Abstract
Angiomyolipomas are rare lesions, often arising in the kidney, and are part of a group of tumours with a diverse appearance and evidence of dual melanocytic and smooth muscle differentiation known as PEComas (tumours of perivascular epithelioid cell origin). This report describes an unusual case of a colonic PEComa in a 40 year old woman. Unlike most of the previous colonic angiomyolipomas/PEComas reported in the literature, this case formed a large, mainly extrinsic mass and was monotypic, and composed entirely of the myomatous component with no adipose tissue or typical vasculature.
Keywords: colon, PEComa, angiomyolipoma, epithelioid, HMB-45
Angiomyolipoma is an uncommon, usually benign, renal tumour showing a characteristic histological triad of adipose tissue, vessels, and modified smooth muscle with immunohistochemical and ultrastructural evidence of dual melanocytic and smooth muscle differentiation. The tumour may be found sporadically or in association with tuberous sclerosis, an autosomal dominantly inherited disorder, characterised by mental retardation, epilepsy, and adenoma sebaceum.1 Recently, similar tumours at other sites have been shown to have a similar origin.
We present the case of a 40 year old woman with a PEComa (tumour of perivascular epithelioid cell (PEC) origin) of the colon without evidence of tuberous sclerosis. Unlike the previous colonic PEComas/angiomyolipomas reported, this case formed a large, mainly extrinsic mass and was monotypic, composed entirely of the myomatous component with no adipose tissue or typical vasculature.
CASE REPORT
A 40 year old woman was admitted to University Hospital, Nottingham, UK with a history of abdominal bloating and constipation for one year. Her family history and past medical history were unremarkable. Colonoscopy revealed a large extraluminal mass in the medial wall of the caecum. There were no mucosal abnormalities. At laparotomy a large mobile mass arising from the medial caecal wall was removed.
The right hemicolectomy specimen contained a mass arising in the caecum measuring 80 × 60 × 90 mm. This was predominantly extrinsic but formed a polypoid protrusion into the caecum. The tumour had a solid, haemorrhagic cut surface with areas of necrosis. It had a lobulated outline lined by peritoneum (fig 1A).
Figure 1.

(A) The tumour was large and mainly extrinsic with extensive areas of haemorrhage and necrosis. (B) A spindled area within the submucosa invading the overlying colonic mucosa (arrow). (C) Epithelioid area with large atypical cells. (D) A strap-like atypical epithelioid cell with an arrow indicating rhomboid crystals within the cytoplasm.
Histologically, the tumour was composed of distinct spindled and epithelioid cellular populations (fig 1B–D). The spindled area was arranged in fascicles with cigar shaped nuclei in the submucosa and focally invaded the overlying mucosa. The epithelioid area was more extensive and showed cells with abundant dense eosinophilic and granular cytoplasm, with some showing cytoplasmic clearing. Some cells showed eosinophilic nuclear inclusions, whereas others had a strap-like morphology. There was pronounced nuclear pleomorphism, with some cells showing large nucleoli mimicking ganglion cells. The mitotic rate was three/50 high power fields. The tumour showed small vessels but not the typical vessels of classic angiomyolipoma. Despite extensive sampling, no adipose tissue was present. Immunocytochemistry showed strong positivity for HMB45 in both components (fig 2A, B). Staining for smooth muscle actin and desmin was positive in the spindled areas, with focal positivity in the epithelioid component. Staining for cytokeratins, CD31, calretinin, α fetoprotein, and S100 was negative in both components. Staining for CD117, melan A, and CD34 was focally and weakly positive. Electron microscopy showed occasional rhomboid crystals (fig 2D) and numerous small cytoplasmic vesicles (fig 2C), not recognisable as premelanosomes.
Figure 2.
