The use of topical mitomycin C (MMC) to prevent recurrence after pterygium surgery is increasing since its introduction by Kunitomo and Mori in Japan, and its subsequent popularisation in the United States by Singh and associates.1 Low dose MMC (0.02%) twice daily for 5 days after the operation has been prospectively studied with long term follow up, and few serious side effects have been noted.2, 3 Intraoperative MMC appeared to be an effective and safe adjunctive treatment of primary pterygium excision.4
Case Reports
We retrospectively analysed three patients who presented at the Haemek Medical Central, Afula, Israel with scleral melting which developed after pterygium excision between October and November 2000, with intraoperative application of MMC (0.02% for 3 minutes). The MMC was washed out immediately with an abundant amount of balanced salt solution for at least 3 minutes. During the past 10 years we performed over 300 pterygium excisions with intraoperative use of MMC in Haemek Medical Center with three cases having serious complications.
Case 1 (Fig 1)
Figure 1.
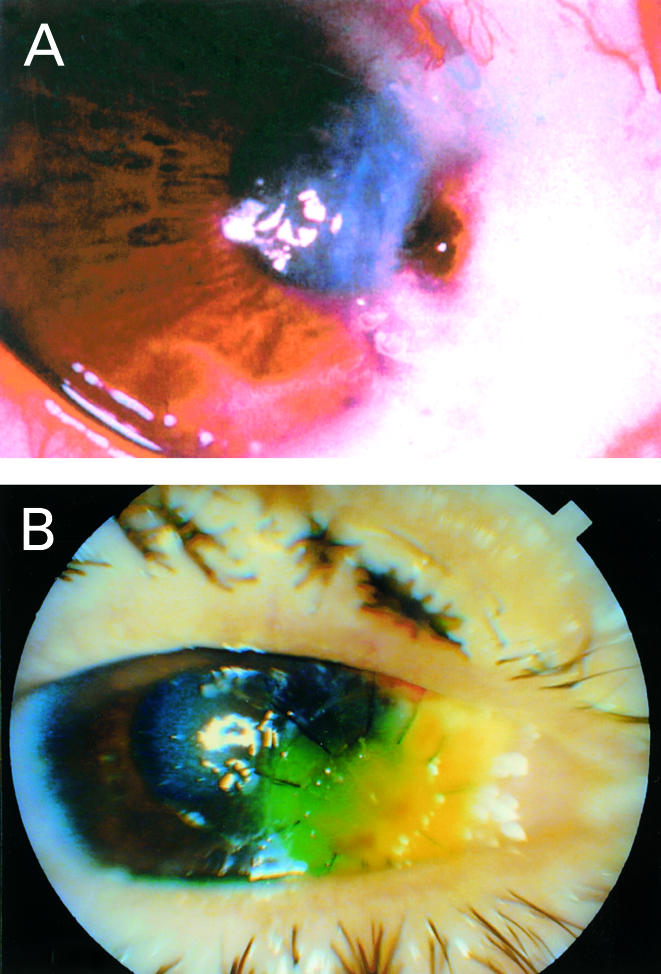
A previously healthy 50 year old man underwent recurrent pterygium excision of the right eye using a bare sclera technique with intraoperative application of MMC 0.02% for 3 minutes, having undergone pterygium excision with MMC 10 months earlier in his right eye. Visual acuity was 6/9+ SC. Preoperative ophthalmological examination revealed a nasal flashy wide lesion 4.5 mm over the limbus and inferior symblepharon, with the remainder of the examination being normal. He was released on the same day, following surgery at which time there were no complications. On the first (postoperative day 1) and second (postoperative day 7) follow ups no complaints or complications were noted. However, on postoperative day 30, corneal limbal perforation and iris incarceration in the wound was noted. Immediately, he underwent right eye corneal tectonic graft surgery. At his last follow up (12 weeks after the pterygium excision with MMC), the best corrected visual acuity was 6/24 CPH, the graft has good adaptation, no gap and no rejection signs.
Case 2 (Fig 2)
Figure 2.
