Abstract
Background: A new commercially available device (IOLMaster, Zeiss Instruments) provides high resolution non-contact measurements of axial length (using partial coherent interferometry), anterior chamber depth, and corneal radius (using image analysis). The study evaluates the validity and repeatability of these measurements and compares the findings with those obtained from instrumentation currently used in clinical practice.
Method: Measurements were taken on 52 subjects (104 eyes) aged 18–40 years with a range of mean spherical refractive error from +7.0 D to −9.50 D. IOLMaster measurements of anterior chamber depth and axial length were compared with A-scan applanation ultrasonography (Storz Omega) and those for corneal radius with a Javal-Schiötz keratometer (Topcon) and an EyeSys corneal videokeratoscope.
Results: Axial length: the difference between IOLMaster and ultrasound measures was insignificant (0.02 (SD 0.32) mm, p = 0.47) with no bias across the range sampled (22.40–27.99 mm). Anterior chamber depth: significantly shorter depths than ultrasound were found with the IOLMaster (−0.06 (0.25) mm, p <0.02) with no bias across the range sampled (2.85–4.40 mm). Corneal radius: IOLMaster measurements matched more closely those of the keratometer than those of the videokeratoscope (mean difference −0.03 v −0.06 mm respectively), but were more variable (95% confidence 0.13 v 0.07 mm). The repeatability of all the above IOLMaster biometric measures was found to be of a high order with no significant bias across the measurement ranges sampled.
Conclusions: The validity and repeatability of measurements provided by the IOLMaster will augment future studies in ocular biometry.
Keywords: axial length, anterior chamber depth, corneal curvature, partial coherence interferometry
The advent of a new commercially available device which uses partial coherent interferometry (PCI) to measure axial length (IOLMaster, Carl Zeiss Jena GmbH) presents distinct advantages over traditional ultrasound methods of measurement. The IOLMaster does not require contact with the eye and hence avoids risk of corneal abrasion, claims significantly higher resolution measures of axial length compared with ultrasound methods (plus or minus 0.01 mm versus plus or minus 0.15 mm), anterior chamber depth (plus or minus 0.01 mm versus plus or minus 0.15 mm), and has additional facilities to measure corneal curvature (plus or minus 0.01 mm).1,2 Whereas the principal application of the device will be in cataract surgery (the IOLMaster has onboard software menus for the computation of intraocular lens power), the relatively high order of dioptric resolution for axial length (∼plus or minus 0.03 D) is especially valuable in studies of myopia. With regard to the former, PCI has been shown to be independent of cataract grade.3 Concerning the latter, it is well documented that an increase in posterior vitreous chamber depth is the principal structural correlate of myopia,4–7 the IOLMaster is likely to figure significantly in future myopia research. While previous laboratory studies have shown good agreement between PCI and ultrasound methods of measurement,3,8,9 the main purpose of this paper is to compare the reliability and repeatability of data obtained clinically with the IOLMaster with those using a standard applanation ultrasound method of the type employed in many previous studies on myopia. In addition, as the image analysis techniques to measure anterior chamber depth and corneal curvature used by the IOLMaster have not been previously assessed, the accuracy and repeatability of these methods have been examined in this study.
MATERIALS AND METHODS
Fifty two subjects (32 male and 20 female), with a mean age of 25.2 (SD 4.7) years (range 18–40 years, median 23.6 years) participated in the study. Subjects with ocular pathologies, abnormal binocular vision, and previous allergy to the topical anaesthetic benoxinate hydrochloride were excluded from the study. Measurements were performed on 104 eyes by two qualified optometrists (JS-R and EAHM), after the purpose of the study was explained and informed consent given. The monitor of the instrument was used to align the right eye, followed by the left, with the instrument's internal fixation target. The eyes were in focus when the instrument head was approximately 5.5 cm away from the subject's eyes. Subjects were asked to perform a complete blink just before measurements were taken in order to spread an optically smooth tear film over the cornea.
