Abstract
Aim: To describe a distinctive spectrum of retinal microvascular abnormalities in 12 patients with neurofibromatosis type 1 (NF-1).
Methods: This is an observational prospective study of the ocular fundus evaluated by direct ophthalmoscopy with or without fluorescein angiography, to investigate retinal microvascular abnormalities in 32 patients with NF-1 and in 30 control subjects. The evaluation included a complete general and neurological physical examination and in some cases computed tomography, magnetic resonance imaging with gadolinium-DTPA, or both.
Results: The occurrence of a distinctive spectrum of retinal microvascular abnormalities is described in 12 patients with NF-1 (37.5%). At the lower end of the spectrum, present in 10 patients, the anomaly consisted of minuscule second or third order tortuous venules, which were called “corkscrew retinal vessels.” These were usually isolated but in a few cases multiple. They flow towards the superior or inferior temporal veins. They had a length of one to two disc diameters. They ended either in a minute tuft or vanished on the retinal surface. The upper end of the spectrum was seen in only two patients. One of them had an exceptionally large venous anastomosis on the nasal retina and the other had an arteriovenous malformation extending over one retinal quadrant. None of the patients in the control group had such retinal microvascular abnormalities.
Conclusion: The “corkscrew” retinal vessels described in this report constitute a broad spectrum of microvascular markers in NF-1 patients.
Keywords: neurofibromatosis, corkscrew retinal vessels, retinal microvascular abnormalities, choroidal neurofibroma
Neurofibromatosis type 1 (NF-1) is an autosomal dominant condition affecting one in 4000 individuals. The responsible gene has been located on chromosome 17. Except for Lisch nodules, ocular manifestations are relatively infrequent in NF-1. These consist of choroidal and retinal hamartomas.1–3 In this study, we report the existence of retinal microvascular abnormalities in 12 individuals.
PATIENTS AND METHODS
We evaluated 32 consecutive patients with the diagnosis of NF-1 based on criteria established by the NIH.4 Every patient received a thorough systemic, neurological, and neuro-ophthalmological evaluation, with special attention to retinal findings by direct ophthalmoscopy. In 12 patients, five males and seven females, between 14 and 40 years of age (mean 24.9 years), distinctive retinal microvascular abnormalities were observed and documented with retinal photographs and in six patients fluorescein angiography was also obtained. Table 1 shows their demographic characteristics and associated conditions. Thirty healthy individual served as our controls.
Table 1.
Patients from this series
| Case | Age | Sex | VA | FA | LN | ULPN | CN | Associated extraocular findings |
| 1 | 29 | 20/20 OU | − | + | + | − | NF right leg | |
| 2 | 21 | M | 20/15 OU | − | + | + | − | − |
| 3 | 27 | M | 20/20 OU | − | + | − | − | Systemic lupus erythematosus, abdominal NF |
| 4 | 23 | F | OD 20/40 | + | + | − | + | ONSM OD |
| OS 20/15 | ||||||||
| 5 | 14 | F | 20/20 OU | − | + | − | − | Malignant Schwannoma (retroperitoneal) |
| 6 | 26 | F | 20/20 OU | + | + | − | − | Chiasmal astrocytoma |
| 7 | 23 | F | 20/15 OU | + | + | − | + | − |
| 8 | 37 | F | OD NPL | − | + | + | − | Sphenoidal dysplasia, meningoblastic meningioma |
| OS 20/15 | ||||||||
| 9 | 22 | F | 20/20 | + | + | − | + | − |
| 10 | 16 | M | 20/20 | + | + | − | − | − |
| 11 | 40 | M | 20/20 | + | + | − | + | NF right leg |
| 12 | 21 | F | 20/20 OU | + | + | − | − | Large navus back |
VA = visual acuity, FA = fluorescein angiogram, LN = Lisch nodules, ULPN = upper lid plexiform neurofibroma, CN = choroidal neurofibroma, OU = both eyes, OD = right eye, OS = left eye, ON = optic nerve, NF = neurofibroma, ONSM = optic nerve sheath meningioma.
RESULTS
In 12 of 32 patients with NF-1 (37.5%) we identified a spectrum of retinal microvascular abnormalities of diverse complexity, spanning from a single affected vessel, which we called “forme fruste” of the anomaly, to the full blown manifestation, called the “complex form.” The lower end of the spectrum was observed in 10 patients. The anomaly was located within two disc diameters of the optic disc, and consisted in a small (second or third order venule) tributary of the superior or inferior temporal vein or less frequently the nasal veins (two cases). The small, tortuous vessel usually spanned one or two and a half disc diameters, bending andwarping upon itself like a corkscrew and vanishing or ending in a minute tuft. Fluorescein angiography, performed in six of our 12 patients, demonstrated the anomaly more clearly. The anomaly did not leak fluorescein (see Figs 1–3).
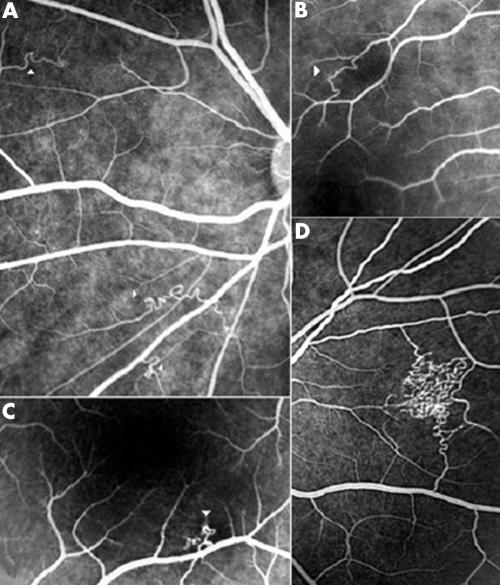
Figure 1.
