The sebaceous carcinoma is a very rare malignant tumour primarily found in the area of the eyelid. Most of these carcinomas originate in the tarsal meibomian glands although they may in extremely rare cases originate in the glands of Zeis of the eyelashes or the sebaceous glands of the caruncle.1 The periorbital primaries are reported to behave aggressively with the tendency to metastasise early with a significant mortality in most series.2
In many cases correct diagnosis of a sebaceous carcinoma of the eyelid is delayed not only as a result of the rarity of this tumour but also because of its ability to masquerade as a variety of other eye conditions such as chalazion or chronic blepharoconjunctivitis. A high index of suspicion is vital if these tumours are to be adequately treated.
We present a case of sebaceous carcinoma and discuss the clinical behaviour, the diagnosis, and the differential diagnosis difficulties as well as the therapy.
Case report
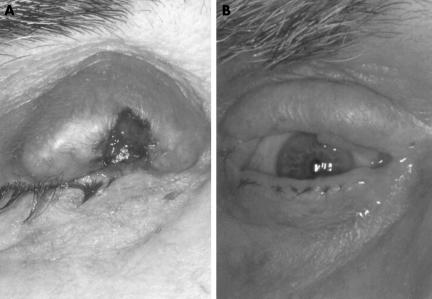
A 78 year old patient presented with a localised inflammation in the centre of the right upper eyelid. Under local antibiotic therapy for 6 weeks the lesion increased in size and showed putrid secretion on the surface. The patient refused further treatment and presented 22 months later with no healing of the lesion on the upper lid and a visible increase in size. The clinical examination revealed an ulcerating tumour measuring 3 cm in diameter at the right upper lid with a bloody encrusted lid margin (Fig 1A) and an enlarged lymph node on the right preauricular area of the parotid gland. The ocular examination revealed no conjunctival or corneal involvement. A biopsy of the eyelid tumour revealed a carcinoma of a meibomian gland with complete infiltration of the upper lid. Conjunctival map biopsies were negative.
Figure 1.
(A) A 78 year old man with a meibomian carcinoma of the right upper eyelid. Note the exulcerating tumour measuring 3 cm in diameter with a bloody encrusted lid margin. (B) Result 15 months after surgery.
Two weeks later a total resection of the upper lid with rapid section examination of the resection margins was carried out as well as the extirpation of the lymph node and an underlying metastasis beneath the parotid gland. Because the rapid section examination from the lateral mucosal border did not show any infiltration with tumour tissue, we decided to do a three layered primary reconstruction of the upper lid with a pedicled temporal island flap covered with a full thickness skin graft from the contralateral upper lid. The reconstruction of the conjunctiva was achieved by an oral mucosal graft. In order to make the raising of the lid possible, the flap was fixed on the fascial residue of the superior levator palpebrae muscle. The histopathological reappraisal revealed tumour stage T3N1 (Fig 2) and a R0 resection.
Figure 2.
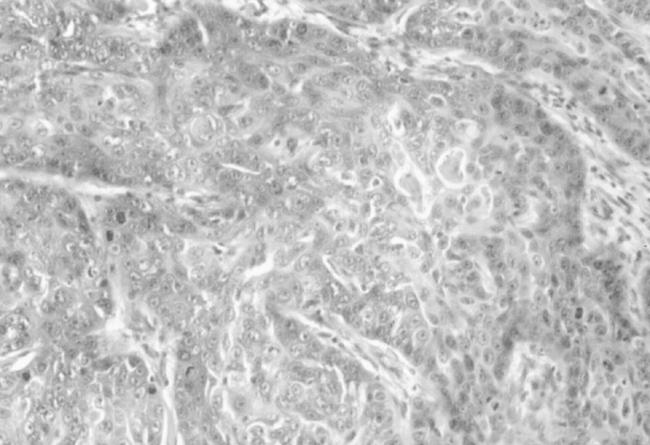
Deep infiltrating partly sebaceous differentiated tumour formations with high mitotic activity (haematoxylin and eosin, ×200).
Two weeks after the surgery a neck dissection was performed and an adjuvant radiation therapy of the right orbit as well as the cervical lymph draining was begun in 25 cycles with a dose of 50 Gy.