Corneal curvature was measured with the IOLMaster and compared with measures from a videokeratoscope (EyeSys Instruments, Houston, TX, USA) and a Javal-Schiötz keratometer (Topcon, Capelle a/d IJssel, Netherlands). The IOLMaster reflects six points of light, arranged in a 2.3 mm diameter hexagonal pattern (measured by digital callipers), from the air/tear film interface. The separation of opposite pairs of lights is measured objectively by the instrument's internal software and the toroidal surface curvatures calculated from three fixed meridians.10 In comparison, the Javal-Schiötz keratometer requires the user to align the keratometer mires along the principal meridians and corneal curvature is measured by subjective alignment of the mires, reflected from the central 3.4 mm of the cornea. Videokeratography is an image analysis technique for measuring corneal topography with eight concentric rings of light, of known separation and width, reflected from the air/tear film interface. The separation of the 16 ring edges is measured objectively by the internal image analysis software of the instrument, at 1 degree intervals over 360 degrees, over a corneal diameter of 3 mm.11 In addition, an eccentricity value is calculated to indicate the mean rate of corneal flattening using all rings, over a corneal diameter of approximately 9.2 mm.12
Anterior chamber depth was measured with the IOLMaster and compared with measures from an A-scan applanation ultrasound device (Storz Omega Compu-Scan Biometric Ruler, Storz International, St Louis, MO, USA). The IOLMaster directs a 0.7 mm width slit beam of light through the anterior segment of the eye at an angle of 38 degrees to the visual axis. The instrument camera is aligned so that the light beam forms an optical section and the internal software measures the distance between the anterior corneal pole and the anterior crystalline lens surface to calculate the anterior chamber depth. The A-scan applanation device calculates anterior chamber depth from the time taken for ultrasound waves to reflect back to its receiver from an optical surface.13 One drop of topical anaesthetic, benoxinate hydrochloride 0.4% (Minims, Chauvin Pharmaceuticals Ltd), was instilled in each of the subject's eyes 2 minutes before ultrasound measurement. Special care was taken in aligning the transducer beam probe along the optical axis and to exert minimal corneal pressure. Ten measurements were taken for each eye and the mean calculated.
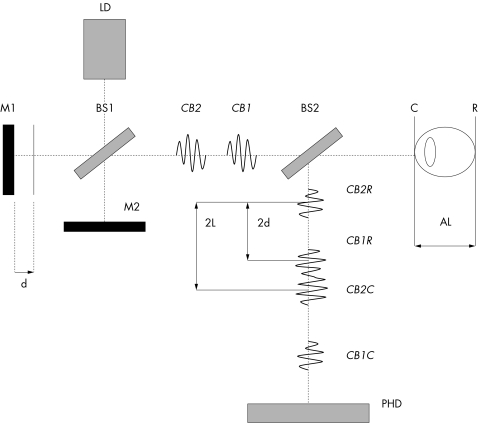
Axial length was measured with the IOLMaster and compared with measures from the A-scan applanation ultrasound device. The IOLMaster measures optical axial length by partial coherence interferometry, based on the Michelson interferometer (Fig 1).9 The laser diode (LD) generates infrared light (λ = 780 μm) of short coherence length (CL= 160 μm), which is reflected into the eye by mirrors M1 and M2, after being split into two equal coaxial beams CB1 and CB2 by the beam splitter B1. The separation of the two coaxial beams is twice the displacement d of the mirror M1. Both coaxial beams enter the eye, where reflections take place at the corneal (C) and retinal (R) interfaces. On leaving the eye, the difference in frequency between the coaxial beams is detected by a photodetector (PHD), after passing through a second beam splitter (BS2). During measurement, the mirror M1 is moved at constant speed, producing a Doppler modulation in the frequency of the reflected coaxial light at the photodetector. The displacement d of the mirror M1 can be precisely determined and related to the reflected signals detected at the photodetector, allowing accurate measurements of the length AL between the cornea and the retina.
Figure 1.
Operating principal of IOLMaster.
Measurements with this device are not affected by longitudinal eye motion.3,9 The calculation of axial length is dependent on the refractive index of the medium in which the light travels, and therefore the optical path length is divided by the mean group refractive index (taken as n = 1.3549) in order to obtain the geometrical axial length.9,14 Laser light is reflected from the retinal pigment epithelium, in contrast with ultrasound waves which are reflected from the internal limiting membrane. Hence, in order to make the IOLMaster results comparable with previous ultrasound measures, a conversion factor has been incorporated into the instrument software.8,9 The A-scan applanation device calculates axial length from the time taken for ultrasound waves to reflect back to its receiver from the internal limiting membrane.13
Three separate measurements were recorded for both axial length and corneal curvature, whereas a single shot automatically generated five measures of anterior chamber depth. In around 5% of subjects, measurements were automatically rejected by the instrument as, compared with the respective mean, they were different by 0.05 mm for corneal curvature, 0.15 mm for anterior chamber depth or the signal to noise ratio (an indicator of measurement quality) for axial length was lower than 2.0. In these cases, an error message was displayed on the monitor and the measure repeated.