Collage of various retinal microvascular abnormalities in NF-1. Fluorescein angiographic spectra of various corkscrew retinal microvascular abnormalities. Notice bizarre arrangement of corkscrew vessels in different individuals. Patient 9 (A), patient 7 (B), patient 4 (C), patient 5 (D).
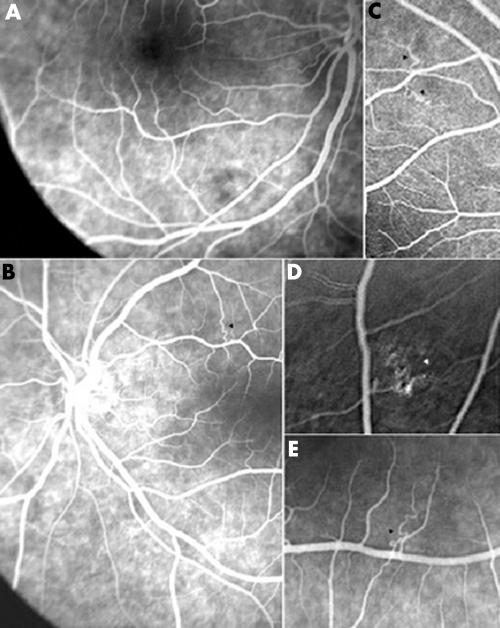
Figure 2.
Collage of various retinal microvascular abnormalities and choroidal neurofibromas in NF-1. Fluorescein angiograms (A) and (B) show patchy hyperfluorescence from underlying choroidal neurofibromas. Photographs (C), (D), and (E) show retinal microvascular abnormalities (arrowheads) in various patients from this series.
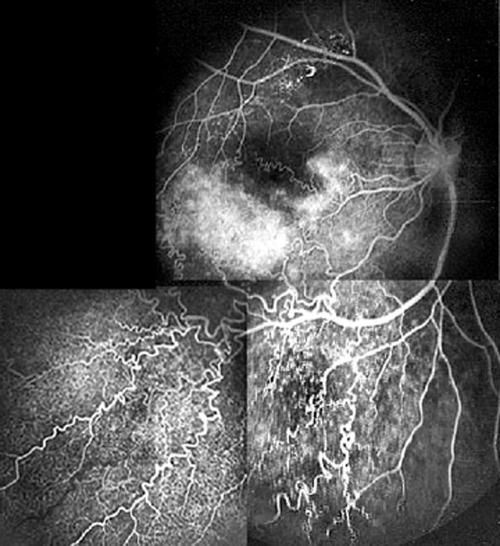
Figure 3.
Fluorescein angiogram from patient 12. Photographic composition of retinal microvascular malformation with grotesque arrangement of retinal corkscrew vessels in the inferotemporal retina. Notice choroidal neurofibroma (paramacular white blush).
Most of the anomalies were found in the left eye and in three cases were bilateral. In nine cases only one vessel was involved and in the remaining three cases more than one. One patient had the anomaly in four separate venules.
At the upper end of the spectrum we found two patients whose abnormalities were much more striking. One was a venovenous anastomosis in the nasal retina, covered by a thin layer of capillaries, and the other a more extensive arteriovenous malformation coexisting with an epiretinal membrane. Two patients also had choroidal neurofibromas. All these findings were completely asymptomatic and visual function was unaffected in each case. None of the 30 control subjects had retinal microvascular abnormalities.
DISCUSSION
Except for a recent report by one of us (RMM) describing these findings in eight patients with NF-1, such a condition has not been reported previously.5 The retinal microvascular abnormalities in our 12 patients seem to constitute retinal markers of NF-1. In a majority the anomaly consisted of a very subtle vascular change confined to small venules that can easily pass unnoticed. The condition does not affect vision. Fluorescein angiography enhances the anomaly but does not show leakage of dye. We believe these are congenital stable retinal microvascular abnormalities, as evidenced by their unchanging appearance over the years we have observed them. We are uncertain as to the nature of these findings.
Acknowledgments
The authors wish to thank Professor William F Hoyt from the Neuro-ophthalmology Unit at the University of California San Francisco, for his expert editorial assistance.
REFERENCES
- 1.Savino PJ, Glaser JDS, Luxenberg MN. Pulsating enophthalmos and choroidal hamartoma. Two rare stigmata of neurofibromatosis. Br J Ophthalmol 1977;61:483–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Destro M, D'Amico DJ, Gragoudas ES, et al. Retinal manifestations of neurofibromatosis. Diagnosis and management. Arch Ophthalmol 1991;109:662–6. [DOI] [PubMed] [Google Scholar]
- 3.Yasunari T, Shiraki K, Hattori H, et al. Frequency of choroidal abnormalities in neurofibromatosis type 1. Lancet 2001;356:988–91. [DOI] [PubMed] [Google Scholar]
- 4.National Institutes of Health Consensus Development Conference. Neurofibromatosis Conference Statement. Arch Neurol 1988;45:575–80. [PubMed] [Google Scholar]
- 5.Muci-Mendoza R. Anormalidades vasculares retinianas en neurofibromatosis con documentación de un hamartoma vascular puro no descrito. Gac Méd Caracas 1999;107:13–31. [Google Scholar]