Abstract
Aims: In order to establish normal values and interocular differences of visual acuity, Lea symbols were applied to neurologically and ophthalmologically normal children.
Methods: 385 children (21–93 months old) were examined, within a routine check up in an urban paediatric practice where Lea symbol acuity (LS) was measured. Of these children, 90 were re-examined in hospital comparing Lea symbol acuity (LS) and Landolt C acuity (LC). Strabismus, ametropia, and any organic eye disease were excluded.
Results: In the paediatric practice, LS could be measured on both eyes in 54% of the children. In the age group above 36 and 48 months the success rate was 76% and 95%, respectively. Acuity in the paediatric practice ranged from 0.1 to 2.0 (median 1.25) in the whole group. Interocular acuity difference was one line or less in 80%. In the hospital, LS and LC could be measured on both eyes of 77% and 48% of the 90 children, respectively. Cooperation increased with age. LS in the hospital ranged from 0.32 to 2.0 (median 1.0) and LC from 0.16 to 1.25 (median 0.8). Interocular difference of LS acuity was one line or less in 90%.
Conclusion: Lea symbols were found to be useful for visual acuity assessment in early childhood. Significant variability of visual acuity in this age group is caused by cooperation. When monocular measurements are possible on both eyes, however, the intraindividual interocular difference of visual acuity usually does not exceed one line.
Keywords: Lea symbols, children, amblyopia, visual acuity
Early measurement of visual acuity1,2 is desirable in order to detect amblyopia and to control its treatment. Severe amblyopia as caused by stimulus deprivation can be detected even in infancy by preferential looking.3–6 However, the sensitivity of preferential looking for refractive and strabismus amblyopia is limited.7 In amblyopia, recognition acuity is more severely reduced than grating acuity or detection acuity.8 Therefore, in cooperative patients, assessment of recognition acuity is more sensitive. Yet, optotypes are usually not applicable before the age of 3 years, and picture charts9 which may already be known by younger children are hardly standardised. Lea symbols10,11 combine the advantages of optotypes and pictures. They are well standardised and can be given names by 2 year old children.12 The Lea tests use three symbols, a house, an apple, and a square (Fig 1), differing in few critical details from the fourth symbol, which is a circle. Below the threshold of recognition, each symbol appears as a small circle. The test is graded in decadic logarithmic steps (lines) from 0.1 to 2.0 at a distance of 3 metres. It is available in single symbol and crowded symbol versions.
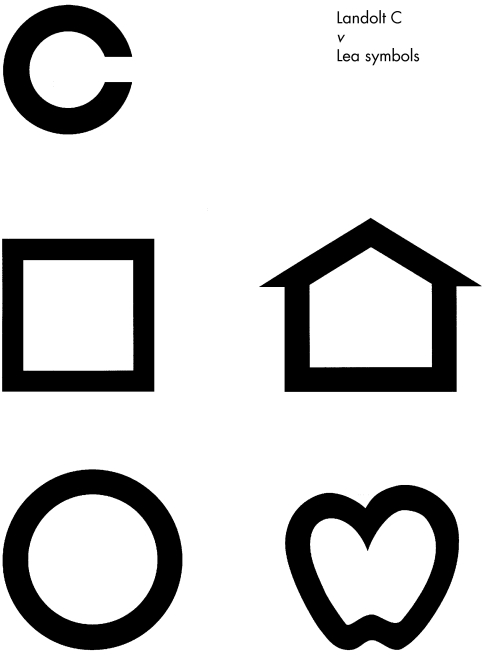
Figure 1.
Lea symbols compared with the Landolt C corresponding to the same visual acuity. The diameter of the Lea symbols is about 20% larger than the diameter of the corresponding Landolt C. While the Landolt C contains only one critical detail (the gap), the house, apple, and square differ from the circle in more details.
