We describe the clinical appearance and progress of bilateral ocular chemical injury caused by paraquat, a herbicide. Paraquat is used more commonly in developing countries and it has been associated with severe and prolonged ocular surface abnormalities due to the nature of the chemical.1 The current concepts in managing such an injury are reviewed.
Case report
A 69 year old fruit farmer splashed a 20% solution of paraquat into both his eyes. The exposure of the right eye to the solution was more marked. The eyes were irrigated for less than 5 minutes at the time of the injury, and a formal irrigation, using Ringer's solution for each eye, was not performed until presentation 5 hours later.
General medical history revealed that apart from controlled hypertension he was otherwise well and he had no previous history of ocular problems.
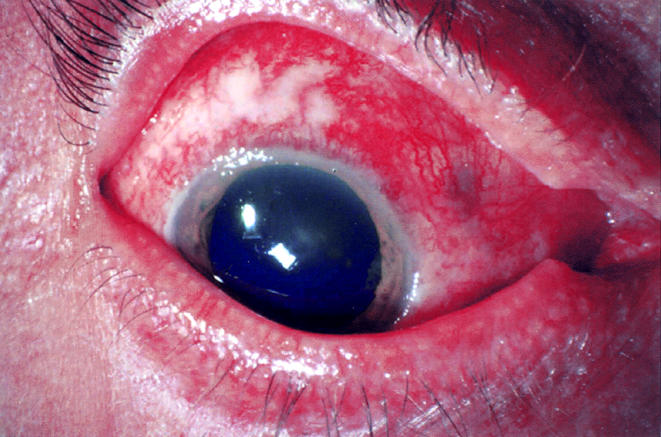
On arrival uncorrected visual acuity was 6/9 on the right and 6/12 on the left. The intraocular pressure was 14 mm Hg on the right and 19 mm Hg on the left. There was a circular 90% epithelial defect centred over the right cornea. The remaining corneal epithelium was opaque, leathery and oedematous (Fig 1). The left cornea was epithelialised although the surface was irregular and hazy in appearance (Fig 2). The conjunctiva was hyperaemic and chemotic, particularly on the right. The limbal vasculature initially appeared congested, but there was no evidence of episcleral ischaemia. The corneal stroma was clear. Examination did not reveal any abnormality of the anterior chamber, lens, or posterior pole in either eye.
Figure 1.
Right eye at presentation.
Figure 2.

Left eye at presentation.
The patient was commenced on our chemical burns protocol.2 This comprises topical citrate 10% drops every 2 hours, ascorbate 10% drops every 2 hours, chloramphenicol ointment four times daily, atropine 1% drops three times a day, fluorometholone acetate 1% drops every 2 hours, oral ascorbate 500 mg four times daily, and 4 g of a urinary alkaliniser (Ural, Abbot Pharmaceutical, IL, USA) containing 750 mg citric acid anhydrous and 630 mg sodium citrate anhydrous three times daily.
On the first day after presentation there was complete loss of the corneal epithelium in the right eye. The bulbar and tarsal conjunctival epithelium had also sloughed off. The conjunctiva in this eye was diffusely chemotic. There was extensive thrombosis of superficial and deep conjunctival vessels over the entire bulbar conjunctiva; however, the episcleral vessels remained intact and patent.
The left cornea had punctate epithelial erosions over most of its surface and an epithelial defect involving the inferomedial conjunctiva had just encroached onto the adjacent cornea. The conjunctiva in the left eye was also oedematous and had thrombosed vessels around the epithelial defect. Over the next few days the epithelial defect in the left eye enlarged to involve the inferonasal quadrant of the cornea although the conjunctival defect only enlarged slightly.
A severe pseudomembranous conjunctivitis developed in the right eye by the third day with fibrinous adhesions developing in the inferior fornix. Periodic glass rodding was commenced to break early symblepharon formation and the steroid was changed to non-preserved dexamethasone 1% hourly by day.
At 6 days post-injury there was evidence of epithelial healing from the margin of the epithelial defect in the inferior fornix of the right eye. Topical citrate and ascorbate were stopped and treatment was altered to non-preserved topical medication only: topical dexamethasone 1% every 2 hours, chloramphenicol four times daily, and hypromellose every 2 hours. Autologous serum tears (diluted to 20% in sterile saline solution) were also commenced 2 hourly.
