Abstract
Aim: To investigate the experiences of people with macular disease within the British healthcare system.
Method: The Macular Disease Society Questionnaire, a self completion questionnaire designed to survey the experiences of people with macular disease, was sent to 2000 randomly selected members of the Macular Disease Society. The questionnaire incorporated items about people's experiences with health professionals and the information and support provided by them at the time of diagnosis and thereafter.
Results: Over 50% thought their consultant eye specialist was not interested in them as a person and 40% were dissatisfied with their diagnostic consultation. 185 people thought their general practitioner (GP) was well informed about macular disease but twice as many people thought their GP was not well informed. About an equal number of people thought their GP was supportive as those who thought their GP was not supportive. A total of 1247 people were told “nothing can be done to help with your macular disease.” A number of negative emotional reactions were experienced by those people as a result, with 61% of them reporting feeling anxious or depressed. Of 282 people experiencing visual hallucinations after diagnosis with macular disease, only 20.9% were offered explanations for them.
Conclusions: Many people with macular disease have unsatisfactory experiences of the healthcare system. Many of the reasons for dissatisfaction could be resolved by healthcare professionals if they were better informed about macular disease and had a better understanding of and empathy with patients' experiences.
Keywords: macular disease, doctor-patient communication, quality of life
Despite the prevalence of macular disease1 and its growing incidence,2 little research has focused on the psychological aspects of the condition. Those studies that have been carried out focused on the impact of the condition itself on quality of life and emotional wellbeing.3,4 There are, however, more specific aspects of being diagnosed with a chronic condition such as macular disease that warrant investigation. One such is patients' satisfaction with health care.
The importance of satisfactory doctor-patient communication is well established in psychological research. Good patient centred communication is associated with adherence to treatment regimens, improved biomedical outcomes, reduced length of stay in hospital following treatment, and improved pain control and psychological functioning.5 Studies of cancer patients emphasise the importance of giving the patient both adequate and accurate information.6 Anxiety and depression have been shown to affect recall and comprehension of information in non-patients.7 Other work, however, suggested that anxious patients have better recall of information because they attend more actively.8 These findings indicate that there is no justification for the assumption that withholding information from patients will prevent increased anxiety.
Affective behaviour has been found to be the strongest factor in explaining patient satisfaction.9 Ben-Sira10 found that the affective quality of a consultation is particularly important when patients are anxious about their health, as they will be more sensitive to their doctors' attitudes. Patients who present with deteriorating vision are likely to be worried about their condition and they may be acutely sensitive to the consultant's approach. One aim of the present study was to gain a better understanding of people's experiences with health professionals.
In response to reports of unsatisfactory experiences with health professionals among members of the Macular Disease Society (a British charitable organisation), members of a local group of the society instigated the design and piloting of a questionnaire with which to survey the views and experiences of members of the society. The Macular Disease Society Questionnaire (MDSQ) contained some questions that were derived from the literature, but others were newly designed. Newly designed items included those that concerned people's experiences of health professionals (ophthalmologists, general medical practitioners, and optometrists) at the time of diagnosis and thereafter. They inquired about provision of information, the affective quality of consultations, and the perceived level of support given to patients.
METHOD
Participants
Two thousand people were selected at random from the Macular Disease Society membership of approximately 7500 (in 1999, when the survey was conducted). Inclusion criteria specified that participants were aged 18 years or over, diagnosed with macular disease for at least 6 months, and resident in the United Kingdom.
Completed questionnaires were returned by 1421 members (71%). One respondent was under 18 years old and their questionnaire was not included in the analysis. A further 118 questionnaires were returned uncompleted, giving a gross response rate of 77%. Of these, 11 were returned unopened and 16 were returned because the member had died. A further 14 were unknowingly sent to professional members and supporters who did not have macular disease. Twenty were not completed because the recipients thought the questionnaire did not refer to their own condition (that is, they thought it applied only to people with age related macular degeneration). Thirty four said they were unable to complete it because of visual impairment or other reasons of poor health. Ten people said they were unwilling to complete the questionnaire and 13 gave no reason for non-completion. Participants included 436 men and 975 women (sex unspecified for nine), reflecting the prevalence of macular disease in the general population.2 The mean age of the group was 76 years (SD 10.5). Mean duration of macular disease was 7.34 (6.98) years from the date of diagnosis. Data concerning occupation before macular disease indicated that there were 95 (6.7%) participants in employment category I (professional), 343 (24.1%) in category 2 (managerial and technical), 233 (16.4%) in category 3nm (skilled non-manual), 69 (4.9%) in category 3m (skilled manual), 35 (2.5%) in category 4 (semiskilled), and 22 (1.5%) in category 5 (unskilled).11 Housewives totalled 264 (18.6%) and 340 (23.9%) people indicated only that they were retired. There were no employment data in 19 cases.
