.032 |
| Ceftriaxone | 0.38 |
| Vancomycin | 0.38 |
| Clindamycin | 1.5 |
| Trimethoprim-sulfamethoxazole | 0.047 |
| Tetracycline | 0.125 |
DISCUSSION
Rhodococcus equi is an aerobic, pleomorphic coccobacillus, which predominantly causes infection in patients with HIV and other immunosuppressed conditions, with more than 200 reported cases.6,7 This organism is a facultative intracellular pathogen that infects macrophages and survives intracellularly because of its ability to resist the oxidative burst and prevent phagosome–lysosome fusion. This enables it to survive the lethal effects of antibiotics and cause chronic and relapsing infections. It is found in soil and is a well known cause of infection in animals, particularly foals, swine, horses, sheep, calves, and goats. Exposure to these animals is often found in patients with rhodococcus infection. Infection is acquired via the airborne route and is extremely rare in immunocompetent individuals.8 The lung is usually the primary site of infection, resulting in necrotising pneumonia, with subsequent haematogenous dissemination, most commonly to the brain. The initial infection in the lung manifests as a cavitary lesion, followed by consolidation, pleural effusion, and rarely mediastinal enlargement and pulmonary nodules. Other tissue infections that have been described include gastrointestinal infections, pericarditis, meningitis, mastoiditis, and abscesses in the liver, kidney, and psoas muscles. To our knowledge, there are 11 reported cases of R equi brain abscesses, and most were in patients with HIV, patients with haematological malignancies, and renal transplant recipients.1–5,9,10 Only two cases have been described in immunocompetent individuals.9,10
“Both the duration and the route of treatment should be adjusted based on the clinical and radiological response to treatment”
There are limited data and no clear guidelines for the treatment of infections caused by R equi. The organism is consistently sensitive to vancomycin, erythromycin, aminoglycosides, rifampin, and imipenem and resistant to the penicillins and cephalosporins.11 The choice and duration of antibiotics are very important to prevent therapeutic failure. Because an adequate concentration of the antibiotic must be achieved intracellularly, it is recommended that a combination of at least two antibiotics should be used for a two to six month period. A proposed approach for the treatment of R equi infections suggests that local infections in immunocompetent hosts should be treated by a combination of two oral antibiotics, using drugs such as erythromycin, rifampin, and/or a quinolone.12 It is also suggested that more serious infections, including those in immunocompromised hosts, should initially be treated intravenously using a combination of two to three drugs such as vancomycin, imipenem, aminoglycosides, rifampin, ciprofloxacin, and or erythromycin. The authors suggest that both the duration and the route of treatment should be adjusted based on the clinical and radiological response to treatment.
Our case report describes a man with impaired immune status secondary to liver disease and a splenectomy who acquired R equi lung infection leading to abscess formation and subsequent bacteraemia with seeding to the brain. We believe it emphasises the role of this bacterium in causing the combined lung–brain abscess syndrome. Individuals who present with cavitary lung lesions and brain abscesses should be screened for R equi.
Take home messages.
We describe a man with impaired immune status as a result of liver disease and splenectomy who acquired Rhodococcus equi lung infection, which led to abscess formation and subsequent bacteraemia, with seeding to the brain
This case emphasises the role of this bacterium in the combined lung–brain abscess syndrome
Individuals who present with cavitary lung lesions and brain abscesses should be screened for R equi
The patient gave his consent for the case to be published.
REFERENCES
- 1.Crone P, Rajeebally I, Jonquet O. Rhodococcus equi brain abscess in an immunocompetent patient. Scand J Infect Dis 2002;34:300–2. [DOI] [PubMed] [Google Scholar]
- 2.Kohl O, Tillmanns HH. Cerebral infection with Rhodococcus equi in a heart transplant recipient. J Heart Lung Transplant 2002;21:1147–9. [DOI] [PubMed] [Google Scholar]
- 3.Akan H, Akova M, Ataoglu H, et al. Rhodococcus equi and Nocardia brasiliensis infection of the brain and liver in a patient with acute nonlymphoblastic leukemia. Eur J Clin Microbiol Infect Dis 1998;17:737–9. [DOI] [PubMed] [Google Scholar]
- 4.Obana WG, Scannell KA, Jacobs R, et al. A case of Rhodococcus equi brain abscess. Surg Neurol 1991;35:321–4. [DOI] [PubMed] [Google Scholar]
- 5.Hsueh PR, Hung CC, Teng LJ, et al. Report of invasive Rhodococcus equi infections in Taiwan, with an emphasis on the emergence of multidrug-resistant strains. Clin Infect Dis 1998;27:370–5. [DOI] [PubMed] [Google Scholar]
- 6.Flepp M, Luthy R, Wust J, et al. Rhodococcus equi infection in HIV disease. Schweiz Med Wochenschr 1989;119:566–74. [PubMed] [Google Scholar]
- 7.Cohen WA. Intracranial bacterial infections in patients with AIDS. Neuroimaging Clin N Am 1997;7:223–9. [PubMed] [Google Scholar]
- 8.Kedlaya I, Ing MB, Wong SS. Rhodococcus equi infections in immunocompetent hosts: case report and review. Clin Infect Dis 2001;32:E39–46 Epub 2001 Jan 24. [DOI] [PubMed] [Google Scholar]
- 9.Blanco J, Yebra M, Munoz R, et al. Cerebral abscess caused by Rhodococcus equi in an immunocompetent patient. Enferm Infecc Microbiol Clin 1998;16:294–5. [PubMed] [Google Scholar]
- 10.Martin MP, Moragrega B, Garcia M, et al. [Rhodococcus equi brain abscess in a patient in hemodialysis.] Nefrologia 2000;20:387–8. [PubMed] [Google Scholar]
- 11.Moretti F, Quiros-Roldan E, Casari S, et al. Rhodococcus equi: pulmonary cavitation lesion in patient infected with HIV cured by levofloxacin and rifampicin. AIDS 2002;16:1440–2. [DOI] [PubMed] [Google Scholar]
- 12.Weinstock DM, Brown AE. Rhodococcus equi: AN emerging pathogen. Clin Infect Dis 2002;34:1379–85. [DOI] [PubMed] [Google Scholar]