Abstract
Aims: To describe the results of a study of the incidence of conjunctival ulceration and its pathology as a manifestation of Behçet's syndrome.
Methods: The authors reviewed retrospectively medical charts of 152 patients with Behçet's syndrome seen at the uveitis service of Okayama University Hospital from January 1995 to December 1999. Criteria used to diagnose Behçet's syndrome in this study required the presence of oral aphthous ulceration plus any two of three other manifestations—genital ulceration, eye lesions such as iridocyclitis and uveoretinitis, or skin lesions such as erythema nodosum. The presence of conjunctival ulceration was determined in patients with Behçet's syndrome through standardised ophthalmological examinations. A biopsy of the conjunctival ulceration was performed in one patient. The incidence of conjunctival ulceration in patients with Behçet's syndrome was calculated and the clinical and pathological features of this ulceration were examined.
Results: Four of 152 patients (2.6%) developed conjunctival ulceration in concordance with exacerbation of their systemic symptoms. Histopathological examinations of a conjunctival biopsy specimen in one patient revealed intraepithelial and perivascular infiltration with neutrophils and lymphocytes, consistent with Behçet's syndrome. The conjunctival ulcerations of the study patients showed good response to topical corticosteroids or topical steroids plus oral colchicine.
Conclusions: Conjunctival ulceration should be noted as an uncommon but possible manifestation of Behçet's syndrome. Accordingly, routine examination of the conjunctiva is recommended in patients with Behçet's syndrome, and Behçet's syndrome should be included in a list of differential diagnoses for patients with conjunctival ulcerations.
Keywords: conjunctival ulceration, Behçet's syndrome
Behçet's syndrome is a relapsing illness characterised by oral aphthous and genital ulceration, uveoretinitis, and skins lesions such as erythema nodosum. Frequent ophthalmic manifestations of this condition are iridocyclitis, retinal haemorrhages, and cotton wool spots. Conjunctival ulceration has been considered rare in Behçet's syndrome and, until now, has been described only in a few case reports.1–3 Accordingly, in this study, we examine the incidence and pathology of conjunctival ulceration in Behçet's syndrome.
PATIENTS AND METHODS
We reviewed the medical records of 152 consecutive patients with Behçet's syndrome seen during the 5 year period from January 1995 to December 1999 at the uveitis service in Okayama University Hospital. Of these 152 patients, 111 had been followed at this institution since before January 1995, while 41 patients were newly diagnosed with Behçet's syndrome or were referred during this 5 year period to the uveitis service after the diagnostic establishment of Behçet's syndrome. The patients included 67 men and 85 women, whose ages ranged from 13 to 78 years old (mean 42.7 years old) at their first visit during the 5 year period.
The diagnostic criteria for Behçet's syndrome used in this study required the presence of oral aphthous ulceration plus any two of three other manifestations—genital ulceration, eye lesions such as iridocyclitis and uveoretinitis, or skin lesions such as erythema nodosum.4 All patients were systemically examined by a doctor familiar with Behçet's syndrome or a dermatologist at least once during the 5 year period. At each visit during the follow up, the patients underwent standardised ophthalmological examinations, including visual acuity measurement, conjunctival inspection, slit lamp biomicroscopy, funduscopy after mydriasis, and intraocular pressure measurement by applanation tonometry. Additionally, the presence or absence of systemic signs of Behçet's syndrome was also evaluated at each visit. Fluorescein angiography was performed in all patients at the initial presentation and on the other occasions when eye symptoms showed exacerbation.
RESULTS
Four (three women and one man) of 152 patients with Behçet's syndrome developed conjunctival ulceration during the 5 year period. Statistical significance of female dominance could not be proved because of the small number of patients with conjunctival ulceration (χ2 test).