The majority of members of the Macular Disease Society were over 50 years of age at onset of macular disease, but membership includes some people with other conditions. The present sample included 23 with macular dystrophy, 15 with macular hole, eight with pseudoxanthoma elasticum, and three with diabetic macular retinopathy.
Materials
The MDSQ was designed for self administration by people with macular disease. The type face Arial 16 bold font was used. All items and instructions were justified to the left. Instructions were enclosed in hatched line boxes. Upper case (with the exception of initial capitals) was avoided where possible. An information letter was included which explained the rationale for the study, guaranteed confidentiality for participants, and asked people to complete the form either by themselves or with the help of another person. The researchers offered telephone help if needed.
Written informed consent was obtained from each participant, in accordance with the Declaration of Helsinki.
Procedure
The Macular Disease Society provided address labels for those members who were selected to receive a questionnaire. These were used to mail the questionnaires and the researchers were given no other information about recipients because of ethical considerations. No copies of the address labels were retained. Thus, no information about non-responders, including postcodes, was available to the study.
Initially, 50 people were mailed to pilot the questionnaire. After studying the responses of the pilot group a blank sheet of paper was added to the end of the remaining questionnaires to allow for extensive open text responses, and instructions to continue on the sheet if necessary were added. The remaining 1950 questionnaires were dispatched over a 4 week period. Four participants requested telephone assistance and these were all dealt with by the first author.
RESULTS
Experiences at the diagnostic consultation
Two questions asked specifically about the diagnostic consultation. Table 1 shows the questions and frequencies of responses. A majority of participants thought their eye specialist was not interested in them as a person and over 40% were dissatisfied with their consultation. Cross tabulation using Cramer's V test of significance showed that there were no differences between expected and observed frequencies across the employment categories of those who considered that their ophthalmologist was interested in them and those who thought he/she was not interested in them. Similarly, there were no differences in the distributions of employment categories of those who were satisfied and those who were dissatisfied with their diagnostic consultation (p values >0.05).
Table 1.
Frequencies (%) and valid percentages of responses to two questions about experiences at the diagnostic consultation.
| Question | Response | No (%) | Valid percentage |
| Did you feel that the eye specialist who diagnosed your macular disease was interested in you as a person? | Yes | 634 (44.6) | 46.3 |
| No | 735 (51.8) | 53.7 | |
| missing | 51 (3.6) | ||
| Did you feel that the interview with the eye specialist was satisfactory? | Yes | 801 (56.4) | 59 |
| No | 557 (39.2) | 41 | |
| missing | 62 (4.4) |
Participants were asked to give their reasons for dissatisfaction. Answers were coded into 10 categories. Table 2 shows the number who gave each reason and the percentage (as a percentage of those who answered the question). Many people gave more than one reason. The two most common reasons given were the attitude of the specialist and lack of information about macular disease.
Table 2.
Reasons for dissatisfaction with diagnostic consultation: numbers, percentages, and details of categories
| Reason for dissatisfaction | No | % |
| Specialist's attitude (dismissive, patronising, brusque, unfeeling, uninterested in patient/condition, use of jargon, talking to colleagues while ignoring patient, making patients feel of no consequence because of their age) | 263 | 43.5 |
| Lack of information or advice (about condition, prognosis, adjustment, low vision aids, self help groups, counselling), lack of written information | 262 | 43.4 |
| Told nothing could be done | 80 | 13.1 |
| Problems with management (delay in getting appointments, paperwork/ correspondence lost, seeing different doctors). | 71 | 11.7 |
| Shocked by what they were told | 47 | 7.05 |
| Lack of time with consultant | 41 | 6.85 |
| Discharged after consultation | 34 | 5.6 |
| Condition not named | 32 | 5.4 |
| No opportunity for questions | 21 | 3.5 |
| Wanted second opinion | 11 | 1.8 |
Experiences with general practitioners (GPs) around the time of diagnosis
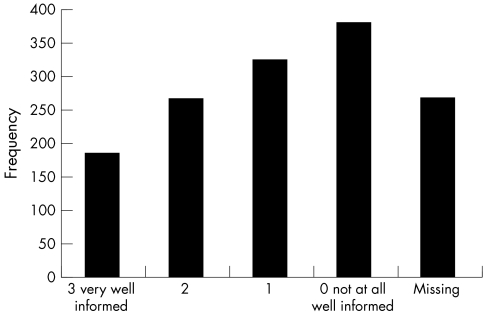
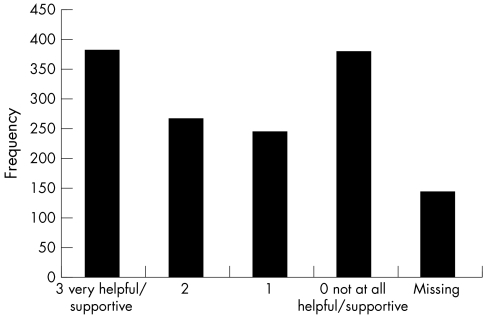
Two questions were asked about participants' experiences with GPs around the time of diagnosis. Figures 1 and 2 show the questions and the frequency of responses, which were made on a Likert scale from 0 to 3. One hundred and eighty five people reported that their GP was very well informed about macular disease but more than twice as many (379) reported that their GP was not at all well informed. About equal numbers reported that their GP was either very supportive (383) or not at all supportive (379). There was a significant correlation between perceived GP knowledge and perceived GP supportiveness (r = 0.561, n = 1126, p = <0.01). A high proportion of non-responders to these two questions prompted investigations to highlight any differences between responders and non-responders. Cross tabulations using Cramer's V test of significance showed that participants who were less severely affected with macular disease were over-represented in the non-responders groups for both questions (V = 0.085, p <0.018; V = 0.103, p <0.005). Severity was determined by self reported registration as blind, partially sighted, or non-registration. There were no differences between expected and observed frequencies across different types of macular disease (categories wet, dry, not age related macular degeneration, and don't know) (p >0.05). For both questions t tests for independent samples showed that non-responders were significantly older than responders (GP knowledge; t = 3.607, n = 1414, p <0.001: GP supportiveness; t = 2.264, n = 1414, p <0.05).