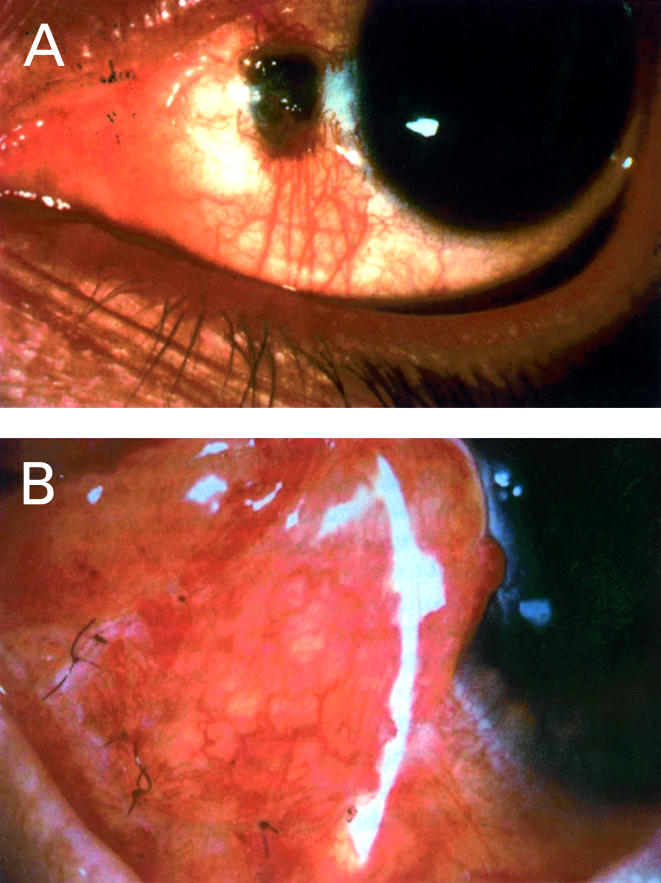
A previously healthy 37 year old man underwent pterygium excision of the left eye using a bare sclera technique with intraoperative application of MMC 0.02% for 3 minutes. His presenting symptoms were cosmetic only. Visual acuity was 6/6 partial SC. Preoperative ophthalmological examination revealed nasal flashy wide lesion 2.8 mm over the limbus with the remainder of the examination being normal. Two years previously he had undergone pterygium excision of the right eye using a bare sclera technique with intraoperative application of MMC 0.02% for 3 minutes. The right eye procedure had been successful and was performed in the same institute. Three weeks after the surgery, on routine follow up scleral melting and necrosis were noted. The scleral defect was unresponsive to ocular lubricants, topical antibiotics, topical steroids, and patching. Ten weeks after the left eye pterygium excision and MMC application, he underwent autologous conjunctival graft surgery to repair the defect. Follow up 2 weeks later showed that the graft has good adaptation and re-epithelialisation was noted.
Case 3
A previously healthy 70 year old man underwent pterygium excision of the right eye using a bare sclera technique with intraoperative application of MMC 0.02% for 3 minutes. On preoperative examination: visual acuity 6/24 partial SC in the right eye and 6/60 SC in the left, anterior segment was quiet except flashy temporal pterygium 7 mm over the limbus partially covering the pupil axis in the right eye. The procedure of the right eye pterygium excision with MMC was successful and performed in the same institute. No complaints or complications were noted at the first two follow ups; however, 3 weeks postoperatively right eye temporal scleral melting and ectasia was seen ( 3 mm × 3 mm in size). Conservative topical treatment with antibiotics, topical anti-inflammatory agents, and steroids failed to resolve the situation. Consequently, 8 weeks after the initial right eye surgery he underwent right eye conjunctival flap grafting over the area of scleral melting. At his last examination best corrected visual acuity was 6/36 partial, blood vessel growth was noted towards the bare sclera and re-epithelialisation with minimal staining. He is still being treated with topical antibiotics with some improvement.
Comment
Mitomycin C is an antineoplastic antibiotic agent isolated from the fermentation filtrate of Streptomyces caespitosus. Its action is similar to alkylating agents; it alkylates and crosslinks DNA and, in addition, may generate superoxide and hydroxyl radicals in solution. It also inhibits DNA, RNA, and protein synthesis.5
These combined effects may result in a long term influence on cellular proliferation.
