Abstract
Background/aims: Retinal nerve fibre layer analysis by scanning laser polarimetry has been shown to facilitate diagnosis of glaucoma while its role in glaucoma follow up is still unclear. A major difficulty is the slow reduction of retinal nerve fibre layer thickness in glaucomatous optic neuropathy. Eyes of patients were studied after acute retrobulbar optic nerve lesion in order to evaluate the usefulness of scanning laser polarimetry in documenting retinal nerve fibre layer loss over time.
Methods: Five patients who suffered severe retrobulbar optic neuropathy have had repeated measurements of the retinal nerve fibre layer using scanning laser polarimetry at various intervals, the first examination being within 1 week of injury.
Results: All eyes showed a marked decrease in peripapillary retinal nerve fibre layer thickness, which followed an exponential curve and occurred predominantly within 8 weeks of injury. Compared to a previous study using red-free photographs, scanning laser polarimetry showed retinal nerve fibre layer loss earlier in the course of descending atrophy.
Conclusion: Scanning laser polarimetry is useful for early detection and documentation of retinal nerve fibre layer loss following acute injury to the retrobulbar optic nerve. It seems to be a promising tool for follow up of individual glaucoma patients.
Keywords: scanning laser polarimetry, optic neuropathy, optic nerve injury, retinal nerve fiber layer
Retinal nerve fibre layer (RNFL) analysis by scanning laser polarimetry has been developed to facilitate both diagnosis and follow up in glaucoma. The nerve fibre analyser (NFA; Laser Diagnostic Technologies, San Diego, CA, USA), commercially available since 1993, is a confocal scanning laser ophthalmoscope that can assess the thickness of peripapillary RNFL by measuring the retardation of the laser beam as it double passes the birefringent retinal nerve fibre layer. The polarising properties of the cornea and lens are neutralised by a built-in compensator. Weinreb et al demonstrated in 1995 that this method provides a quantitative measurement of nerve fibre layer thickness which is consistent with known properties of axonal loss in glaucomatous optic neuropathy.1 At the outset of this study scanning laser polarimetry was not an established method for follow up of glaucoma patients, and at present published studies on the effectiveness of scanning laser polarimetry for following RNFL thickness over time are still scarce.2–5 A major difficulty in evaluating scanning laser polarimetry as a clinical tool in the long term management of individual glaucoma patients is the slow decrease of RNFL thickness in the course of glaucomatous optic neuropathy. In contradistinction, acute severe retrobulbar injury to the optic nerve is known to cause a much more rapid loss of optic nerve axons. We therefore initiated a study of eyes with previous acute injury to the optic nerve to evaluate the usefulness of scanning laser polarimetry in documenting RNFL loss over time. In addition, provided that quantification of axonal loss could be achieved, we set out to analyse the time course of the evolving descending optic atrophy following acute optic nerve injury.
PATIENTS AND METHODS
Five patients with severe acute unilateral intracanalicular or intracranial lesions to the optic nerve were included in the study since 1994. Their mean age was 38 years (range 19–58); three of them were male and two were female. Two patients suffered an injury to the optic nerve in the setting of a fulminant infectious pansinusitis with direct invasion of the nerve (patients 2 and 4), two had fractures of the optic canal (patients 3 and 5), and one had inadvertent trauma to the intracranial portion of the optic nerve during extirpation of a pituitary adenoma (patient 1). All patients showed acute and severe visual loss with relative afferent pupillary defect on the affected side, normal initial funduscopic findings, and subsequent development of pronounced optic disc pallor (Fig 1). They had sequential ophthalmological examinations as well as repeated measurements of the peripapillary RNFL using scanning laser polarimetry with the nerve fibre analyser I , II, or GDx (Laser Diagnostic Technologies, San Diego, CA, USA). Only one technology was used per individual. Unfortunately, we could not use the healthy eye as control owing to poor fixation of the affected eye.
Figure 1.
Right fundus of patient 1 before (A) and 16 weeks after (B) injury to the right intracranial optic nerve. The evolution of optic atrophy is clearly visible.
All scanning laser polarimetry measurements were performed by the same skilled operator (M-JC). The first examination was performed within the first week after injury, except for patient 1, in whom the measurements were obtained 4 days before injury. Examination intervals and length of follow up were variable and are shown in Figure 2. Informed consent has been obtained from all patients.
