Abstract
Aim: To present the results of 27 patients who had enucleation for malignant melanoma of the choroid with hydroxyapatite implant wrapped in bovine pericardium.
Method: A retrospective study was performed on 27 patients, 12 males and 15 females, who had enucleation as a primary treatment for their choroidal melanomas. The patients were followed up at 1 week, 1 month, 3 months, and then every 6 months. A conformer was fitted at 1 week and an artificial eye at 1 month. The average follow up was 1.7 years.
Results: No patient had extrusion of the implant. One patient needed repair of the wound, two patients required a lateral tarsal strip, and one patient developed a conjunctival granuloma, which did not need excision. In one patient there was shallowing of the inferior fornix. The cosmetic results and ocular movement were satisfactory in all but one patient.
Conclusion: Use of bovine pericardium as wrapping material for the hydroxyapatite implants has shown promising results with minimal extrusion rates providing an effective alternative for sclera, eliminating the potential risks of CJD.
Keywords: bovine pericardium, melanoma, hydroxyapatite, enucleation
Hydroxyapatite orbital implant has become increasingly popular since its approval in 1989 by the US Food and Drug Administration after being first introduced by Dr Arthur Perry in 1985.1 It is used for enucleations, eviscerations, and secondary socket procedures.2 As a result of the host tissue migrating into the implant it provides low rates of extrusion accompanied by increased mobility of the prosthesis. Sclera3 is the most widely used wrapping materials but because of the risk of Creutzfeldt-Jakob disease (CJD)4 and possibly human immunodeficiency virus (HIV)5 in the United Kingdom efforts are being made to find another suitable alternative. This study describes our experience with 27 patients who had hydroxyapatite implants with bovine pericardium as the wrapping material.
PATIENT AND METHODS
It was a retrospective study of 27 patients between July 1998 and December 1999 who had enucleation for a malignant melanoma of the choroid. All the patients presented to our ocular oncology service and had a full ocular and systemic examination to ensure they had an ocular melanoma without evidence of systemic metastasis.
Enucleation was performed under general anaesthesia by the same surgeon in all cases.
Conjunctival peritomy was followed by the isolation of the four recti muscles with 6-0 Vicryl sutures. The two obliques were then cut. The globe was enucleated with enucleation scissors and homeostasis was maintained by digital pressure with a gauze soaked in warm saline. The time of pressure varied from person to person. The hydroxyapatite implant was wrapped with preformed bovine pericardium wrap (Ocugaurd Supple made by Bio-Vascular Inc, St Paul, MN, USA supplied in UK by John Weizz). The loose ends of the covering were sutured with 6-0 Dacron to ensure adequate coverage and a tight fit on the implant (see Fig 1). The opposite end of the wrapping had incisions in the form of a rectangle corresponding to the recti muscles and the four recti muscle were attached to the loose ends. The Tenon's capsule was sutured over the implant with interrupted 6-0 Vicryl sutures. Conjunctiva was closed with a continuous 8-0 Vicryl suture after Marcain 0.5% (bupivacaine) injection into the sub-Tenon's space. Pressure bandage was applied for about 24 hours and the patient was kept on the ward overnight and discharged home the next day. The patient was then reviewed in 1 week when a conformer was put. After that follow up was at 1 month when a temporary artificial eye was given till the patient received a permanent prosthesis, 3 months, 6 months and then every 6 months. At each visit examination included fitting of the artificial eye, evidence of any wound dehiscence or extrusion of the implant.
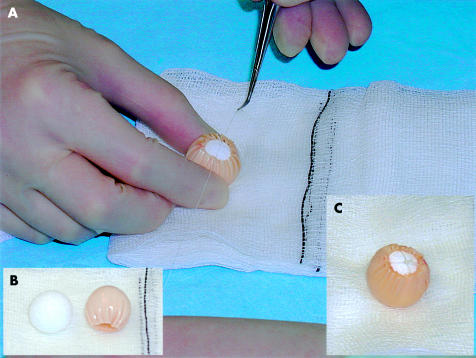
Figure 1.
(A) Hydroxyapatite implant wrapped in bovine pericardium with ends of the wrap being anchored with 6-0 Dacron. (B) The hydroxyapatite implant and the bovine pericardium wrap shown separately. (C) The wrapped implant ready for implantation.
RESULTS
The average age of the patients was 52 years (21–83 years), of which 12 patients were males and 15 were females. None of the patients received any radiation or any form of local therapy preoperatively. The mean follow up was 1.73 years (1.1–2.2 years).
Intraoperative complications included difficult homeostasis in one patient. One patient had a subconjunctival haematoma at 1 week, which settled down on observation. Wound dehiscence, which was subsequently repaired, was noted at 3 months in one patient. Two patients had lower lid laxity for which they underwent lateral canthal slings. One patient had shrinkage of the lower fornix with poor cosmetic results. One patient developed a small conjunctival granuloma but did not need any surgical intervention.
There was no extrusion of the implant in any patient; 26/27 (96%) of the patients achieved an acceptable cosmetic and functional result.
DISCUSSION
Various wrapping material have been used for hydroxyapatite implants as it prevents both the extrusion and exposure of the implant because of the irritating effect of its spicular surface. Sclera6,7 has been the most commonly used material and is obtained from the donor eyes. The decreased willingness of people to donate eyes and also the risk of transmitting life threatening viral infections8 has motivated clinicians to look for other useful alternatives. They include Vicryl mesh (polyglactin 910),9,10 posterior auricular muscle complex grafts,11 rectus abdominis sheath,12 polytetrafluoroethylene,13 and fascia lata14 with varying results.