Scleral melting occurring after pterygium surgery with adjunctive treatment has been well reported.6, 7 However, no serious complications were noted in the study by Frucht-Pery and Ilsar8 with postoperative use of 0.1 mg/ml MMC twice daily for 5 days (with a mean follow up period of 15.3 months) or in intraoperative MMC treated eyes.4 A common element in toxicity with MMC is a relatively large cumulative dose.7 Therefore, most ophthalmologists believe that a single intraoperative exposure to MMC would reduce the complication rate of MMC eye drop regimen.4
In the current series, all patients underwent pterygium excision in the bare sclera technique with the low concentration of 0.02% of MMC and a short application of 3 minutes. Among our patients one had corneal perforation that was treated by tectonic keratoplasty and other two had severe deep scleral melting that required conjunctival flaps or autologous graft. Our patients were all healthy, without conditions predisposing to ulceration or poor wound healing such as Sjögren syndrome, severe keratoconjunctivitis sicca, acne rosacea, atopic keratoconjunctivitis, or herpes keratitis (Table 1). We suspected that the MMC concentration was not appropriate during that period. We checked the concentration and it was difficult to obtain precise results after a waiting period, owing to the degradation of the material.
Table 1.
| No | Age/sex/race | Presenting symptom | Clinical finding | Treatment | Preop VA v postop | Outcome |
| 1 | 50/M/white | Blurred vision, dust sensation | Limbal perforation with iris incarceration in the wound | Tectonic corneal graft | 6/9+ SC 6/24 CPH | Good graft adaptation. No recurrence of pterygium after 12 weeks |
| 2 | 37/M/white | Cosmetic disturbance | Scleral nasal melting (3 mm × 2 mm) | Trial at conservative topical treatment failed. Autologous conjuctival graft | 6/9+ SC 6/12+ SC | Good graft adaptation at last follow up |
| 3 | 70/M/white | Pterygium covering the pupil visual axis | Scleral temporal melting (3 mm × 3 mm) | Trial at conservative topical treatment failed. Conjuctival flap | 6/24 pt CC 6/36 pt CC | Blood vessels growth towards the bare sclera with re-epithelisation. No recurrence of pterygium after 12 weeks |
This report raises serious questions regarding routine use of MMC. Recently, some investigators have evaluated the safety and efficacy of low dose MMC (0.02%) for an even shorter time (30 seconds).9 All ophthalmologists should be aware of the possibility of vision threatening complications and avoid routine and broad use of mitomycin in all fields.
References
- 1.Singh G, Wilson MR, Foster CS. Mitomycin eye drops as treatment for pterygium. Ophthalmology 1988;95:813–21 [DOI] [PubMed] [Google Scholar]
- 2.Hayasaka S, Noda S, Yamamoto Y, et al. Postoperative instillation of low dose mitomycin-c in the treatment of primary pterygium. Am J Ophthalmol 1988; 106:715–8. [DOI] [PubMed] [Google Scholar]
- 3.Rachmiel R, Leibe H, Levartovsky S. Results of treatment with topical mitomycin C 0.02% following excision of primary pterygium. Br J Ophthalmol 1995;79:233–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cano-Para J, Diaz-Llopis M, Maldonado MJ, et al. Prospective trial of intraoperative mitomycin C in the treatment of primary pterygium. Br J Ophthalmol 1995; 79:439–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glaubiger D, Ramu A. Antitumor antibiotics. In: Chabner BA, ed. Pharmacologic principles of cancer treatment. Philadelphia: WB Saunders, 1982:407–10.
- 6.Mackenzie FD, Hirst LW, Kynaston B. Reccurence rate and complications after beta-irradiation for pterygium. Ophthalmology 1991;98:1776–80 [DOI] [PubMed] [Google Scholar]
- 7.Rubenfeld RS, Pfister RS, Stern RM, et al. Serious complications of topical mitomycin-c after pterygium surgery. Ophthalmology 1992;99:1647–54. [DOI] [PubMed] [Google Scholar]
- 8.Frucht-Pery J, Ilsar M. The use of low dose mitomycin-c for prevention of recurrent pterygium. Ophthalmology 1994; 101:759–62. [DOI] [PubMed] [Google Scholar]
- 9.Cheng HC, Sung-Huel T, Ping-Lin K, et al. Low-dose intraoperative mitomycin C as chemoadjuvant for pterygium surgery. Cornea 2001;20:24–9. [DOI] [PubMed] [Google Scholar]