Visual acuity tests are calibrated against the Landolt C which is the standard optotype.13 The calibration is performed at a high acuity level. At low levels, the acuity values using various optotypes can differ significantly from the visual acuity as measured by the Landolt C. Particularly in amblyopic eyes, letters are easier to recognise than a Landolt C of the corresponding size.14 Fortunately, there is only a little difference between Lea symbol acuity and the Landolt C acuity even in strabismus amblyopia15 and Lea symbols showed a high sensitivity for amblyopia,16,17 which could be shown in previous examinations on amblyopic older children and adults. In the present study we examined healthy children in order to establish age related normal values of Lea symbol acuity and to compare the results of acuity assessment during a paediatric examination (performed to detect amblyopia) and an ophthalmological re-examination.
PATIENTS AND METHODS
Paediatric examination
In total, 385 children who came to a paediatric practice in Giessen in 1999 were included. In the practice, the parents were informed about the study and asked to answer a questionnaire. The questionnaire asked for family history (strabismus, ametropia), general disorders, and eye disorders of the child, and premature birth. Lea single symbol acuity (LS) was assessed by repeatedly instructed staff (through RB and MG) using a Lea Symbols Single Symbol Book (Precision Vision, catalogue no 2506). The examination distance was 3 metres and a 3/4 criterion was prescribed, always starting at a well recognisable level where the child instantly answered. If the first three questions at that level were answered correctly, the next (higher) line was used. If only two of the three symbols were answered correctly, the fourth symbol was asked. If this symbol was answered correctly, we proceeded to the next line. If there were fewer than three correct answers, the previous line—that is, the highest level where at least three of four symbols were named correctly was taken as visual acuity. If an answer was wrong, “second chances” were not allowed. Both eyes were examined separately. Care was taken that the other eye was completely occluded. In addition, the Lang stereotest18 was applied. The fundus red reflex test19 and the Hirschberg test were performed by the paediatrician. After the parents' informed consent was obtained, we arranged an appointment for re-examination in our department.
Ophthalmological examination
In our department, acuity was also assessed with the Lea Symbols Single Symbol Book (LS). The children were also examined monocularly on both eyes, if possible. Additionally, the Lea 15 Line Folding Distance Chart (Precision Vision, catalogue no 2501), containing crowded Lea symbols, was used (CLS). In this chart, the interoptotype distances relate to the size of the symbols. Both LS and CLS were determined at a distance of 3 metres. Furthermore, Landolt C acuity was determined with test charts20 containing Landolt Cs with four alternative straight directions in single (LC) and crowded arrangement with 2.6 minutes of arc interoptotype distance (LC2.6). The Landolt C test charts were applied at a distance of 5 metres where the decadic logarithmic calibration ranges from 0.16 to 1.25. For each visual acuity test, a 3/4 criterion always starting at a well recognisable level following the same forced choice procedure as described above was used. The order of the visual acuity tests followed a pseudorandomised protocol so that there was an equal chance to start testing either with Lea symbols or with the Landolt C. Within the same symbols, single symbols (LS, LC) preceded crowded symbols (CLS, LC2.6). Strabismus and any organic eye disease were excluded by thorough ophthalmological examination including biomicroscopy, indirect ophthalmoscopy, refractometry or retinoscopy, cover test, assessment of ocular motility, fundus red reflex test,19 Hirschberg test, and the Lang stereotest18 performed by RB or SH. Refractometry or retinoscopy were performed in cycloplegia, if the parents agreed. Examinations in our department took about one and a half hours for all measurements including history, cycloplegia, and little breaks for playing and speaking with the children.
For visual acuity results in the paediatric practice and within the ophthalmological examination, the 0.10 (α0.1), 0.25, 0.50, 0.75, and 0.90 quantiles for the “better” eye of each child and the cooperation rates were calculated.
RESULTS
Paediatric practice
Of the 385 children (male 172, female 213) aged 21–93 months (median 47 months), 126 (33%) had visited an ophthalmologist at least once before, 15 (4%) wore glasses, and nine (2.3%) had received occlusion therapy. Random dot stereopsis was proved in 297 children (77%, median 48 months). The remaining children (median 25 months) did not respond to the Lang stereotest. Six children showed minor, non-amblyogenic ocular changes (suspected ptosis, haemorrhage of eyelid, entropium, head turn, small haemangioma, intermittent exotropia). In 2% of the families, strabismus was known, in 52% at least one of the parents had glasses.