Case reports
Case 1
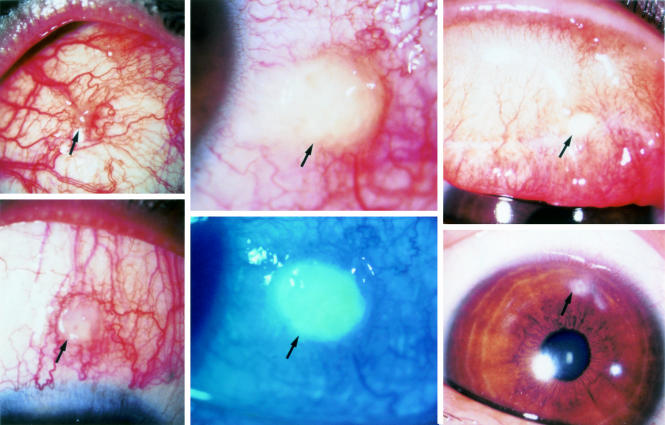
One month before presentation at our institution, a 40 year old woman, who had suffered oral and genital ulceration and erythema nodosum in the lower extremities for the previous 10 years, experienced foreign body sensation in both eyes. Diagnosed with Behçet's syndrome by a doctor 5 years earlier, she had taken oral colchicine 0.5–1 mg daily, which she discontinued at the time of ophthalmic presentation. Examination revealed several ulcerations in the bulbar conjunctiva of both eyes (Fig 1). No inflammation was found in the aqueous or fundus. Fluorescein angiography showed no retinal vascular inflammation, and the results of a conjunctival culture were negative. Administration of 0.1% fluorometholone eye drops four times daily, in addition to resumption of oral colchicine, led to subsidence of the conjunctival ulceration as well as a reduction of oral ulceration within approximately 2 weeks. Although conjunctival ulceration recurred in both eyes several times in the following 4 years, each recurrence was treated successfully with oral colchicine and 0.1% fluorometholone eye drops.
Figure 1.
Conjunctival ulceration (arrows) in four patients with Behçet's syndrome. An ulcer in the upper bulbar conjunctiva of the right eye in case 1 (top left); an ulcer in the temporal bulbar conjunctiva of the left eye in case 2 (top and bottom middle); a kissing ulcer in the upper palpebral conjunctiva and cornea of the right eye in case 3 (top and bottom right); and an ulcer in the upper bulbar conjunctiva of the left eye in case 4 (bottom left).
Case 2
A 24 year old woman with a family history (her father) of Behçet's syndrome, who had experienced oral ulceration, genital ulceration, and erythema nodosum for 1 year, developed a persistent ulceration on the temporal bulbar conjunctiva of the left eye of 3 months' duration. Ophthalmological examination revealed a best corrected visual acuity of 20/10 in both eyes. Although the patient had oral ulcerations at the time of presentation, no ophthalmic inflammation was found except for the conjunctival ulceration in the left eye (Fig 1). Fluorescein angiography showed no retinal inflammation. With the application of 0.1% betamethasone four times daily, the conjunctival ulceration resolved within 2 months. No oral medication was prescribed. Although this patient experienced recurrent oral ulcerations during the following 3 years, she developed no further conjunctival ulceration.
Case 3
A 27 year old woman, with a 7 year history of oral ulceration, experienced a 6 month increase in the number of episodes of oral ulceration as well as a month long occurrence of genital ulceration and erythema nodosum in the lower extremities, when she developed photophobia and tearing in the right eye. Leucocytosis, elevated serum C reactive protein (CRP) levels, and positive HLA-B51 were noted, and the patient was diagnosed with Behçet's syndrome. Ophthalmological examination revealed kissing ulcers in the upper palpebral conjunctiva and the cornea in the right eye (Fig 1). The conjunctiva in the left eye was normal, and there was no inflammation in the aqueous or fundus. Fluorescein angiography revealed no retinal vascular inflammation, and the results of conjunctival culture were negative. The conjunctival ulceration subsided gradually in the following 6 months with the administration of 0.1% fluorometholone eye drops four times daily. Oral colchicine 0.5 mg daily was given to control oral and genital ulcerations.