Objective refraction was performed with the Shin-Nippon SRW-5000 autorefractor and the mean spherical equivalent calculated from six readings.15 The repeatability of the IOLMaster was examined by measuring corneal curvature, anterior chamber depth, and axial length on the same subjects after a period of 1–10 days from the initial measurement.
Statistical analysis
The bias between measures (the mean difference, standard deviation, and 95% confidence limits) was calculated and presented graphically.16 Comparison between measures was performed using paired two tailed t tests. Corneal curvatures were converted from dioptres into a vector representation in millimetres for analysis17: a spherical lens of power MSE (the mean spherical equivalent = sphere + [cylinder/2]); Jackson cross cylinder at axis 0° with power J0 (= −[cylinder/2] cos[2 × axis]); Jackson cross cylinder at axis 45° with power J45 (= −[cylinder/2] sin[2 × axis]). The level of agreement between biometry measures and ocular refraction was tested using the Pearson's product moment correlation coefficient.
RESULTS
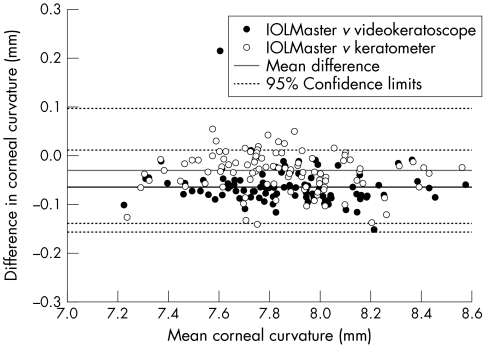
Corneal curvature measurement differences between the IOLMaster, Javal-Schiötz keratometer, and videokeratoscope are shown in Table 1. The mean difference in corneal curvature measured by the IOLMaster was in better agreement with the Javal-Schiötz keratometer than the videokeratoscope, but more variable (Fig 2). The broken lines on the graphs (Figs 2–4) indicate the extent to which the IOLMaster might over-read or under-read compared to the alternative methods examined (that is, the IOLMaster could be expected to read as much as 0.01 mm above or 0.13 mm below the corneal videokeratoscope for mean corneal curvature).
Table 1.
Vector comparison of corneal curvature measurements between the IOLMaster and Javal-Schiötz keratometer and videokeratoscope
| Instrument | Function | Mean difference (mm) | 95% confidence limits |
| Javal | Mean k | −0.03 | 0.13 |
| J0 | 0.01 | 0.11 | |
| J45 | 0.00 | 0.06 | |
| EyeSys | Mean k | −0.06 | 0.07 |
| J0 | −0.01 | 0.08 | |
| J45 | −0.03 | 0.06 | |
Figure 2.
Corneal curvature: difference between IOLMaster measures and Javal-Schiotz keratometer or EyeSys corneal topographer; repeatability of IOLMaster (n=104 eyes).
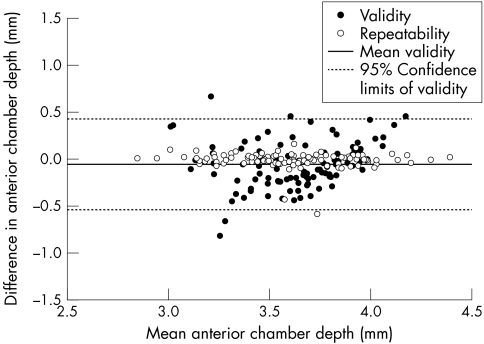
Figure 3.
Anterior chamber depth: difference between IOLMaster and A-Scan ultrasonography; repeatability of IOLMaster (n=104 eyes).
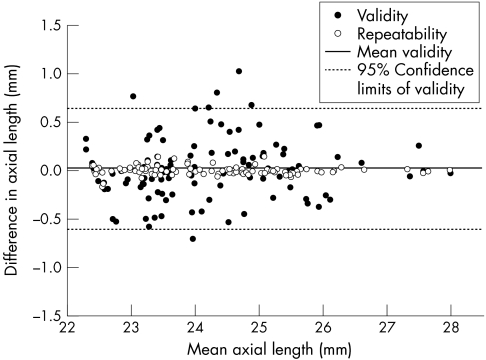
Figure 4.
Axial length: difference between IOLMaster and A-Scan ultrasonography; repeatability of IOLMaster (n=104 eyes).
