Abstract
This case report describes for the first time a case of pure testicular carcinoid preaortic lymph node metastases in a 25 year old patient with carcinoid syndrome. The simultaneous occurrence of intratubular germ cell neoplasia in the surrounding testicular tissue was identified by OCT4 and placental-like alkaline phosphatase positivity. This confirmed that the tumour had a germ cell origin in the testis, rather than being a metastasis from an extragenital carcinoid.
Keywords: testis, carcinoid, intratubular germ cell neoplasia, carcinoma in situ
About 90 cases of carcinoid tumour of the testis have been reported to date.1,2 Histologically, most correspond to pure patterns and a few occur as a component of testicular teratoma. From a diagnostic viewpoint, it is important to differentiate primary testicular carcinoids from either metastases from extragenital carcinoids3 or testicular neoplasms of non-germ cell origin resembling carcinoids, such as granulosa cell tumours.
We report, for the first time, a case of pure testicular carcinoid with lymph node metastases and carcinoid syndrome. In this tumour, the concomitant presence of intratubular germ cell neoplasia (ITGCN) in the surrounding testicular tissue helped to identify its germ cell origin in the testis and to eliminate the possibility of a metastasis from an extragenital carcinoid.
CASE REPORT
A 25 year old patient presented with dull scrotal pain. He had had a mass in the left testis since childhood, and since adolescence had experienced bouts of watery diarrhoea and flushing episodes, considered allergic in nature by his family practitioner.
Physical examination revealed a hard left testicular mass, which ultrasound showed to be a solid, nodular, heterogeneous lesion with isolated irregular calcifications. Both α fetoprotein and β human chorionic gonadotrophin concentrations were within normal limits. A left orchidectomy was performed. After a histopathological diagnosis of pure testicular carcinoid, we measured 5-hydroxyindole acetic acid concentrations and found them to be raised at 330 ng/ml. Both diarrhoea and flushing were reduced after surgery. The presence of a carcinoid tumour elsewhere was initially discarded by full body scintigraphy with 111In-octreotide. However, 11 months later an abdominal computerised tomography scan revealed preaortic lymph node involvement, confirmed surgically by the finding of masses at lymphadenectomy. However, 5-hydroxyindole acetic acid concentrations remained within normal limits. Surgical inspection of intestine and liver failed to demonstrate a mass. The caecal appendix was unremarkable. The patient is presently alive and symptom free.
PATHOLOGY
The left testis contained a 6 × 5.5 × 4.5 cm, white/yellow, hard, nodular tumour with only a thin rim of testicular tissue. No gross involvement of the tunica albuginea or adnexa was evident. Sampling comprised a total of 15 tissue blocks. Microscopically, the tumour was an insular-type carcinoid arranged in nests and acini separated by broad collagenous tracts (fig 1A). Coagulative necrosis was present in the central area. Cells were regular and homogeneous, lacking atypia or mitoses, but there were microscopic foci of capsular and adnexal invasion. Immunohistochemistry revealed pronounced cytoplasmic positivity to synaptophysin and chromogranin (fig 1B); placental-like alkaline phosphatase (PLAP) was negative in the carcinoid areas. Intratubular extension of carcinoid was not detected. The surrounding testicular parenchyma was reduced to an atrophic band revealing widespread foci of ITGCN, both at a distance and in the vicinity of the carcinoid (fig 2A), showing cells with irregular nuclei and prominent nucleoli, (fig 2B) some displaying mitoses. Immunohistochemically, they revealed membranous PLAP positivity (fig 3A), but they were synaptophysin and chromogranin negative. OCT4 (Santa Cruz Biotechnology, Santa Cruz, California, USA), a novel marker for ITGCN,4 was positive in some, but not all, of the atypical germ cell nuclei of the ITGCN of neighbouring and distant tubules (fig 3B).
Figure 1.
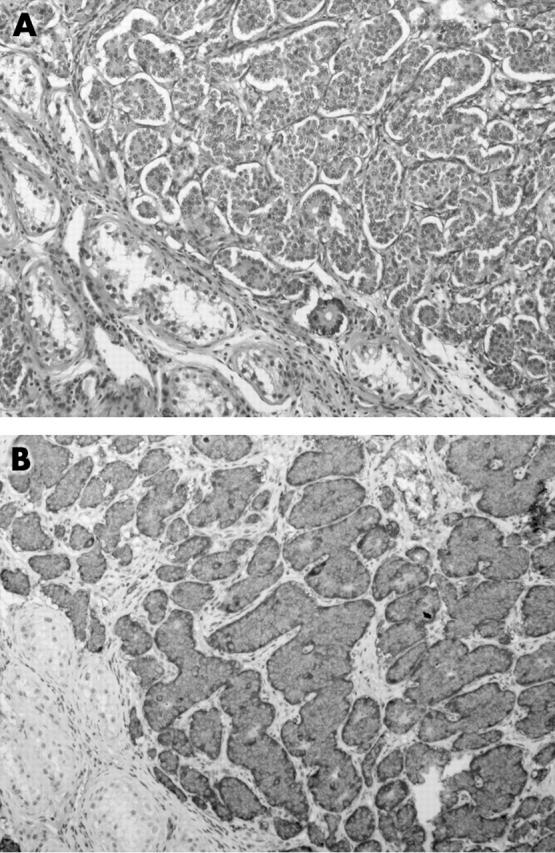
(A) Characteristic nests of insular type of carcinoid are (B) positive for chromogranin.
