Abstract
Aim: To evaluate the complications associated with pegging of porous hydroxyapatite orbital implants.
Methods: Complications associated with pegging were retrospectively reviewed from the charts of 100 of 133 patients with hydroxyapatite implantation from 1993 to 2000.
Results: 48 (48%) of the 100 hydroxyapatite implanted patients who had undergone pegging were found to have problems with their pegs, including discharge (45.8%), peg falling out (20.8%), pyogenic granulomas (16.7%), popping peg (14.6%), hydroxyapatite visible around peg hole (8.3%), part of peg shaft visible (6.2%), peg drilled off centre (6.2%), peg drilled at an angle (4.2%), and excess movement of peg (4.2%). The standard peg fell out statistically more often than the peg and sleeve system (Yates's corrected χ2, p=0.038). There was a trend towards complications of the peg with use of a standard peg (versus sleeved peg) (p=0.226).
Conclusions: There are several potential complications of pegging. Most complications are minor and can be managed successfully.
Keywords: hydroxyapatite implant, peg complications
The porous hydroxyapatite implant is the artificial ocular motility implant designed to provide natural movement of the artificial eye.1 It enables the orbital soft tissue to grow into the porous implant and produce a true integrated status within the orbit. The movement of the prosthesis is maximised when the implant is coupled to the prosthesis via a peg.2 In this report, we assess the complications of peg placement in hydroxyapatite orbital implants and evaluate the factors associated with these complications.
MATERIALS AND METHODS
We retrospectively reviewed all patients who received a hydroxyapatite orbital implant (the Bio-Eye Implant; Integrated Orbital Implant Inc, San Diego, CA, USA) after enucleation, evisceration, or secondary implantation by the oculoplastic team. All the patients who had undergone the pegging procedure were included in our study. The recorded information included patient age, sex, the eye involved, ocular diagnosis before the surgery, and previous ocular surgery or radiotherapy. The size of the implant, the type of ocular implant, and complications associated with the pegging procedure were recorded. The time interval from the implantation and peg placement, preoperative assessment of implant vascularity via a technetium-99 bone scan before peg placement, the type of peg system, and problems during the follow up period were also recorded. A statistical analysis of these variables with Yates's corrected χ2 was performed.
Peg placement was performed in the operating room under sterile conditions. In adults the pegging procedure was performed under retroimplant local anaesthesia; in children it was performed under general anaesthesia. In the supine position, the patient was prepared and draped, and then a lid speculum was positioned. The conjunctiva and subconjunctival tissues were grasped with forceps to stabilise the implant. We used an 18 gauge needle to start the hole with the needle perpendicular to the anterior plane of the orbit. A hand held drill (supplied by Integrated Orbital Implant Inc, San Diego, CA, USA) was used to enlarge the drill hole with either a 3.0 mm drill bit for the standard peg or a 3.8 mm drill bit for sleeved pegs. The needles and drill bit were simply rolled between the thumb and index finger with gentle downward pressure.
Once the hole was made, the standard peg (Integrated Orbital Implant, Inc) or the peg and sleeve system (Integrated Orbital Implant, Inc) was used. We used the standard peg before 1995 and changed to the peg and sleeve system after 1995. Both peg systems were made from high temperature polycarbonate. The standard peg system consisted of only a peg. The peg and sleeve system consisted of a threaded unidirectional sleeve to be screwed into the implant and a central peg. If a standard peg was used, it was placed directly in the drilled vestibule, and the conjunctival edges were tucked under the peg to encourage growth of conjunctiva along the peg vestibule wall. If a peg and sleeve system was used, the sleeve was then screwed into the drilled vestibule, and a temporary peg was placed within the sleeve. Then it was covered by the conformer, antibiotic ointment, and dressing. Four weeks later, the temporary peg was replaced with a permanent peg.
RESULTS
A total of 133 patients received a hydroxyapatite orbital implant between August 1992 and December 1999; 100 of them underwent a peg placement. Among the 100 patients with peg placement, 68 had undergone enucleation, 22 patients had undergone evisceration, and 10 patients had received a hydroxyapatite implant as a secondary or exchange procedure. Among the 33 patients who did not receive peg placement, 20 were lost of follow up and 13 patients felt satisfied with prosthesis and did not want to be pegged.
The ages ranged from 4 to 79 years, with a mean of 37 years. There were 63 males and 37 females. The affected eye was the right eye in 53 cases and the left in 47 cases. The reasons for surgery are shown in Table 1. The majority of implants placed were 20 mm in diameter. The time interval from surgery to pegging ranged from 5 to 32 months in primary patients, with a mean of 9.8 months. In the secondary implant group, the range was from 6 to 26 months, with a mean of 11.0 months (Table 2).