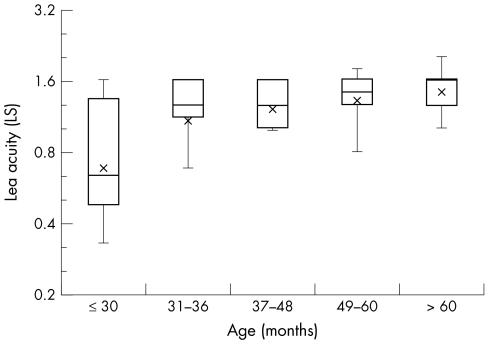
In 208 children (54%) Lea single symbol acuity was determined monocularly on both eyes. Results of visual acuity measurements with Lea symbols are presented in the form of box plots for the better eye of each child (Fig 2). In 17% of the 208 children, the measured acuity differed between both eyes by more than one line (maximum four lines). Cooperation for monocular examination on both eyes was only 8% for the 156 children aged ≤30 months. In the age group 31–48 months, cooperation improved from 56% below 36 months to 76% above 36 months. More than 90% of children older than 48 months showed cooperation. The 10% quantile for visual acuity of the “better” eyes was 0.32 for children ≤30 months. Between 30 and 36 months of age, there was a rapid increase. In the age groups >36 months, the 10% quantiles for visual acuity of the “better” eyes were 0.8 to 1.0. An interocular difference of LS >1 line was found in up to 20% of the children independent of age (Table 1).
Figure 2.
Box plots of Lea single symbol acuity (“better” eye of each child) of 208 children examined monocularly on both eyes in the paediatric practice.
Table 1.
Cooperation (determination of monocular visual acuity of both eyes possible) of 385 children coming to a paediatric routine examination. 10% quantiles (α0.1) for visual acuity (Lea single symbols) of the “better” eye of each child and children who had an acuity difference >1 line between both eyes
| Age (months) | No | Cooperation/rate | α0.1 | Difference >1 line |
| 21–30 | 156 | 13 (8%) | 0.32 | 2 (15%) |
| 31–36 | 16 | 9 (56%) | 0.63 | 0 (0%) |
| 37–48 | 71 | 54 (76%) | 1.0 | 6 (11%) |
| 49–60 | 63 | 60 (95%) | 0.80 | 15 (25%) |
| 60–93 | 79 | 72 (91%) | 1.0 | 13 (18%) |
| 21–93 | 385 | 208 (54%) | 0.80 | 36 (17%) |
Ophthalmological examination
Of the 385 children it was possible to re-examine 90 (23%) in our department. These children were 23–70 months old (median 42.5 months). The parents of the remaining 295 children either did not agree to the ophthalmological re-examination (65%) or failed to come to their appointment (15%). Fifty eight parents (20%) could not be reached by phone despite several attempts; 75% of the children who had never before been ophthalmologically examined did not appear for re-examination. Of the 90 children (41 male, 49 female) re-examined in our department, 29, nearly the same rate as in the entire group, had undergone an ophthalmological examination at least once before, and 58% of the parents mentioned a history concerning eye disorders (glasses 49, strabismus two, red-green deficiency one) in the family. Of their children, 48% had had contact with an ophthalmologist before. Two children (2.2%) wore glasses (for comparison: of those children who did not appear for the ophthalmological examination, 33% had also had contact with an ophthalmologist before and 4.4% wore glasses). Thirty two children did not receive cycloplegia because of their parents' refusal. None of these 32 children nor the 58 children checked under cycloplegia showed a significant refractive error (>3 D sph, >1.5 D cyl). Random dot stereopsis was proved in 87 children (97%), three children did not respond to the Lang stereotest (median 29 months). Of the re-examined children, only 71 (82.5%) had shown random dot stereopsis in the paediatric practice.