Bovine pericardium15 has been used in animal models with satisfactory results. Though it is bovine, it is from the American cow thus ensuring that it is free from BSE, which was the main concern motivating us to change from the use of sclera. It is available as a sterilised sealed prepared wrapping material, making its use very easy.
It is sterilised using glutaraldehyde, ethanol, and propylene oxide and has to be immersed and agitated in 500 ml of sterile physiological saline after removal from non-pyrogenic water with propylene oxide in the supply container before wrapping the hydroxyapatite implant.
Exposure rates of hydroxyapatite implant range from 0% to 11%.16,17 Our exposure rate was 1/27 (3.7%) compared to sterile wound dehiscence in 2/14 (14%) cases previously reported.18 The results of motility of the prosthesis were also quite satisfactory, even though we did not drill the hydroxyapatite implant, and the patients were happy with the results.
All our patients tolerated the wrapping of bovine pericardium very well and none had any unusual inflammatory reactions or postoperative complications.
This study has shown promising results with the use of bovine pericardium, which are comparable to the other traditionally used and the more recent, but cumbersome, materials. This study shows that bovine pericardium is a good alternative for wrapping hydroxyapatite implants.
REFERENCES
- 1.Dutton JJ. Coralline hydroxyapatite as an ocular implant. Ophthalmology 1991;98:370–7. [DOI] [PubMed] [Google Scholar]
- 2.Custer PL, Trinkaus KM, Fornoff J. Comparative motility of hydroxyapatite and alloplastic enucleation implants. Ophthalmology 1999;106:513–516. [DOI] [PubMed] [Google Scholar]
- 3.Perry AC. Integrated orbital implants. Adv Ophthalmic Plastic Reconstruct Surg 1990;8:75–81. [PubMed] [Google Scholar]
- 4.Heckmann JG, Lang CJG, Petruch F, et al. Transmission of Creutzfeldt-Jakob disease via a corneal transplant. J Neurol Neurosurg Psychiatry 1997;63:388–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caron MJ, Wilson R. Review of the risk of HIV infection through corneal transplantation in the United States. J Optom Assoc 1994;65:173–8. [PubMed] [Google Scholar]
- 6.Kawai S, Suzuki T, Kawai K. Mobility of hydroxyapatite orbital implant covered with autologous sclera. Jap J Ophthalmol 2000;44:68–74. [DOI] [PubMed] [Google Scholar]
- 7.Kawai S, Tanako T, Suzuki T, et al. Mobility of orbital implant covered by own sclera. Nippon Ganka Gakkai Zasshi 1998;102:193–9. [PubMed] [Google Scholar]
- 8.Seiff SP, Chang JS, Hurt MH, et al. Polymerase chain reaction identification of human immunodeficiency virus-1 in preserved human sclera. Am J Ophthalmol 1994;118:528–30. [DOI] [PubMed] [Google Scholar]
- 9.Jordan DR, Allen LH, Ells A, et al. The use of vicryl mesh (polyglactin 910) for implantation of hydroxyapatite orbital implants. Ophthalmic Plastic Reconstruct Surg 1995;11:95–9. [DOI] [PubMed] [Google Scholar]
- 10.Jordan DR, Klapper SR. Wrapping hydroxyapatite implants. Ophthalmic Surg Lasers 1999;30:403–7. [PubMed] [Google Scholar]
- 11.Naugle TC Jr, Lee AM, Haik BG, et al. Wrapping hydroxyapatite orbital implants with posterior auricular muscle complex grafts. Am J Ophthalmol 1999;128:495–501. [DOI] [PubMed] [Google Scholar]
- 12.Kao SC, Chen S. The use of rectus abdominis sheath for wrapping of the hydroxyapatite orbital implants. Ophthalmic Surg Lasers 1999;30:69–71. [PubMed] [Google Scholar]
- 13.Kao LY. Polytetrafluoroethylene as a wrapping material for a hydroxyapatite orbital implant. Ophthalmic Plastic Reconstruct Surg 2000;16:286–8. [DOI] [PubMed] [Google Scholar]
- 14.Naugle TC, Elliot LF, Sabatier RE. High incision harvesting of fascia lata. Ophthalmic Plastic Reconstruct Surg 1988;4:127. [Google Scholar]
- 15.DeBacker CM, Dutton JJ, Proia AD, et al. Bovine pericardium versus homologous sclera as wrapping materials for hydroxyapatite ocular implants: an animal study Ophthalmic Plastic Reconstruct Surg 1999;15:312–16. [DOI] [PubMed] [Google Scholar]
- 16.Buettner H, Bartley GB. Tissue breakdown and exposure associated with orbital hydroxyapatite implants. Am J Ophthalmol 1992;113:669–73. [DOI] [PubMed] [Google Scholar]
- 17.Remulla HD, Rubin PA, Shore JW, et al. Complications of porous spherical orbital implants. Ophthalmology 1995;102:586–93. [DOI] [PubMed] [Google Scholar]
- 18.Char DH. Early wound dehiscence with use of hydroxyapatite orbital implant covered with calf pericardium. Br J Ophthalmol 2001;85:627–8. [DOI] [PMC free article] [PubMed] [Google Scholar]