Anterior chamber depth, as measured with the IOLMaster, was significantly shorter (by −0.06 (0.25) mm, p <0.02) than that measured by applanation ultrasound (Fig 3). There was no significant mean difference (bias) in the accuracy of the instrument for the whole range of anterior chamber depths evident in this study (that is, 2.85–4.40 mm). The IOLMaster could be expected to read as much as 0.43 mm above or 0.54 mm below ultrasound for anterior chamber depth.
Axial length, as measured with the IOLMaster, was similar to that measured by applanation ultrasound (difference 0.02 (0.32) mm, p = 0.47; Fig 4). Again, there was no significant bias in the accuracy of the instrument for the whole range of axial lengths evident in this study (that is, 22.40–27.99 mm). The IOLMaster could be expected to read as much as 0.65 mm above or 0.61 mm below ultrasound for axial length.
The repeatability of corneal curvature measurements made with the IOLMaster are given in Table 2. The mean difference in anterior chamber depth (−0.01 (0.08) mm, p = 0.24; Fig 3) and axial length (0.00 (0.04) mm, p = 0.75; Fig 4) measured with the IOLMaster was insignificant and there was no bias over the whole range. A significant correlation with ocular refraction was found for anterior chamber depth (r = 0.51, p <0.01) and axial length (r = −0.77, p <0.01).
Table 2.
Vector comparison of IOLMaster corneal curvature measurements repeated after an interval of between 1 and 10 days
| Function | Mean difference (mm) | 95% confidence limits |
| Mean k | 0.00 | 0.04 |
| J0 | 0.00 | 0.05 |
| J45 | 0.00 | 0.03 |
DISCUSSION
The study shows that the validity, repeatability, and clinical utility of optical and image analysis methods of assessing ocular biometric measures, match at least those offered by instrumentation currently used in clinical practice and it is envisaged that the IOLMaster will be well received in both the clinical and research environment.
Validity
The close match found between axial length measurements using the IOLMaster and applanation ultrasound (0.02 (0.32) mm) is consistent with those reported previously by Hitzenberger,8 who found a difference between Doppler interferometry and water immersion ultrasonography of 0.01 (0.13) mm. This study has found a closer agreement between PCI and applanation ultrasonography than most of the previous reports.3 The IOLMaster image analysis procedure for measuring anterior chamber depth gave values that closely matched those for applanation ultrasound. Although there was a statistically significant difference between these measures (on average −0.06 mm), this is smaller than the resolution of applanation ultrasound and clinically insignificant (<2% of the anterior chamber depth). IOLMaster measures of corneal curvature were similar to those of keratometry and videokeratoscopy.
Repeatability
The coefficient of repeatability for IOLMaster axial length measurements found in this study (0.00 (0.04) mm) is clearly impressive when compared with those generally found for ultrasound, in which a difference between the first and the mean of three or five readings has been found to be of the order of 0.12 to 0.15 mm.1 Previous studies using optical methods have used the mean standard deviation of single session repeated measures to assess repeatability and reported values of 0.025 mm8 and 0.019 mm.3 The repeatability of anterior chamber depth image analysis measures with the IOLMaster was also good, but slightly more variable than that found for axial length. IOLMaster measures of corneal curvature had repeatability levels similar to those previously reported for keratometry and videokeratoscopy.1,11,18,19
Clinical utility
The facility for taking biometry measurements without the need for corneal contact is a particular advantage in both clinical and research environments and especially in child studies as, once fixation has been achieved, it is claimed that only 0.5 seconds is required to perform a measurement. The significant correlation between axial length and ocular refraction reported in this study is well documented.5,20 In contrast, a weaker, but significant, correlation was found between anterior chamber depth and ocular refraction. Previous studies have failed to support this latter finding.5,21 The IOLMaster currently cannot provide measures of lens thickness but, despite this, its higher level of precision and repeatability for anterior chamber depth may provide further insight into the role of anterior segment dimensions in emmetropisation. Drexler and colleagues22 have developed a non-commercial instrument which uses PCI to measure lens thickness with a precision of 8–10 μm and a resolution of 9 μm and is thus able to monitor temporal change in the accommodation response, but the wavelength of laser light used cannot penetrate the eye as far as the posterior pole for concomitant measures of axial length. Accurate axial length determination is also of particular relevance in the quantitative analysis of fundus structures23,24 such as the optic disc,25,26 the neuroretinal rim area,27,28 and the retinal nerve fibre layer thickness.29
Determination of retinal contour is relevant to our understanding of the mechanisms of eye growth.30–34 Previous studies have determined retinal contour using relatively complex computer software analysis which requires input data obtained from A-scan ultrasonography, keratometry, and peripheral refraction,30,31,35 magnetic resonance imaging,36 or the indirect estimation of retinal contour from peripheral refraction.32,33 Determination of retinal contour with PCI methods has been previously reported for a single individual8 and represents a valuable facility for future studies on posterior segment dimensions. The axial length:corneal radius ratio has been proposed as a biometric predictor for the onset and development of myopia, particularly in children.20,21,37 Examination of the utility of this ratio will be enhanced by the ability of the IOLMaster to provide non-contact, successive, repeatable, high resolution measurements of axial length and corneal radius.