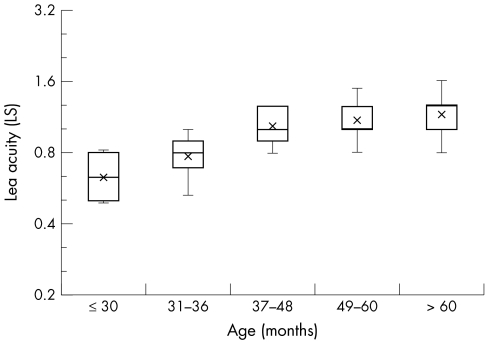
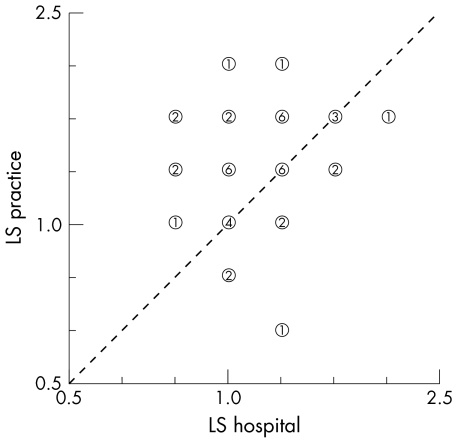
As Table 2 shows cooperation in the Lea symbol test increased with age. An interocular difference of LS more than one line occurred mainly in children below 36 months of age. In this age group, the 10% quantile of LS was 0.5, while above 36 months, it was 0.8. While the LS of the entire group (median age 47 months) and the re-examined children were similar (Figs 2 and 3), for those 42 children who both in the practice and in the hospital (median age 42.5 months) cooperated in visual acuity assessment, LS of the “better” eye measured in the practice surpassed LS measured in our department by 1.3 lines. In Figure 4 LS measured in the practice is plotted against LS measured in our department.
Table 2.
Cooperation (determination of monocular visual acuity of both eyes possible) of the 90 children re-examined in the hospital, 10% quantiles (α0.1) for visual acuity (Lea single symbols) of the “better” eye of each child and children who had an acuity difference >1 line between both eyes
| Age (months) | No | Cooperation/rate | α0.1 | Difference >1 line |
| 23–30 | 33 | 14 (42%) | 0.5 | 4 (29%) |
| 31–36 | 8 | 8 (100%) | 0.63 | 1 (13%) |
| 37–48 | 10 | 8 (80%) | 0.8 | 0 (0%) |
| 49–60 | 18 | 18 (100%) | 0.8 | 1 (6%) |
| 60–70 | 21 | 21 (100%) | 0.8 | 0 (0%) |
| 23–70 | 90 | 69 (77%) | 0.63 | 6 (9%) |
Figure 3.
Box plots of Lea single symbol acuity (“better” eye of each child) of 69 children examined monocularly on both eyes in the hospital.
Figure 4.
Lea single symbol acuity (LS) measured in the paediatric practice plotted against the LS measured in the hospital. The mean difference LSpractice – LShospital was 1.3 lines. A difference of more than one line occurred in nine children (21%).
Lea symbols showed a higher applicability compared to the Landolt C, especially in young children. Table 3 shows the mean of LS, CLS, LC, and LC2.6 of the “better” eyes, the cooperation rates for monocular testing of both eyes and the number of children older than 30 months without cooperation. Concerning single Lea symbols, six children had an interocular difference of more than one line, mostly two lines. Using the crowded version of the test, five children had an interocular difference of more than one line with a maximum of three lines. In order to detect possible signs of fatigue, Table 4 contains a comparison of the acuities of the (examined first) right eye and the (examined second) left eye of the cooperative children. Evidence of fatigue could not be found because there was no systematic difference between the right and the left eyes.
Table 3.
Mean Lea symbol acuity (LS), crowded Lea symbol acuity (CLS), Landolt C acuity (LC), and crowded Landolt C acuity (LC2.6 ) of the “better” eyes (90 children re-examined in the hospital), cooperation (both eyes monocularly), children older than 30 months without cooperation, and interocular acuity differences >1 line
| Test | Mean | Cooperation/rate | Age >30 months non-cooperative | Difference >1 line |
| LS | 0.94 | 69 (77%) | 2 | 6 (9%) |
| CLS | 0.82 | 51 (57%) | 5 | 5 (10%) |
| LC | 0.82 | 43 (48%) | 13 | 8 (19%) |
| LC2.6 | 0.63 | 40 (44%) | 17 | 6 (15%) |
Table 4.