Two weeks after the injury there were persistent epithelial defects in both eyes but the healing edge of conjunctival epithelium had reached the nasal limbus in the right eye. Best corrected visual acuity was 6/24 right and 6/6 left. At this stage there was no pseudomembrane present although the conjunctiva remained inflamed.
By 4 weeks after injury the ocular surface in both eyes had re-epithelialised. The cornea of the right eye at this stage was clear with no vascularisation. Visual acuity remained 6/24 on the right.
Impression cytology of both central corneas was undertaken at this point. The right cornea showed conjunctival-type epithelium with scattered goblet cells, polymorphonuclear leucocytes, and numerous apoptotic bodies. The left cornea demonstrated a corneal phenotype epithelium.
The last review was at 6 months post-injury. Uncorrected visual acuity was 6/9 in both eyes. The conjunctiva of both eyes remained minimally inflamed with mild erythema, chemosis, and subepithelial fibrosis now evident. These changes were more marked in the right eye (Fig 3). There was superficial pannus encroaching onto the right cornea predominantly superonasally. The affected area in the left eye shows subconjunctival fibrosis with vascular disorganisation and localised scleral translucency (Fig 4). Current treatment was dexamethasone 1% twice daily in both eyes.
Figure 3.
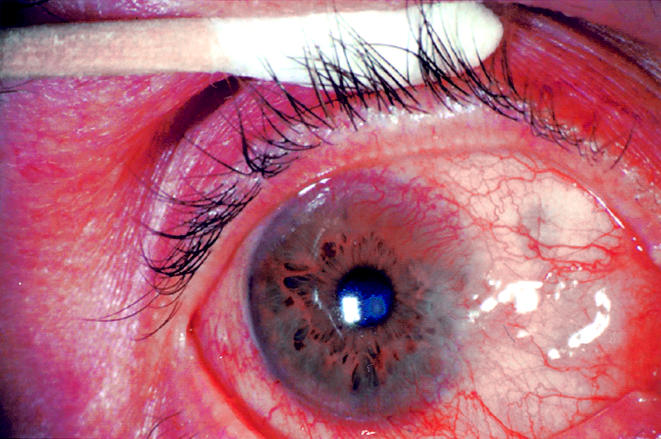
Right eye 6 months after injury.
Figure 4.
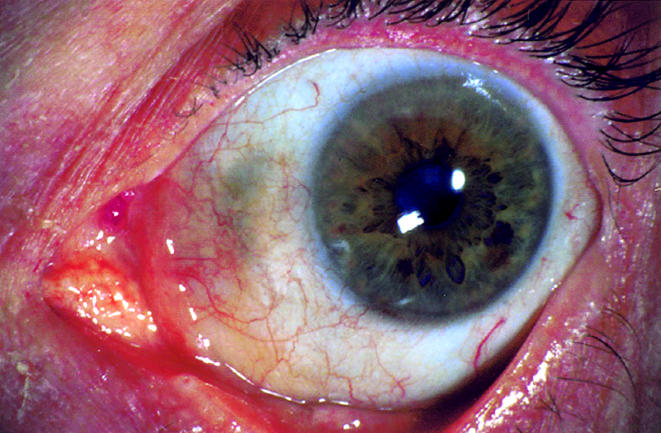
Left eye 6 months after injury
Comment
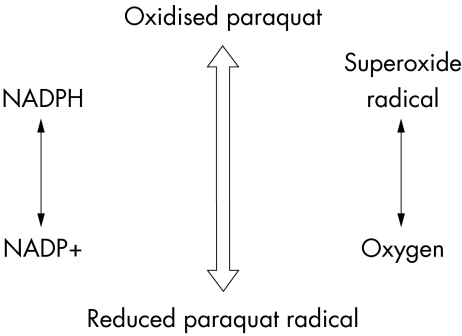
Paraquat is a dipyridylium quaternary ammonium salt that acts as an indiscriminate killer of all plant life. Preparations made commercially commonly contain the related compound diquat as well as surfactants to increase distribution over the leaf and aid penetration. Toxicity in humans is thought to relate to paraquat recycling in the redox reaction (Fig 5). This depletes NADPH and interrupts cell metabolism. The reduced paraquat then reoxidises using oxygen to generate a superoxide radical.
Figure 5.
Redox cycling reaction with paraquat.
The oxygen free radicals generated bind macromolecules and damage membrane lipids. Intracellular processes involving calcium are also affected. Paraquat may not be effectively cleared from the cell, resulting in persistent cell damage. Prolonged clinical effects lasting up to a year have been reported.