A local relapse or further metastasis 15 months after the surgery did not occur (Fig 1B).
Comment
The low incidence and the non-specific clinical symptoms led us to conclude that the diagnosis of a sebaceous carcinoma of the eyelid often occurs very late. One warning sign is the local loss of the eyelashes resulting from a tumour infiltration of the follicle. Every therapy refractive, one sided, tumour-like eyelid lesion has to be clarified histologically to rule out a sebaceous carcinoma. A full thickness eyelid biopsy combined with conjunctival map biopsies is the appropriate approach to the diagnosis.3 In our case we found the typical pagetoid infiltration of the overlaying epidermis at the margins of the widely exulcerated carcinoma. It presented without sign of multicentric growth, which together with pagetoid spread indicates poor prognosis.4
The therapy of choice for the sebaceous carcinoma is primarily a surgical one. If the tumour is very large or recurrent with demonstrated spread to bulbar conjunctiva, to the other eyelid, or to orbital tissue, a subtotal or complete exenteration may be necessary.5–7 If evidence of spread to regional lymph nodes is present a lymph node or radical neck dissection should be performed,8 usually combined with partial parotidectomy.3 An alternative to the surgical excision is the radiation therapy with a total dose of >50 Gy.9 Radiation therapy may be considered as an adjunct to local surgery. Recurrence of tumour usually occurs within 3 years following radiotherapy alone.10
There are some techniques of eyelid reconstruction presently available. An ideal eyelid reconstruction should replace the missing tarsoconjunctival structures and skin, protect the globe, give a natural appearance with only minor donor defect morbidity, and should be done as a one stage procedure. The temporal island flap described in our case report has the advantage of being a one stage procedure, which is relatively easy and quickly done and provides well vascularised tissues. A disadvantage is that the overlying temporal skin of the island flap can be very heavy, which makes de-epithelialisation or excision of the relatively thick skin and replacement by a full thickness skin graft necessary.
Postoperative patients must be followed up at short intervals as the tumour has a fast growth potential. The approximate guidelines are 3 monthly interval during the first year, 6 monthly during the second year, and then on a yearly basis for life.3
References
- 1.Batsakis JG, Littler ER, Leahy MS. Sebaceous cell lesions of the head and neck. Arch Otolaryngol 1972;95:151. [DOI] [PubMed] [Google Scholar]
- 2.Prioleau PG, Santa Cruz DJ. Sebaceous gland neoplasia. J Cutaneous Pathol 1984;11:396–414. [DOI] [PubMed] [Google Scholar]
- 3.Zürcher M, Hintschich CR, Garner A, et al. Sebaceous carcinoma of the eyelid: a clincopathological study. Br J Ophthalmol 1998;82:1049–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rao NA, Hidayat AA. Sebaceous carcinomas of the ocular adnexe. Hum Pathol 1982;13:113–22. [DOI] [PubMed] [Google Scholar]
- 5.Doxanos MT, Green WR. Sebaceous gland carcinoma. Arch Ophthalmol 1984;102:245–9. [DOI] [PubMed] [Google Scholar]
- 6.Haas AF, Kietly DW. Basal cell carcinoma. In: Mannis MJ, Macsai MS, Huntly AC, eds. Eye and skin disease. Philadelphia: Lippincott-Raven Publishers, 1996:395–403
- 7.Harvey JT, Anderson RL. The management of meibomian gland carcinoma. Ophthalmic Surg 1982;13:56–61. [PubMed] [Google Scholar]
- 8.Kostick Da, Linberg JV, McCormick SA. Sebaceous gland carcinoma. In: Mannis MJ, Macsai MS, Huntly AC, eds. Eye and skin disease. Philadelphia: Lippincott-Raven Publishers, 1996:413–17.
- 9.Yen MT, Tse DT, Wu X, et al. Radiation therapy for local control of eyelid sebaceous cell carcinoma: report of two cases and review of the literature. Ophthal Plast Reconstr Surg 2000;16:211–5. [DOI] [PubMed] [Google Scholar]
- 10.Nunery WR, Welsh MG, McCord CD Jr. Recurrence of sebaceous carcinoma of the eyelid after radiation therapy. Am J Ophthalmol 1983;96:10–15. [DOI] [PubMed] [Google Scholar]