Comparison of means and medians of acuities of the right eye (RE) which was firstly examined and the left eye (LE) which was examined second (compare with Table 3)
| Test | Cooperation (n) | Mean/median RE | Mean/median LE |
| LS | 69 | 0.88/1.0 | 0.89/1.0 |
| CLS | 51 | 0.74/0.8 | 0.76/0.8 |
| LC | 43 | 0.77/0.8 | 0.75/0.8 |
| LC2.6 | 40 | 0.61/0.63 | 0.56/0.63 |
DISCUSSION
For children older than 30 months, applicability of the Lea symbols was high. The cooperation rate was higher compared with the Landolt C, particularly concerning the single symbol version (77% v 48%). In comparison, in a recent study Lea symbols were found to be superior to the optotypes of the HOTV test in 3 year old children with cooperation rates of 92% v 85%.12 Nevertheless, in the paediatric practice the cooperation rate did not exceed 90% before the age of 4 years. While the overall cooperation rate for visual acuity determination in the paediatric practice was only 50% in those children who later were re-examined, it was 77% in our department. The Lang stereotest also showed better cooperation in the hospital compared to the paediatric practice (97% v 82.5%). This difference may partially be explained by the time interval between both examinations, which was up to 3 months. There may have been a training effect from the previous examination in the practice. Under the study conditions in the hospital, there was more time available to motivate the children. Besides, cooperation in the paediatric practice may have been influenced by negative associations because of vaccinations, for example, during previous visits.
The difference between the acuity values in the paediatric practice and in the hospital may be explained by various factors. Non-compliance of the practice staff with the 3/4 test criterion (“short cuts” or “second chances”) or by shortening the test distance in some cases cannot be excluded. The re-examination in the hospital exactly complied with the prescribed test procedure. Because of the longer lasting examinations in the hospital, there could possibly be fatigue effects in some children. There was no systematic difference between the right eyes, which were always examined first and the left eyes. Nevertheless, a fatigue effect cannot be excluded absolutely. It is difficult to establish generally applicable age related absolute values of visual acuity for children below 4 years.
Measured acuity largely depends on the examined group, the situation, and the motivation of both the child and the observer. This is also confirmed by the Lang stereotest cooperation rates. Using crowded Lea symbols, which make a bigger demand on the child, cooperation decreased from 77% to 57% in the entire re-examination group. Of the children older than 36 months, 96% were testable. In this age group, crowded symbols should be preferred because of higher sensitivity for amblyopia.15 Another previous study comparing ETDRS and Lea symbol acuity also showed crowded Lea symbols to be already applicable in young children.21 For comparison, only 48% (44%) of the children could be examined with the single (crowded) Landolt C. Particularly in younger children, Lea symbols showed a higher applicability. In total, Lea symbol acuity surpassed Landolt acuity by 1.2 (1.9) lines for single (crowded) optotypes concerning those children cooperating in both tests. This difference has to be considered when changing from Lea symbols to the Landolt C. The difference decreases with increasing age because of cooperation and visual development, as well as intellectual development. In adult volunteers, LS surpassed LC by only 0.5 lines.15
In conclusion, the results of this study show that Lea symbols are preferably useful for visual acuity assessment in childhood, as long as the Landolt C is not yet applicable. Important indications for using the Lea test are visual acuity assessment during pleoptic treatment and developmental diagnostics. Age related normal values of Lea symbol acuity up to 5 years, for example by the 10% quantiles of Table 2, can be helpful to inform parents about the acuity development of their child. An interocular acuity difference more than one line, despite good cooperation, should arouse attention irrespective of age.
REFERENCES
- 1.Riggs LA. Visual acuity. In: Graham CH ed. Vision and visual perception. New York: Wiley, 1966:321–49.
- 2.Sheridan MD. Vision screening procedures for very young or handicapped children. In: Gardiner P, MacKeith R, Smith V, eds. Aspects of developmental and pediatric ophthalmology, Clinics in developmental medicine. London: Spastic International Medical Publications, 1969:39–47.