Case 4
A 54 year old man, diagnosed with Behçet's syndrome 6 years previously, developed iritis in the left eye one year after the diagnosis. During the 3 months before presentation, he experienced increased episodes of oral and genital ulceration, and erythema nodosum in the lower extremities, when he noticed redness, but no pain, in the left eye. This patient had taken oral colchicine intermittently, but was not taking oral colchicine at the time of presentation. Ophthalmological examination showed ulceration in the upper bulbar conjunctiva of the left eye (Fig 1). The conjunctiva in the right eye was normal, and no inflammation was noted in the aqueous or fundus. The patient resumed oral colchicine 1 mg daily in addition to the application of 0.1% betamethasone four times daily. Oral colchicine reduced the number of episodes of oral ulceration afterwards. The conjunctival ulcer subsided in 1 month; however, another ulcer developed on the temporal bulbar conjunctiva in the left eye, which was also successfully treated with 0.1% betamethasone.
Pathology
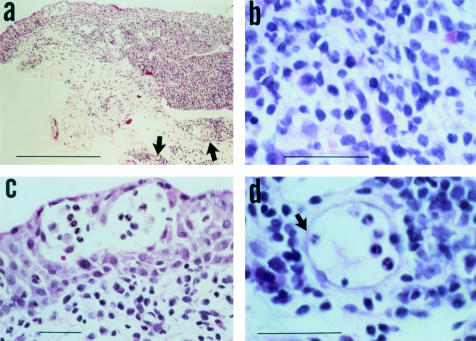
A biopsy of the ulcer in the bulbar conjunctiva of the right eye was performed in case 1. The ulcer bed was infiltrated mainly with lymphocytes, plasma cells, and neutrophils, as well as a small number of eosinophils (Fig 2). Intraepithelial neutrophil infiltration was also found. Lymphocytes and plasma cells had infiltrated around the vessels beneath the conjunctival epithelium, indicative of vasculitis. Immunohistochemical staining disclosed that infiltrating small lymphocytes consisted of an approximately equal number of T cells (positive for CD45RO, CD43, and CD3) and B cells (positive for CD20 and CD75). Overall, B cells were more dominant than T cells, when plasma cells were included in the count.
Figure 2.
Light micrographs of the biopsy specimen of the bulbar conjunctival ulcer in the right eye of case 1. Infiltration of the ulcer bed with inflammatory cells (a) and perivascular infiltration (arrows in (a)). Infiltrating cells consist mainly of small lymphocytes and plasma cells (b). Note intraepithelial infiltration with neutrophils (c) and intravascular adherence of neutrophils (arrow in (d)). Haematoxylin and eosin stain. Bars: a = 500 μm b, c, d = 50 μm.
DISCUSSION
In the four patients described in this report, conjunctival ulceration developed in concordance with the exacerbation of systemic symptoms of Behçet's syndrome such as oral and genital ulcerations and erythema nodosum. This indicates that conjunctival ulceration may develop as a clinical manifestation of Behçet's syndrome. In addition to conjunctival ulceration, corneal infiltration with ulceration was noted as a kissing ulcer corresponding to the lesion in the upper palpebral conjunctiva in case 3. Conjunctival ulcerations in all patients showed a positive response to topical corticosteroids or topical corticosteroids plus oral colchicine.
It should be noted that conjunctival ulceration in all four patients developed in the absence of intraocular inflammation. This suggests that conjunctival ulcers may present as an isolated finding in Behçet's syndrome without other retinal or intraocular inflammation. The present diagnostic criteria for Behçet's syndrome,4 as used in this study, require the presence of at least three of four signs such as oral and genital ulcerations or skin and eye lesions, with an emphasis on oral ulcerations. The eye lesions specified in the criteria do not include conjunctival ulceration; however, to better diagnose Behçet's syndrome, the dissociation of conjunctival ulceration with intraocular inflammation in the present four patients suggests that conjunctival ulceration may be recognised as one sign of eye lesions.