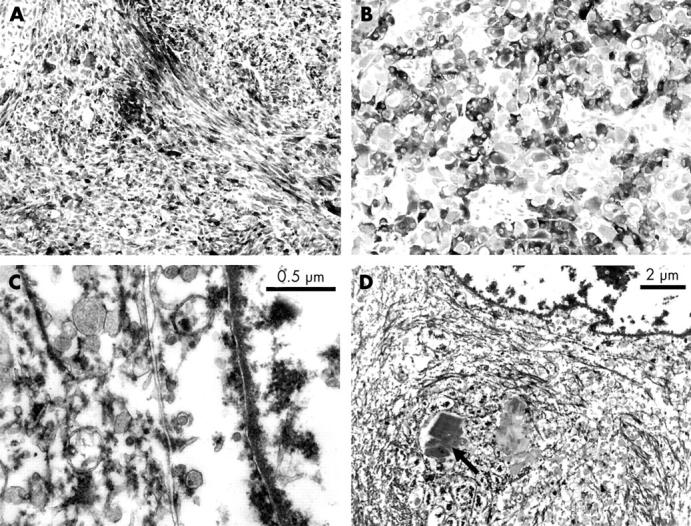
(A) Strong positive staining for HMB45 in the spindled areas. (B) Strong positive staining for HMB45 in the epithelioid areas. (C) Electron microscopy image showing the cytoplasmic vesicles. (D) Electron microscopy image showing the rhomboid crystals (arrow).
DISCUSSION
Angiomyolipoma is a distinctive neoplasm, typically arising in the kidney and characterised by a combination of adipose tissue, abnormal blood vessels, and smooth muscle. It is believed to arise from the putative perivascular epithelioid cell (PEC), which may give rise to a variety of tumours and proliferations such as angiomyolipoma, lymphangiomyoma, lymphangiomyomatosis, clear cell myomelanocytic tumour of the falciform ligament/ligamentum teres, and pulmonary clear cell “sugar” tumour.2 PEComas are characterised by evidence of dual melanocytic and smooth muscle differentiation, both at the immunohistochemical and the ultrastructural level. Typically, there is strong immunoreactivity with the HMB45 antibody and variable expression of muscle markers.
“Angiomyolipoma/PEComa may be a challenging diagnosis to make when it arises outside its typical renal location because of its rarity and the histological variation”
Angiomyolipoma/PEComa may be a challenging diagnosis to make when it arises outside its typical renal location because of its rarity and the histological variation. Typically, angiomyolipoma shows a mixture of adipose tissue, fat, and abnormal vessels, but it may show a wide range of histological appearances. These include tumours where the muscle component is dominant, including epithelioid variants and those showing considerable nuclear atypia.
Gastrointestinal involvement is rare, with only seven previous cases reported in the colon and one each in the duodenum, stomach, and appendix.3–9 The previously reported cases were small (1–3 cm) polypoid tumours, mainly of classic histological type. Only one previous case,9 a 3 cm lesion in the caecum, was entirely epithelioid myomatous but without necrosis. Another 1 cm lesion in the appendix showed an epithelioid and typical vascular component without fat.9 Thus, our present case is the second reported case in the gastrointestinal tract to consist entirely of the myomatous component, and is also the largest example reported in the gastrointestinal tract.
The combination of a rare tumour at an unusual site with an atypical histological appearance presents diagnostic challenges. Our differential diagnosis included gastrointestinal stromal tumour, leiomyosarcoma, melanoma, and extrarenal rhabdoid tumour. Although gastrointestinal stromal tumour may contain epithelioid areas they are rarely as pleomorphic as in this case. The weak staining with CD117 and the strong positivity for HMB45 precluded this diagnosis. Epithelioid leiomyosarcoma was probably the most important differential diagnosis to consider. Like this tumour, it can present a combination of spindled and epithelioid morphology and may be very pleomorphic. HMB45 positivity has been described in the clear cell component of uterine epithelioid leiomyosarcomas,10 although these rare tumours may also represent part of the PEComa spectrum. In our case, HMB45 was strongly positive throughout the tumour in spindled and epithelioid areas; this has not been described in leiomyosarcoma. Melanoma was excluded because of lack of staining for S100, whereas rhabdoid tumour was unlikely given the lack of positivity for keratins and minimal positivity for desmin in the epithelioid area, HMB45 positivity, and absence of typical ultrastructural features.
Take home messages.