- 3.Atkinson J, Braddick O. `Preferential looking' for monocular and binocular acuity testing of infants. Br J Ophthalmol 1982;66:264–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dobson V, McDonald MA, Kohl P, et al. Visual acuity screening of infants with the acuity card procedure. J Am Optom Assoc 1962;57:284–9. [PubMed] [Google Scholar]
- 5.McDonald MA, Dobson V, Sebris SL, et al. The acuity card procedure: a rapid test of infant acuity. Invest Ophthalmol Vis Sci 1985;26:1158–62. [PubMed] [Google Scholar]
- 6.Teller DY. The forced-choice preferential looking procedure: a psycho-physical technique for use with human infants. Infant Behav Dev 1979;2:135–53. [Google Scholar]
- 7.Katz B, Sireteanu R. The Teller acuity card test: a useful method for the clinical routine? Clin Vis Sci 1990;5:307–23. [Google Scholar]
- 8.Gräf M, Becker R, Neff A, et al. Examinations with the Cardiff Acuity Test. Ophthalmologe 1996;93:333–40. [PubMed] [Google Scholar]
- 9.Hedin A, Nyman KG, Derouet B. A modified letter matching chart for testing young children's visual acuity. J Pediatr Ophthalmol Strabismus 1997;17:114–18. [DOI] [PubMed] [Google Scholar]
- 10.Hyvärinen L, Näsänen R, Laurinen P. New visual acuity test for preschool children. Acta Ophthalmol (Kbh) 1980;58:507–11. [DOI] [PubMed] [Google Scholar]
- 11.Miller JM, Dobson V, Harrey EM, et al. Comparison of preschool vision screening methods in a population with a high prevalence of astigmatism. Invest Ophthalmol Vis Sci 2001;42:917–24. [PubMed] [Google Scholar]
- 12.Hered RW, Murphy S, Clancy M. Comparison of the HOTV and Lea symbols for preschool vision screening. J Pediatr Ophthalmol Strabismus 1997;34:24–8. [DOI] [PubMed] [Google Scholar]
- 13.Bach M, Kommerell G. Determining visual acuity using European normal values: scientific principles and possibilities for automatic measurement. Klin Monatsbl Augenheilkd 1998;212:190–5. [DOI] [PubMed] [Google Scholar]
- 14.Rassow B, Wang Y. Correlation of letter optotypes with Landolt ring for different degrees of visual acuity. Klin Monatsbl Augenheilkd 1999;215:119–26. [DOI] [PubMed] [Google Scholar]
- 15.Gräf M, Becker R, Kaufmann H. Lea symbols: visual acuity assessment and detection of amblyopia. Graefes Arch Clin Exp Ophthalmol 2000;238:53–8. [DOI] [PubMed] [Google Scholar]
- 16.Becker R, Gräf M, Kaufmann H. Assessment of visual acuity of strabismic amblyopic patients with different test charts. Graefes Arch Clin Exp Ophthalmol 1999;DOI 10.1007/s0041799c0647.
- 17.Gräf M, Becker R. Determining visual acuity with LH symbols and Landolt rings. Klin Monatsbl Augenheilkd 1999;215:86–90. [DOI] [PubMed] [Google Scholar]
- 18.Lang J. Ein neuer Stereotest. Klin Monatsbl Augenheilkd 1983;182:373. [Google Scholar]
- 19.Brückner R. Exakte Strabismusdiagnostik bei 1/2- bis 3-jährigen Kindern mit einem einfachen Verfahren, dem “Durchleuchtungstest”. Ophthalmologica 1962;144:184–98. [Google Scholar]
- 20.Haase W, Hohmann A. A new test (C-Test) for quantitative examination of crowding with test results in amblyopic and ametropic patients. Klin Monatsbl Augenheilkd 1982;180:210–15. [DOI] [PubMed] [Google Scholar]
- 21.Harvey EM, Miller JM, Dobson V, et al. A comparison of ETDRS (letter) acuity and Lea (symbol) acuity in a first grade population with a high prevalence of astigmatism. Invest Ophthalmol Vis Sci 1998;39 (Suppl): 947. [Google Scholar]