It should not be surprising that conjunctival ulcers develop in Behçet's syndrome as the conjunctiva is of course a mucous membrane, as are the oral and genital mucosa. Therefore, conjunctival ulceration would be expected to parallel the findings in the other mucosa. Such mucosal involvement would probably be distinct from intraocular inflammation in Behçet's syndrome. Conjunctival ulceration in the present series of patients was, indeed, observed in parallel with exacerbation of oral ulceration, but not in association with intraocular inflammation. All four patients were given topical corticosteroids for conjunctival ulceration, combined with oral colchicine in three of them, mainly to control the systemic manifestations such as oral ulceration. Topical corticosteroids did alleviate ocular symptoms in all the patients, but it remains unknown whether conjunctival ulceration might be rather self limiting. Oral colchicine, at least in case 1, did reduce the number of episodes of conjunctival ulceration in both eyes.
Until now, there have been three case reports describing patients with Behçet's syndrome who developed conjunctival ulceration: a 49 year old white man in the United States,1 a 45 year old woman in Italy,2 and a 45 year old woman in Tunisia.3 The clinical features of conjunctival ulceration in the present series of four patients are similar to those three patients reported previously. The incidence of conjunctival ulceration in this series is 2.6% (four of 152 patients). In comparison, the incidence of conjunctival ulceration in Turkey as reported and cited in Olivieri et al2 is 0.9% (five of 540 patients), similar to the present series.
In case 3 of the present series, corneal infiltration causing ulceration could have derived from the palpebral conjunctiva since the conjunctival and corneal lesions formed a configuration of a kissing ulcer. In a series of patients with Behçet's syndrome in England, corneal ulceration was also reported as an eye lesion, the incidence of which was as high as 16% (four of 25 patients).5 The incidence of corneal ulceration reported in the literature5 seems rather high in our experience, but the reason remains unknown.
A biopsy of the conjunctival ulceration in case 1 revealed infiltration of the ulcer bed, predominantly with neutrophils, small lymphocytes, and plasma cells as well as a small number of eosinophils. In addition, intraepithelial infiltration with neutrophils and their adhesion to the intravascular wall were observed. These findings were consistent with pathological findings of oral ulceration in Behçet's syndrome.6 Immunohistochemical staining of the specimen identified small lymphocytes as both T cells and B cells, supporting the role of T cells in Behçet's syndrome. Indeed, T cells were shown immunohistochemically to be involved in biopsy induced conjunctival inflammation in patients with Behçet's syndrome.7
In conclusion, conjunctival ulceration should be recognised as an uncommon but possible manifestation of Behçet's syndrome. Therefore, routine examination of the conjunctiva is recommended in patients with Behçet's syndrome, and Behçet's syndrome should be included in a list of differential diagnoses for patients with conjunctival ulcerations. In this context, ophthalmologists should look for systemic signs of Behçet's syndrome in patients presenting with conjunctival ulcerations. Once diagnosed, conjunctival ulcerations in Behçet's syndrome show good response to topical corticosteroids. In addition, oral colchicine can be used to reduce episodes of conjunctival as well as oral ulcerations.
REFERENCES
- 1.Winter FC, Yukins RE. The ocular pathology of Behçet's disease. Am J Ophthalmol 1966;62:257–62. [DOI] [PubMed] [Google Scholar]
- 2.Olivieri I, Genovesi-Ebert F, Signorini G, et al. Conjunctival ulceration in Behçet's syndrome. Ann Rheum Dis 1992;51:574–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ouertani A, Lasram L, Mili I. Behçet's disease revealed by an ocular conjunctival aphthous ulcer. A case report. J Fr Ophtalmol 1992;15:131–2. [PubMed] [Google Scholar]
- 4.International Study Group for Behçet's Disease. Criteria for diagnosis of Behçet's disease. Lancet 1990;335:1078–80. [PubMed] [Google Scholar]
- 5.Mason RM, Barnes CG. Behçet's syndrome with arthritis. Ann Rheum Dis 1969;28:95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poulter LW, Lehner T. Immunohistology of oral lesions from patients with recurrent oral ulcers and Behçet's syndrome. Clin Exp Immunol 1989;78:189–95. [PMC free article] [PubMed] [Google Scholar]
- 7.Tugal-Tutkun I, Urganciolu M, Foster CS. Immunopathologic study of the conjunctiva in patients with Behcet syndrome. Ophthalmology 1995;102:1660–8. [DOI] [PubMed] [Google Scholar]