Documented cases of paraquat toxicity, although few, have noted a relatively mild initial appearance with a poor visual outcome in the long term. This has been the result of the development of a conjunctivalised corneal surface and chronic inflammation.1, 3
Paraquat ingestion can result in early fatality due to multiorgan failure. In less severe cases acute renal and hepatic toxicity is common. Pulmonary fibrosis may result in death. Pulsed methylprednisolone and cyclophosphamide during the inflammatory stages may have a profound effect on reducing the mortality.4 It is unclear whether a similar regimen would circumvent the long term sequelae of ocular paraquat injury.
The patient in this case had significant exposure to a commercial preparation with minimal first aid measures being implemented at the time of injury. He developed a severe surface injury over the first 48 hours with marked epithelial loss over one eye. This implied there were few, if any, viable limbal stem cells remaining. A severe pseudomembranous conjunctivitis then developed.
Previous reports of this extensive type of surface injury show that eventually conjunctivalisation of the cornea with vascular pannus is to be expected. Severe injury may result in a disordered ocular surface with dryness, symblepharon, ankyloblepharon, forniceal shortening, entropion, and trichiasis.
Patients with total limbal stem cell loss invariably develop superficial pannus and conjunctivalisation of the cornea. Evidence that previously conjunctival phenotypic epithelium can transdifferentiate into corneal type epithelium is derived from animal experiments with a debrided cornea and limbus where corneal epithelium healed the resultant defect.5 Viable limbal stem cells may thus have remained in the perilimbal crypts of Vogt. The right eye of this patient healed from conjunctival epithelium, confirmed by impression cytology, although most of the cornea remains clear without pannus. It has been reported that transdifferentiation is inhibited once neovascularisation occurs.5 In the left eye, which only had a small zone of limbal stem cell loss if any, the epithelium over the cornea was confirmed as corneal phenotype on impression cytology and there was no vascularisation.
A suitable microenvironment for healing should be encouraged through the use of medical therapy. Topical corticosteroids in the first week after injury promote successful healing of epithelial defects by controlling inflammation. Adequate lubrication is also important. Autologous serum tears have been reported to relieve the symptoms of dry eye6 and improve the ocular surface disease more successfully than conventional tear substitutes in dry eye states. These drops have also been instrumental in the healing of persistent epithelial defects.7 Essential components of the tear film present in serum tears include epidermal growth factor, vitamin A, and transforming growth factor β, which are important for the proliferation, differentiation, and maturation of the surface epithelium.7
We present a case of severe paraquat chemical injury to both eyes that had a good outcome from treatment. This case demonstrates a very good result from a usually devastating injury.
Preventing conjunctivalisation of the corneal surface after total loss of the limbal stem cell population remains a challenge. Therapeutic intervention may help restore a more functional surface visually. The use of intensive early antioxidant therapy followed by autologous serum tears and non-preserved ocular lubricants may have improved the outcome.
References
- 1.Vlahos K, Coggin M, Coster D. Paraquat causes chronic ocular toxicity. Aus NZ J Ophthalmol 1993;21:187–90. [PubMed] [Google Scholar]
- 2.Brodovsky SC, McCarty CA, Snibson GS, et al. Management of alkali burns. An 11-year retrospective review. Ophthalmology 2000;107:1829–35. [DOI] [PubMed] [Google Scholar]
- 3.Joyce M. Ocular damage caused by paraquat. Br J Ophthalmol 1969;53:688–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin JL, Leu ML, Liu YC, et al. A prospective clinical trial of pulse therapy with glucocorticoid and cyclophosphamide in moderate to severe paraquat-poisoned patients. Am J Respir Crit Care Med 1998;159:357–60. [DOI] [PubMed] [Google Scholar]
- 5.Tseng SCG, Hirst LW, Farazdaghi M, et al. Goblet cell density and vascularisation during conjnunctival transdifferentiation. Invest Ophthalmol Vis Sci 1984;25:1168–76. [PubMed] [Google Scholar]
- 6.Tsubota K, Goto E, Fujita H, et al. Treatment of dry eye by autologous serum application in Sjogren's syndrome. Br J Ophthalmol 1999;83:390–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsubota K, Goto E, Shimmura S, et al. Treatment of persistent corneal epithelial defects by autologous serum application. Ophthalmology 1999; 106:1984–9. [DOI] [PubMed] [Google Scholar]