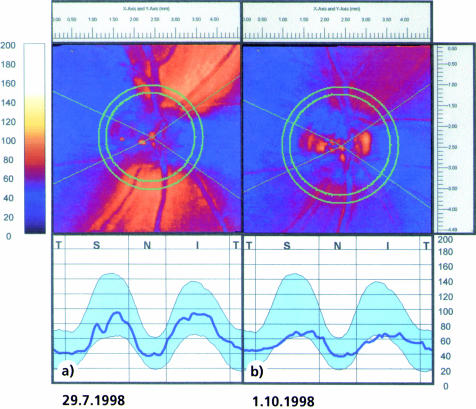
Figure 2.
Nerve fibre layer analysis in patient 5 at the initial (A) and last (B) visit after 9 weeks. The loss of peripapillary nerve fibres over time is evident both in the diminishing yellow-red tones of the false colour retardation image (above) as well as in the flattening of the double hump pattern (below).
NFA and GDx raw data were refined using an algorithm to standardise the individual retardation values. In addition, a blood vessel removal algorithm has been applied. To compare the data which were acquired with three different versions of the instrument, the first measurement of the RNFL of each patient was set as 100% and following measurements were expressed as a percentage of the initial value.
RESULTS
Each individual showed a marked decrease in peripapillary RNFL thickness during observation (Figs 2 and 3). The decrease occurred predominantly within the first 7–8 weeks after injury. Two patients (patients 2 and 5) showed an initial increase in RNFL thickness between the first and the second examination before the expected decrease occurred.
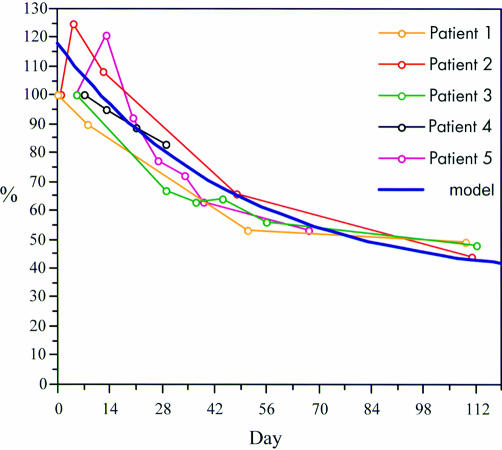
Figure 3.
Individual relative measurements of retardation values obtained by scanning laser polarimetry in the injured eye at each visit (indicated by circles) in all five patients, shown in different colours. The initial value was set as 100% and all subsequent values as percentages thereof. A calculated model is drawn as a solid dark blue curve.
The time course of axonal loss can be represented by an exponential decay with a relaxation time of 48.2 days, an amplitude of 83.2 and a base line of 34.6. The equation used was
 |
where y is the percentage of the initial retardation value, and t the time from injury in days (dark blue line in Fig 3). This means that after 48.2 days (that is, 7 weeks) the amplitude fell off to 1/e of its initial value (83.2/e = 30.6 ) and after 14 weeks to 1/e2 of its initial value.
DISCUSSION
Scanning laser polarimetry is a reproducible method to assess peripapillary RNFL thickness in healthy and glaucomatous eyes.6 In the present study we have demonstrated that progressive RNFL loss following acute injury to the retrobulbar optic nerve can be documented by scanning laser polarimetry as well. Injury to retinal ganglion cell axons in the primate visual system leads to ganglion cell death, termed descending degeneration. In squirrel monkeys the decrease in slow axonal transport and the degeneration of ganglion cells following transection of the retrobulbar optic nerve takes place between 3 and 6 weeks after injury.7 Interestingly, only few data regarding the time course of evolving atrophy of the RNFL following acute injury to the optic nerve were publishedin humans: Lundström and Frisen described the funduscopic findings at different stages of descending optic atrophy.8 Their case report describes little change of the RNFL in the first 4 weeks following injury as seen with red-free photography. The RNFL disappeared gradually during weeks 4–8. Recently, measurements of the RNFL using scanning laser polarimetry were reported in a single patient on days 15, 30, 45, and 90 following severe intracanalicular optic nerve trauma.4 The initial measurement 2 weeks after injury appeared normal and even the examination at 30 days was only mildly abnormal before severe decrease of the RNFL occurred.
