No proved treatment exists for macular oedema secondary to central retinal vein occlusion (CRVO) despite the potential for significant visual loss in affected eyes. We report a patient with bilateral non-ischaemic CRVOs and macular oedema treated with intravitreal triamcinolone acetonide.
An 80 year old woman presented with a 2 week history of acute visual loss in her left eye (LE). She had a 9 month history of poor vision in her right eye (RE). On examination, visual acuity was counting fingers RE and 20/400 LE. Intraocular pressures were 12 and 14 mm Hg, respectively. Anterior segment examination showed bilateral pseudophakia with no evidence of neovascularisation. Dilated fundus examination revealed bilateral CRVOs with macular oedema. Collateral disc vessels were present in the RE. Fluorescein angiography showed diffuse leakage and blockage from intraretinal haemorrhages in both eyes with no areas of non-perfusion (Fig 1). OCT measured a central macular thickness of 735 μm in the RE and 589 μm in the LE (Fig 2A). Owing to the poor visual outcome in the RE with observation, the patient was offered an intravitreal injection of triamcinolone acetonide (Apothecon, Princeton, NJ, USA) in the LE. Topical 0.5% amethocaine (tetracaine, Novartis, Atlanta, GA, USA) was used for anaesthesia. Two drops were applied three times, 5 minutes apart. Betadine (povidone-iodine) 5% (Alcon, Ft Worth, TX, USA) was then applied to the conjunctiva. An injection of 4 mg (0.1 ml) triamcinolone was performed using a sharp 27 gauge, half inch needle through the inferior pars plana, 3.5 mm from the corneal limbus appropriate for her pseudophakic status.
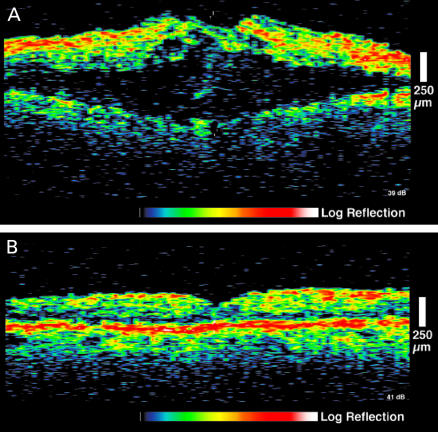
Figure 1.
Mid-phase fluorescein angiography of the left eye shows a central retinal vein occlusion with diffuse leakage and blockage secondary to retinal haemorrhage.
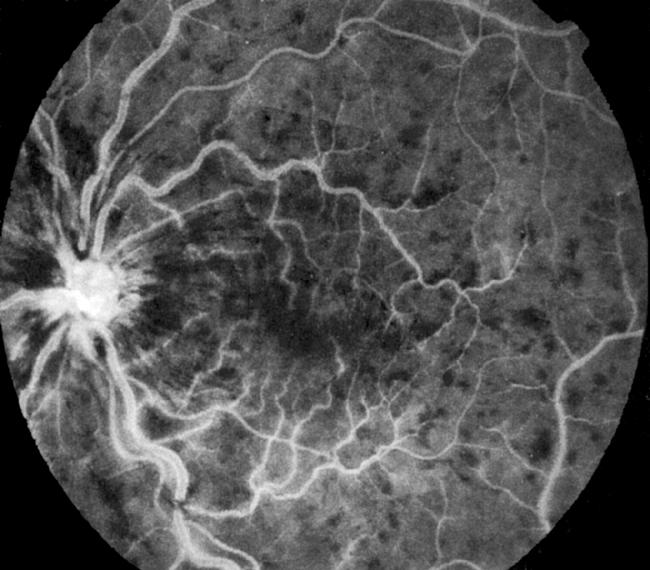
Figure 2.
(A) Optical coherence tomography of the left eye before first intravitreal triamcinolone acetonide injection demonstrating marked macular oedema with intraretinal cysts. (B) Resolution of macular oedema with restoration of normal foveal contour 6 weeks after intravitreal triamcinolone injection.
Six weeks post-injection, visual acuity was 20/80 in the LE. Central macular thickness measured 160 μm with a normal foveal contour (Fig 2B). Visual acuity was 20/30 after 3 months. Central macular thickness remained normal by OCT. Six months post-injection, visual acuity declined to 20/400 because of recurrence of macular oedema, measuring 834 μm by OCT. A second injection was performed in the LE. One month later, visual acuity was 20/50; central macular thickness measured 158 μm with restoration of a normal foveal contour.
Given the significant response in the LE, an intravitreal triamcinolone injection was performed in the RE. The macular oedema responded promptly (735–195 μm central macular thickness) with restoration of normal macular anatomy, but no visual benefit was appreciated. There was no significant elevation in IOP in either eye during the follow up period.
Macular oedema due to CRVO generally carries a poor visual prognosis. After 3 years, 58% of eyes will have vision worse than 20/100.1 Less than 20% of eyes will gain two or more lines of visual acuity. In addition, there are no proved treatment options. The Central Vein Occlusion Study demonstrated that grid photocoagulation had no significant impact on the final visual acuity of eyes with CRVO and macular oedema.1
In this case, a patient with an acute CRVO and macular oedema had significant improvement in visual acuity and complete resolution of macular oedema after each of two intravitreal injections of triamcinolone. A chronic CRVO with macular oedema in the other eye showed an anatomical response without visual improvement. Thus, early treatment may be necessary for visual improvement, before longstanding macular oedema results in irreversible photoreceptor damage. The mechanism by which this modality induces resolution of macular oedema in eyes with CRVO is unclear, though stabilisation of the blood-retinal barrier may play a significant part.2
The safety and efficacy of intravitreal triamcinolone has been well studied in animal models.2,3 It has also been used in humans for the treatment of choroidal neovascularisation and cystoid macular oedema due to uveitis.4,5 IOP elevation may occur in up to 25% of eyes after corticosteroid injection.5 Other potential risks of the procedure include cataract development, retinal detachment, and endophthalmitis.
This case suggests that the use of intravitreal triamcinolone acetonide for the treatment of macular oedema due to CRVO warrants further study.
REFERENCES
- 1.The Central Vein Occlusion Study Group. Evaluation of grid pattern photocoagulation for macular edema in central vein occlusion. Ophthalmology 1995;102:1425–33. [DOI] [PubMed] [Google Scholar]
- 2.Wilson CA, Berkowitz BA, Sato Y, et al. Treatment with intravitreal steroid reduces blood-retinal barrier breakdown due to retinal photocoagulation. Arch Ophthalmol 1992;110:1155–9. [DOI] [PubMed] [Google Scholar]
- 3.Tano Y, Chandler BS, Machemer R. Treatment of intraocular proliferation with intravitreal injection of triamcinolone acetonide. Am J Ophthalmol 1980;90:810–16. [DOI] [PubMed] [Google Scholar]
- 4.Danis RP, Ciulla TA, Pratt LM, et al. Intravitreal triamcinolone acetonide in exudative age-related macular degeneration. Retina 2000;20:244–50. [PubMed] [Google Scholar]
- 5.Antcliff RJ, Spalton DJ, Stanford MR, et al. Intravitreal triamcinolone for uveitic cystoid macular edema: an optical coherence tomography study. Ophthalmology 2001;108:765–72. [DOI] [PubMed] [Google Scholar]