Table 1.
Reasons for hydroxyapatite orbital implantation (100 patients)
| Diagnosis | No of patients | % |
| Phthisis bulbi | 44 | 44 |
| Retinoblastoma | 16 | 16 |
| Painful, blind eye | 16 | 16 |
| Endophthalmitis | 12 | 12 |
| Choroidal melanoma | 4 | 4 |
| Silicone ball exposure | 3 | 3 |
| Eyeball rupture | 2 | 2 |
| Secondary anophthalmos | 1 | 1 |
| Silicone ball infection | 1 | 1 |
| Silicone ball exchange | 1 | 1 |
Table 2.
Background information of hydroxyapatite orbital implantation (Bio-Eye)
| HA implantation | 133 |
| Peg placement | 100 |
| Type of surgery | |
| Enucleation | 68 |
| Evisceration | 22 |
| Secondary implant | 10 |
| Previous ocular surgery | |
| Yes | 67 |
| No | 33 |
| Prior radiotherapy | |
| Yes | 0 |
| No | 100 |
| Implant size used | |
| 16 mm | 2 |
| 18 mm | 14 |
| 20 mm | 84 |
| Type of peg used | |
| Original standard peg | 17 |
| Peg and sleeve | 83 |
| Average time to peg (months) | |
| Primary implantation | 9.8 (5∼32) |
| Secondary implantation | 11.0 (6∼26) |
A bone imaging for ocular implant with technetium-99m MDP 20 mCi was performed in 70 patients before peg placement (70%), at a mean interval of 6 months from hydroxyapatite implantation. The implant to mid-facial bone ratio was more than or equal to 0.8 in 50 patients (71.4%) and less than 0.8 in 20 (28.6%).
Seventeen patients received the original standard peg before 1995, and 83 patients received the peg and sleeve system. The main complications of peg placement are shown in Table 3. Thirty six patients had only one complication and 12 patients had more than one complication.
Table 3.
Problems associated with peg systems (48 patients with hydroxyapatite implant)
| Problem | No of patients | % |
| Discharge (22 (45.8%)) | ||
| Minor/recurrent | 19 | 39.6 |
| Major | 3 | 6.2 |
| Peg falling out (10 (20.8%)) | ||
| With overgrowth of hole | 5 | 10.4 |
| With hole remaining open | 5 | 10.4 |
| Pyogenic granulomas (8 (16.7%)) | ||
| Around peg hole | 8 | 16.7 |
| Within hole | 0 | |
| Popping peg | 7 | 14.6 |
| Hydroxyapatite visible around peg hole | 4 | 8.3 |
| Part of peg shaft visible | 3 | 6.2 |
| Peg drilled off centre | 3 | 6.2 |
| Peg drilled at an angle | 2 | 4.2 |
| Excess movement of peg | 2 | 4.2 |
DISCUSSION
Porous hydroxyapatite has been successfully used as an orbital implant in enucleation, evisceration, and as secondary implants since 1985.2 With drilling and peg placement, these implants can be directly coupled to the prosthesis, allowing a fine prosthetic movement. However, several early and late complications have been reported with the hydroxyapatite peg system. The complications of motility peg placement for the hydroxyapatite orbital implant have been reported including discharge, pyogenic granuloma, peg falling out, poor transfer of movement, clicking, conjunctiva overgrowing peg, poor fitting sleeve, part of sleeve shaft visible, peg drilled on an angle, hydroxyapatite visible around peg hole, peg drilled off centre, popping peg, conjunctival oedema, excessive postoperative pain, excessive movement of peg, and a broken peg.3–14 The most serious complication reported was implant infection requiring implant removal.3
This report is the second largest review of complications occurring with the peg system of hydroxyapatite ocular implant to date. Jordan et al reported that 57 (42%) of 135 patients with Bio-Eye implants had problems.3 Among the 100 patients who received peg placement in our series, 48 (48%) had one or more complications. The complication rate was slightly greater than that reported in previous studies (22.0%–46%).3–5 However, most complications were of a minor nature and no implant infection was noted. In general, the list of complications in our study is similar to that reported by Jordan et al.3
As described in Table 3, discharge was the most common complication, occurring in 22 patients (45.8%). In Jordan's series, discharge is also the most common complication (37%). According to the definition of Jordan et al,3 we included patients who had discharge from the onset of their pegging or those who had increased discharge after pegging. Discharge was classified as minor and major. Minor discharge occurred in 19 patients intermittently but on a recurrent basis. It was generally suppressed with an antibiotic steroid drop. Major discharge occurred regularly and was quite bothersome for the patient and family. The three patients with major discharge were all children with retinoblastoma. Among them, the persistent discharge resolved after peg removal in two patients. In the other patient, the discharge made the peg fall out with hole remaining open. The relatively higher temperature in subtropical climates and the difficulties in postoperative wound care of children may be blamed for the increased discharge.