We describe an unusual case of colonic PEComa (tumour of perivascular epithelioid cell origin) that we believe is the largest so far reported in the gastrointestinal tract
This tumour is also the first of its type to show morphological evidence to suggest potential malignant behaviour
The combination of a rare tumour at an unusual site with an atypical histological appearance presented a diagnostic challenge in this case
Although classic renal angiomyolipomas were regarded as universally benign lesions it is becoming increasingly clear that PEComas should be regarded as tumours of uncertain malignant potential.11–13 Tumours with a poor outcome are usually monotypic myomatous variants, especially those with dominant pleomorphic epithelioid components. Other factors likely to portend poor outcome include presence of haemorrhage and necrosis, local invasiveness, and high mitotic activity. The case presented here had a monotypic appearance with a prominence of epithelioid features, areas of haemorrhage and necrosis, and mucosal invasion, all features that are regarded as potentially malignant. However, to date, the patient remains well with no evidence of recurrence or metastasis.
In summary, we have presented a case of colonic PEComa, which we believe to be the largest so far reported in the gastrointestinal tract and the first to show morphological evidence to suggest potential malignant behaviour.
Acknowledgments
We thank Mr T Gray for the electron microphotography and Ms A Kane for her assistance in photography.
Abbreviations
PEC, perivascular epithelioid cell
The patient gave her full consent for this case report to be published
REFERENCES
- 1.Tong YC, Chieng PU, Tsai TC, et al. Renal angiomyolipoma: report of 24 cases. Br J Urol 1990;66:585–9. [DOI] [PubMed] [Google Scholar]
- 2.Govender D, Sabaratnam RM, Essa AS. Clear cell “sugar” tumour of the breast: another extrapulmonary site and review of the literature. Am J Surg Pathol 2002;26:670–5. [DOI] [PubMed] [Google Scholar]
- 3.Maluf H, Dieckgraefe B. Angiomyolipoma of the large intestine: report of a case. Mod Pathol 1999;12:1132–6. [PubMed] [Google Scholar]
- 4.Pelz J, Weber K, Gohl J, et al. Angiomyolipoma of the colon—case report and review of the literature. Z Gastroenterol 2003;41:715–18. [DOI] [PubMed] [Google Scholar]
- 5.Chen JS, Kuo LJ, Lin PY, et al. Angiomyolipoma of the colon: report of a case and review of the literature. Dis Colon Rectum 2003;46:547–9. [DOI] [PubMed] [Google Scholar]
- 6.Maesawa C, Tamura G, Sawada H, et al. Angiomyolipoma arising in the colon. Am J Gastroenterol 1996;91:1852–4. [PubMed] [Google Scholar]
- 7.Verzaro R, Guadagni S, Agnifili A, et al. A case of extrarenal angiomyolipoma with intestinal localization. Minerva Chir 1992;47:1317–19. [PubMed] [Google Scholar]
- 8.Hikasa Y, Narabayashi T, Yamamura M, et al. Angiomyolipoma of the colon: a new entity in colonic polypoid lesions. Gastroenterol Jpn 1989;24:407–9. [DOI] [PubMed] [Google Scholar]
- 9.Prasad ML, Keating JP, Heng Teoh H, et al. Pleomorphic angiomyolipoma of digestive tract: a heretofore unrecognised entity. Int J Surg Pathol 2000;8:67–72. [DOI] [PubMed] [Google Scholar]
- 10.Silva EG, Deavers MT, Bodurka DC, et al. Uterine epithelioid leiomyosarcomas with clear cells: reactivity with HMB-45 and the concept of PEComa. Am J Surg Pathol 2004;28:244–9. [DOI] [PubMed] [Google Scholar]
- 11.Bonetti F, Martignoni G, Colato C, et al. Abdominopelvic sarcoma of perivascular epithelioid cells. Report of four cases in young women, one with tuberous sclerosis. Mod Pathol 2001;14:563–8. [DOI] [PubMed] [Google Scholar]
- 12.Takahashi N, Kitahara R, Hishimoto Y, et al. Malignant transformation of renal angiomyolipoma. Int J Urol 2003;10:271–3. [DOI] [PubMed] [Google Scholar]
- 13.Martignoni G, Pea M, Rigaud G, et al. Renal angiomyolipoma with epithelioid sarcomatous transformation and metastases: demonstration of the same genetic defects in the primary and metastatic lesions. Am J Surg Pathol 2000;24:889–94. [DOI] [PubMed] [Google Scholar]