The authors have no proprietary interest in the IOLMaster.
REFERENCES
- 1.Butcher JM, O'Brien C. The reproducibility of biometry and keratometry measurements. Eye 1991;5:708–11. [DOI] [PubMed] [Google Scholar]
- 2.Raj PS, Ilango B, Watson A. Measurement of axial length in the calculation of intraocular lens power. Eye 1998;12:227–9. [DOI] [PubMed] [Google Scholar]
- 3.Hitzenberger CK, Drexler W, Dolezal C, et al. Measurement of the axial length of cataract eyes by laser Doppler interferometry. Invest Ophthalmol Vis Sci 1993;34:1886–93. [PubMed] [Google Scholar]
- 4.Bullimore MA, Gilmartin B, Royston JM. Steady-state accommodation and ocular biometry in late-onset myopia. Doc Ophthalmol 1992; 80: 143–55. [DOI] [PubMed] [Google Scholar]
- 5.Goss DA, Van Veen HG, Rainey BB, et al. Ocular components measured by keratometry, phakometry, and ultrasound in emmetropic and myopic optometry students. Optom Vis Sci 1997;74:489–95. [DOI] [PubMed] [Google Scholar]
- 6.Grosvenor T, Scott R. Comparison of refractive components in youth-onset and adult-onset myopia. Optom Vis Sci 1991;68:204–9. [DOI] [PubMed] [Google Scholar]
- 7.Wildsoet CF. In: Rosenfield M, Gilmartin B, eds. Myopia and nearwork. Oxford: Butterworth-Heinemann, 1998:31–57.
- 8.Hitzenberger CK. Optical measurement of the axial eye length by laser Doppler interferometry. Invest Ophthalmol Vis Sci 1991;32:616–24. [PubMed] [Google Scholar]
- 9.Haigis W, Lege B, Miller N, et al. Comparison of immersion ultrasound biometry and partial coherence interferometry for intraocular lens calculation according to Haigis. Graefes Arch Clin Exp Ophthalmol 2000;238:765–73. [DOI] [PubMed] [Google Scholar]
- 10.Fowler CW. Assessment of toroidal surfaces by the measurement of curvature in three fixed meridians. Ophthal Physiol Opt 1989;9:79–80. [DOI] [PubMed] [Google Scholar]
- 11.Dave T, Ruston D, Fowler C. Evaluation of the EyeSys model II computerized videokeratoscope. Part I: Clinical assessment. Optom Vis Sci 1998;75:647–55. [DOI] [PubMed] [Google Scholar]
- 12.Nieves J, Applegate RA. Alignment errors and working distance directly influence the accuracy of corneal topography measurements. [ARVO Abstract] Invest Ophthalmol Vis Sci 1992;33:993 (Abstract no 1509).