The peg falling out (Fig 1) was the next common problem, occurring in 10 patients (20.8%). The standard peg fell out (five in 17) statistically more often (Yates's corrected χ2, p=0.038) than the peg and sleeve system (five in 83) because the sleeve had a tighter fit with the implant. A structural barrier was present with the peg and sleeve system to block the proliferation of granulation tissue in the base of the vestibule.4,11 So overgrowth of the hole when the peg fell out occurred more often with the standard peg system but also occurred with the sleeve system in one case.
Figure 1.
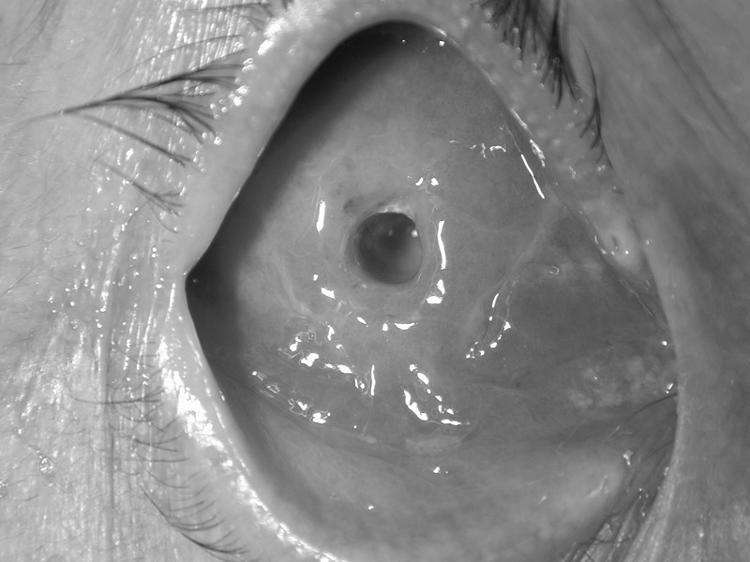
Peg falling out with hole remaining open.
Pyogenic granulomas (Fig 2) were the third most common problem that occurred in eight patients (16.7%). They were seen with both peg systems (one in standard peg and seven in peg with sleeve) and all occurred around the peg hole. Only for those pyogenic granulomas that caused peg displacement did we perform simple excision with cauterisation of the base. We did not use mitomycin C to the base of the pyogenic granuloma after its removal to prevent its recurrence.9 The pyogenic granuloma is the next common problem in Jordan's series. Because the hydroxyapatite is brittle,12,13 the less secure attachment of the peg may cause movement of the peg in the implant, which in turn induce conjunctival irritation and granuloma formation.13
Figure 2.
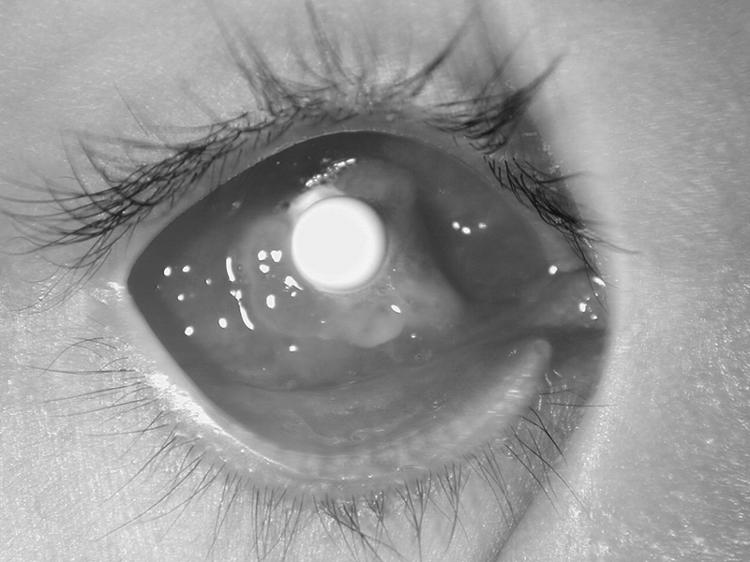
Pyogenic granulomas.
The popping peg phenomenon occurred in seven patients (14.6%) because there was too much subconjunctival tissue present.14 The peg could be pushed into the hole but tended to pop out gradually. Debulking the subconjunctival tissue corrected the problem in one patient.