Using scanning laser polarimetry as well, but at shorter intervals and in a series of five patients, we observed a similar marked decrease of the RNFL thickness during follow up, recorded as changes of the retardation values. The main decrease in RNFL thickness appeared in the first 8 weeks after injury. Subsequent measurements did not reveal further major axonal loss. In our patients degeneration of the RNFL, once started, seemed to follow an exponential curve. However, in patients 2 and 5, an initial unexpected increase of the retardation values was noted within the first 2 weeks. Hypothetically, this finding may represent axonal swelling early in the course of trauma. In contrast with the case reported by Lundström and Frisen,8 and in accordance with the case reported by Medeiros and Susanna,4 we find that decrease in RNFL thickness occurs already within the first 4 weeks after trauma in all patients. We ascribe this to the use of scanning laser polarimetry as opposed to red-free fundus photography. Niessen et al found that a comparison of RNFL assessment by scanning laser polarimetry with standardised red-free photography in 60 glaucoma patients and 24 healthy subjects did not yield equivalent information.9
In conclusion, scanning laser polarimetry may be useful for early detection and documentation of RNFL loss following acute injury to the retrobulbar optic nerve. Of major interest would be to show whether scanning laser polarimetry can help to monitor glaucomatous optic nerve damage in individual patients over time as well.10
Acknowledgments
This study was presented as a poster at the 3rd International Glaucoma Symposium in Prague, Czech Republic, 22–25 March 2001.
The authors do not have any commercial or proprietary interest in the nerve fibre analyser. They do not receive any payment as consultants, reviewers, or evaluators from Laser Diagnostic Technologies, San Diego, CA, USA.
REFERENCES
- 1.Weinreb RN, Shikibo S, Zangwill L. Scanning laser polarimetry to measure the nerve fiber layer of normal and glaucomatous eyes. Am J Ophthalmol 1995;119:627–36. [DOI] [PubMed] [Google Scholar]
- 2.Yamada N, Tomita G, Yamamoto T, et al. Changes in the nerve fiber layer thickness following a reduction of intraocular pressure after trabeculectomy. J Glaucoma 2000;9:371–5. [DOI] [PubMed] [Google Scholar]
- 3.Colen TP, van Everdingen JA, Lemij HG. Axonal loss in a patient with anterior ischemic optic neuropathy as measured with scanning laser polarimetry. Am J Ophthalmol 2000;130:847–50. [DOI] [PubMed] [Google Scholar]
- 4.Medeiros FA, Susanna R Jr. Retinal nerve fiber layer loss after traumatic optic neuropathy detected by scanning laser polarimetry. Arch Ophthalmol 2001;119:920–1. [DOI] [PubMed] [Google Scholar]
- 5.Hollo G, Szabo A, Vargha P. Scanning laser polarimetry versus frequency-doubling perimetry and conventional threshold perimetry: changes during a 12-month follow-up in preperimetric glaucoma. A pilot study. Acta Ophthalmol Scand 2001;79:403–7. [DOI] [PubMed] [Google Scholar]
- 6.Colen TP, Tjon-Fo-sang MJ, Mulder PG, et al. Reproducibility of measurements with the nerve fiber analyzer (NfA/GDx). J Glaucoma 2000;9:363–70. [DOI] [PubMed] [Google Scholar]
- 7.Quigley HA, Davis EB, Anderson DR. Descending optic nerve degeneration in primates. Invest Ophthalmol Vis Sci 1977;16:841–9. [PubMed] [Google Scholar]
- 8.Lundström M, Frisen L. Evolution of descending optic atrophy. A case report. Acta Ophthalmol (Copenh) 1975;53:738–46. [DOI] [PubMed] [Google Scholar]
- 9.Niessen AG, Van Den Berg TJ, Langerhorst CT, et al. Retinal nerve fiber layer assessment by scanning laser polarimetry and standardized photography. Am J Ophthalmol 1996;121:484–93. [DOI] [PubMed] [Google Scholar]
- 10.Lemij HG. The value of polarimetry in the evaluation of the optic nerve in glaucoma. Curr Opin Ophthalmol 2001;12:138–42. [DOI] [PubMed] [Google Scholar]