- 13.Storey JK, Rabie EP. Ultrasound-a research tool in the study of accommodation. Ophthal Physiol Opt 1983;3:315–20. [PubMed] [Google Scholar]
- 14.Fercher AF. Optical coherence tomography. J Biomed Opt 1996;1:157–73. [DOI] [PubMed] [Google Scholar]
- 15.Mallen EAH, Wolffsohn JS, Gilmartin B, et al. Clinical evaluation of the Shin-Nippon SRW-5000 autorefractor in adults. Ophthal Physiol Opt 2001;21:101–7. [PubMed] [Google Scholar]
- 16.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–10. [PubMed] [Google Scholar]
- 17.Thibos LN, Wheeler W, Horner D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci 1997;74:367–75. [DOI] [PubMed] [Google Scholar]
- 18.Dave T, Ruston D, Fowler C. Evaluation of the EyeSys model II computerized videokeratoscope. Part II: The repeatability and accuracy in measuring convex aspheric surfaces. Optom Vis Sci 1998;75: 656–62. [DOI] [PubMed] [Google Scholar]
- 19.Vámosi P, Sohajda Z, Módis L, et al. Comparison of different keratometers with the EyeSys videokeratoscope. Acta Ophthalmol 1998;76:158–64. [DOI] [PubMed] [Google Scholar]
- 20.Grosvenor T, Scott R. Role of the axial length/corneal radius ratio in determining the refractive state of the eye. Optom Vis Sci 1994;71:573–9. [DOI] [PubMed] [Google Scholar]
- 21.Grosvenor T, Scott R. Three-year changes in refraction and its components in youth-onset and early adult-onset myopia. Optom Vis Sci 1993;70:677–83. [DOI] [PubMed] [Google Scholar]
- 22.Drexler W, Baumgartner A, Findl O, et al. Biometric investigation in the anterior eye segment during accommodation. Vis Res 1997;37: 2789–800. [DOI] [PubMed] [Google Scholar]
- 23.Littmann H. The determination of the true size of objects in the background of the fundus. Klin Monatsbl Augenheilkd 1982;180:286–92. Translated by TD Williams [classical article]. Optom Vis Sci 1992;69: 717–20.7087358 [Google Scholar]
- 24.Bennett AG, Rudnicka AR, Edgar DF. Improvements on Littmann's method of determining the size of retinal features by fundus photography. Graefes Arch Clin Exp Ophthalmol 1994;232:361–7. [DOI] [PubMed] [Google Scholar]
- 25.Bengtsson B, Krakau CET. Correction of optic disc measurements on fundus photographs. Graefes Arch Clin Exp Ophthalmol 1992;230:24–8. [DOI] [PubMed] [Google Scholar]
- 26.Garway-Heath DF, Rudnicka AR, Lowe T, et al. Measurement of optic disc size: equivalence of methods to correct for ocular magnification. Br J Ophthalmol 1998;82:643–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Caprioli J, Miller JM. Correlation of structure and function in glaucoma. Quantitative measurements of disc and field. Ophthalmology 1988;95:723. [DOI] [PubMed] [Google Scholar]
- 28.Jonas JB. Optic disc morphometry in chronic primary open angle glaucoma. Graefes Arch Clin Exp Ophthalmol 1988;226:531–8. [DOI] [PubMed] [Google Scholar]
- 29.Caprioli J, Ortiz-Colberg R, Miller JM, et al. Measurements of peripapillary nerve fibre layer contour in glaucoma. Am J Ophthalmol 1989;108:404–13. [DOI] [PubMed] [Google Scholar]
- 30.Dunne MCM. A computing scheme for determination of retinal contour from peripheral refraction, keratometry and A-scan ultrasonography. Ophthal Physiol Opt 1995;15:133–43. [PubMed] [Google Scholar]
- 31.Logan NS, Gilmartin B, Dunne MC. Computation of retinal contour in anisomyopia. Ophthal Physiol Opt 1995;15:363–6. [PubMed] [Google Scholar]
- 32.Seidemann A, Guirao A, Artal P, et al. Relation of peripheral refraction to refractive development? [ARVO Abstract] Invest Ophthalmol Vis Sci 1999;40:S448 (Abstract no 2362).
- 33.Love J, Gilmartin B, Dunne MCM. Relative peripheral refractive error in adult myopia and emmetropia. [ARVO Abstract] Invest Ophthalmol Vis Sci 2000;41:S302 (Abstract no 1592).
- 34.Mutti DO, Sholtz RI, Friedman NE, et al. Peripheral refraction and ocular shape in children. Invest Ophthalmol Vis Sci 2001;41:1022–30. [PubMed] [Google Scholar]
- 35.Logan NS, Gilmartin B, Wildsoet CF, et al. Asymmetry of schematic retinal contour in anisomyopia. [ARVO Abstract] Invest Ophthalmol Vis Sci 1995;36:S949 (Abstract no 4373).
- 36.Cheng HM, Singh OS, Kwong KK, et al. Shape of the myopic eye as seen with high-resolution magnetic resonance imaging. Optom Vis Sci 1992;69:698–701. [DOI] [PubMed] [Google Scholar]
- 37.Grosvenor T. High axial length/corneal radius ratio as a risk factor in the development of myopia. Optom Vis Sci 198;65:689–96. [DOI] [PubMed]