Figure 2.
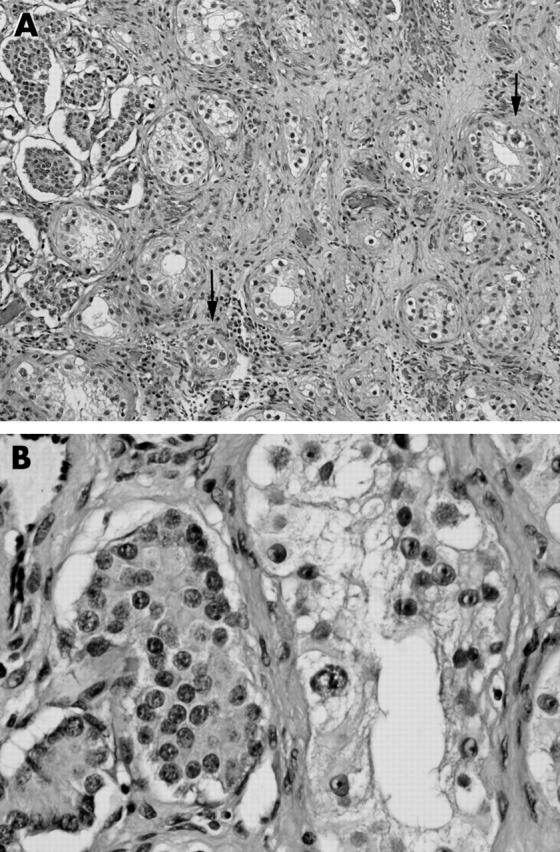
(A) Intratubular germ cell neoplasia areas are present at the interface with carcinoid (arrows). (B) Higher magnification showing large atypical nuclei.
Figure 3.
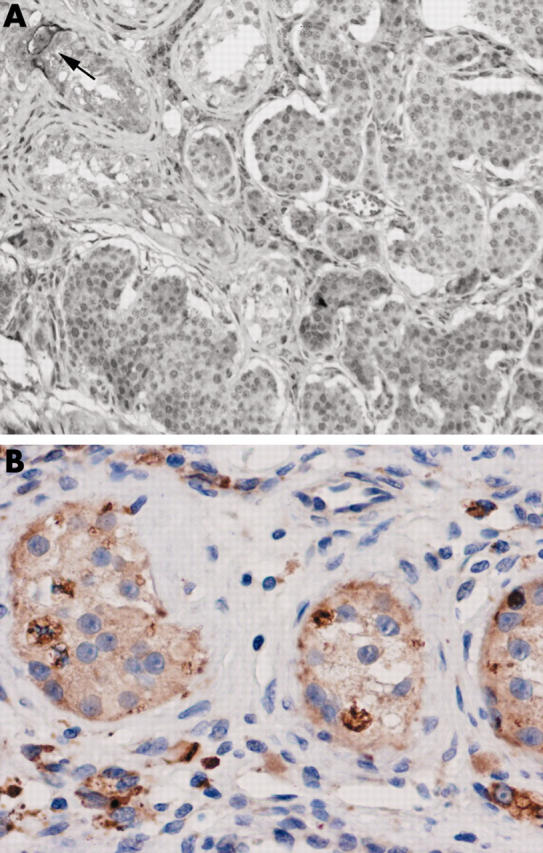
Immunohistochemistry findings showing tubules with cells with (A) membranous positivity to placental-like alkaline phosphatase (arrows) and (B) nuclear positivity for OCT4.
Metastatic tumour, measuring 0.3 to 1 cm, in the four preaortic lymph nodes, was morphologically identical to the testicular primary.
DISCUSSION
Our case provides an insight into the origin of testicular carcinoid. As with other heterotopic single tissue testicular tumours, such as epidermoid cysts, chondroma, etc., the origin of testicular carcinoid remains debatable, and consequently the World Health Organisation classification of testicular tumours5 includes carcinoid in the miscellaneous section.