A number of other complications occurred less often. Hydroxyapatite exposure around the drill site was seen in four patients (8.3%): three occurred with the standard peg and one with the sleeve system. After long term follow up, the exposure resolved without aggressive management and no implant infection was noted. The peg drilled off centre occurred in three patients (6.2%) which caused slight esotropia. Excessive movement of the standard peg occurred in two patients (4.2%) and was due to drilling a hole that was too big. We removed the standard peg and used the sleeve system.
Having part of the peg shaft visible (Fig 3) occurred in three patients (6.2%) as a result of the shaft not being deep enough beneath the conjunctival surface. However, this did not create a fitting problem. In two patients (4.2%), the drill hole was at an angle; because it did not cause discomfort, it was left alone.
Figure 3.

Part of peg shaft visible.
Complications we have not seen to date are poor transfer of movement, clicking, conjunctiva overgrowing peg, poor fitting sleeve, persistent pain, persistent oedema, a broken peg, and implant infection.3,4,8 Though it was not statistically significant (Yates's corrected χ2, p=0.226), the standard peg system seemed to have a greater incidence of complications (13 in 17, 76.5%) compared to the peg and sleeve system (35 in 83, 42.2%), including peg falling out with overgrowth of hole, part of the peg shaft visible, hydroxyapatite visible around peg hole, and excessive movement of peg. For those reasons, we have started to use a peg and sleeve system since 1995. The recent reviews also document that complications occurred more frequently with the standard system.3,4
In conclusion, pegging of the porous hydroxyapatite ocular implants may improve the range of prosthetic movement, but the peg placement has potential problems. Sleeved pegs seem to have fewer problems. Fortunately, most complications are of a minor nature and can be managed successfully. However, these potential problems should be discussed with the patient before pegging.
Acknowledgments
Statistical consultation provided by Huan-Sheng Chen, MD.
The authors have no direct financial interest in any of the products mentioned in this article, nor are they paid consultants for any companies mentioned.
REFERENCES
- 1.Hornblass A, Biesman BS, Eviatar JA. Current techniques of enucleation: a survey of 5,439 intraorbital implants and a review of the literature. Ophthal Plast Reconstr Surg 1995;11:77–88. [PubMed] [Google Scholar]
- 2.Perry AC. Advances in enucleation. Ophthal Plast Reconstr Surg 1991;4:173–82. [Google Scholar]
- 3.Jorden DR, Chan S, Mawn L, et al. Complications associated with pegging hydroxyapatite orbital implants. Ophthalmology 1999;106:505–12. [DOI] [PubMed] [Google Scholar]
- 4.Edelstein C, Shields CL, Potter PD, et al. Complications of motility peg placement for the hydroxyapatite orbital implant. Ophthalmology 1997;104:1616–21. [DOI] [PubMed] [Google Scholar]
- 5.Ashworth J, Brammar R, Inkster C, et al. A study of the hydroxyapatite orbital implant drilling procedure. Eye 1998;12:37–42. [DOI] [PubMed] [Google Scholar]
- 6.Georgiadis NS, Terzidou CD, Dimitriadis AS. Coralline hydroxyapatite sphere in orbit restoration. Eur J Ophthalmol 1999;9:302–8. [DOI] [PubMed] [Google Scholar]
- 7.Remulla HD, Rubin PAD, Shore JW, et al. Complications of porous spherical orbital implants. Ophthalmology 1995;102:586–93. [DOI] [PubMed] [Google Scholar]
- 8.Oestreicher JH, Liu E, Berkowitz M. Complications of hydroxyapatite orbital implants. A review of 100 consecutive cases and a comparison of Dexon mesh (polyglycolic acid) with scleral wrapping. Ophthalmology 1997;104:324–9. [DOI] [PubMed] [Google Scholar]
- 9.Popp JC. The use of mitomycin C for the treatment of pyogenic socket granulation tissue associated with motility pegs. J Ophthal Prosth 1996;98:370–7. [Google Scholar]
- 10.Shields CL, Shields JA, De Potter P, et al. Problems with hydroxyapatite orbital implant: experience with 250 consecutive cases. Br J Ophthalmol 1994;78:702–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kolberg GI. The hydroxyapatite (Bio-Eye) implant. A histological perspective. J Ophthal Prosth 1996;1:29–36. [Google Scholar]
- 12.Goldberg RA, Holds JB, Ebrahimpour J. Exposed hydroxyapatite ocular implants. Report of six cases. Ophthalmology 1992;99:831–6. [DOI] [PubMed] [Google Scholar]
- 13.Choi JC, Iwamoto MA, Bstandig S, et al. Medpor motility coupling post: a rabbit model. Ophthal Plast Reconstr Surg 1999;15:190–201. [DOI] [PubMed] [Google Scholar]
- 14.Jordan D. The popping peg phenomenon [letter]. Arch Ophthalmol 1994;112:300–1. [DOI] [PubMed] [Google Scholar]