Several histogenetic possibilities have been considered for these neoplasms. An origin from argentaffin cells was proposed by some,6 but was subsequently discarded because of the absence of such cells in the testis. A germ cell origin seems a more likely possibility and this is evident when the carcinoid is a component of testicular teratoma. Nevertheless, pure carcinoids are more frequent and are considered to be either monodermal germ cell tumours or the remaining component of burnt out teratoma.7
“From both clinicopathological and diagnostic viewpoints, it is important to distinguish between carcinoid as a primary testicular monodermal teratoma as opposed to a metastasis from an extragenital carcinoid of non-germ cell origin”
The finding of a concomitant precursor lesion of germ cell tumours, such as ITGCN,8 would support such an origin. However, two recent series of testicular carcinoids1,2 were unable to find ITGCN; an absence difficult to explain once inadequate sampling is discarded. Our present case reports for the first time ITGCN in the testicular tissue surrounding a pure carcinoid. The tubules adjacent to the carcinoid showed characteristically atypical intratubular cells with membranous PLAP positivity and nuclear positivity for OCT4, a highly specific marker for ITGCN.4 Our case shows similarities to a previous one,9 where a testicular mature cartilaginous nodule was thought to be a monodermal teratoma because it was associated with ITGCN. Similarly, a pure Wilms tumour of the testis was shown to be a type of monodermal teratoma10 by the identification of i(12p)—a characteristic chromosomal marker of testicular germ cell tumours—in the tumour karyotype. This finding is a more accurate demonstration of a germ cell origin than the more broadly non-specific study by fluorescence in situ hybridisation analysis of X chromosome gain in a series of testicular carcinoids.1
From both clinicopathological and diagnostic viewpoints, it is important to distinguish between carcinoid as a primary testicular monodermal teratoma as opposed to a metastasis from an extragenital carcinoid of non-germ cell origin.11 The last situation is extremely rare, with only 10 cases published in the literature, most of which originated in the gastrointestinal tract.3
Take home messages.
This is the first case of pure testicular carcinoid preaortic lymph node metastases to be described
The simultaneous occurrence of intratubular germ cell neoplasia in the surrounding testicular tissue was identified by OCT4 and PLAP positivity
This confirmed that the tumour had a germ cell origin in the testis, rather than being a metastasis from an extragenital carcinoid
Abbreviations
ITGCN, intratubular germ cell neoplasia
PLAP, placental-like alkaline phosphatase
The patient gave his informed consent for this case report to be published
REFERENCES
- 1.Kato N, Motoyama T, Kameda N, et al. Primary carcinoid tumor of the testis: immunohistochemical, ultrastructural and FISH analysis with review of the literature. Pathol Int 2003;53:680–5. [DOI] [PubMed] [Google Scholar]
- 2.Reyes A, Moran CA, Suster S, et al. Neuroendocrine carcinomas (carcinoid tumor) of the testis. A clinicopathologic and immunohistochemical study of ten cases. Am J Clin Pathol 2003;120:182–7. [DOI] [PubMed] [Google Scholar]
- 3.Xiao GQ, Birns DR, Warner RR, et al. Testicular metastasis of primary cecal carcinoid tumor. Ann Diagn Pathol 2004;8:102–7. [DOI] [PubMed] [Google Scholar]
- 4.Jones TD, Ulbright TM, Eble JN, et al. OCT4: a sensitive and specific biomarker for intratubular germ cell neoplasia of the testis. Clin Cancer Res 2004;10:8544–7. [DOI] [PubMed] [Google Scholar]
- 5.Woodward PJ, Heidenreich A, Looijenga LHJ, et al. Germ cell tumors. In: Eble JN, Sauter G, Epstein JI, et al, eds. WHO classification of tumours. VI. Pathology and genetics of tumours of the urinary system and genital organs. Lyon: IARC, 2004:221–49.
- 6.Talerman A, Gratama S, Miranda S, et al. Primary carcinoid tumor of the testis: case report, ultrastructure and review of the literature. Cancer 1978;42:2696–706. [DOI] [PubMed] [Google Scholar]
- 7.Berdjis CC, Mostofi FK. Carcinoid tumors of the testis. J Urol 1977;118:777–82. [DOI] [PubMed] [Google Scholar]
- 8.Dieckmann KP, Skakkebaek NE. Carcinoma in situ of the testis: review of biological and clinical features. Int J Cancer 1999;83:815–22. [DOI] [PubMed] [Google Scholar]
- 9.Singh N, Cumming J, Theaker JM. Pure cartilaginous teratoma differentiated of the testis. Histopathology 1997;30:373–4. [DOI] [PubMed] [Google Scholar]
- 10.Gillis AJ, Oosterhuis JW, Schipper ME, et al. Origin and biology of a testicular Wilms’ tumor. Genes Chromosomes Cancer 1994;11:126–35. [DOI] [PubMed] [Google Scholar]
- 11.Ulbright TM, Amin MB, Young RH. Germ cell tumors: non-seminomatous. In: Tumors of the testis, adnexa, spermatic cord and scrotum. Washington: Armed Forces Institute of Pathology, 1999:160–4.