Figure 1.
Frequencies of responses to the question “Around the time you were first diagnosed with macular disease, to what extent was your general practitioner well informed about macular disease?”
Figure 2.
Frequencies of responses to the question “To what extent has your GP been helpful and supportive?”
Emotional and other reactions to being told “Nothing can be done about your macular disease”
Participants were asked `Were you ever told that nothing could be done to help with your macular disease?' A total of 1247 responded “yes” and 135 replied “no.” Participants were asked to indicate whether or not they had experienced each of a number of reactions to being told “nothing can be done” (Table 3). Most commonly reported were the reactions of anxiety and/or depression (n = 757, 60.7%) and resignation (752, 60.3%). As many as 54 (4.3%) reported feeling suicidal. Many reported experiencing more than one of the reactions listed. Some participants appeared to have completed only the items to which they gave positive responses, resulting in missing data for each question, ranging from 128 (10.3%) to 217 (17.4%) cases. Participants were asked to state any other emotional reactions in an open text box. Fourteen said they accepted the condition as part of the ageing process, and 12 said they felt determined to find out as much as possible or to explore every avenue.
Table 3.
Numbers of participants experiencing and not experiencing emotional reactions to being told that “Nothing can be done to help your macular disease” and percentage (as a % of those who were told “Nothing can be done”)
| No | ||
| Reaction | Yes (%) | No (%) |
| Anxiety/depression | 757 (60.7) | 362 (29.0) |
| Resigned | 752 (60.3) | 394 (31.6) |
| Shocked/sick/panic | 652 (52.3) | 446 (35.8) |
| Helpless | 629 (50.4) | 457 (32.2) |
| Angry | 395 (31.6) | 664 (46.8) |
| Suicidal | 54 (4.3) | 976 (68.7) |
Visual changes associated with macular disease
A series of questions investigated the experience of photopsias and visual hallucinations, which is common in macular disease and some other eye conditions.12 A total of 1111 people (78.2%) said they had experienced visual changes following the onset of macular disease. Only 257 (18.1%) said they had not experienced them. The three most commonly reported were blurred vision, light flashes, and difficulty seeing at night (Table 4). Hallucinations were reported by 282 people (19.9%). The data show that 518 participants (46.6% of those experiencing visual changes) who experienced visual changes had talked to a health professional about them and, of those, 206 (39.8%) had been given an explanation for them. Among those reporting hallucinations, 122 (43.3%) had mentioned them to a health professional. Of those, only 59 (48.36%) had been given an explanation. Thus, of all those experiencing hallucinations, only 20.9% were given an explanation for them by a health professional. Explanations were not always accurate or reassuring. Among such explanations were age (n = 3), stress (n = 2), psychological (n = 1), brain confusion (n = 1), nothing to do with macular disease (n = 1), and environment (n = 1).
Table 4.
Frequencies of visual changes reported following onset of macular disease and percentages (as a % of those who experienced visual changes)
| Visual change | No | (%) |
| Blurred vision | 512 | 46.1 |
| Flashes of light | 461 | 41.5 |
| Difficulty seeing at night | 418 | 37.6 |
| Difficulty seeing depth | 311 | 28 |
| Hallucinations | 282 | 25.4 |
| Changing coloured patterns | 250 | 22.5 |
| Shimmering light | 245 | 22 |
| Pulsating lights | 236 | 21.2 |
| Other visual changes | 235 | 21.1 |
DISCUSSION
The MDSQ surveyed the experiences of people with macular disease over a wide range of issues. More than half the participants in the survey considered that their eye specialist was not interested in them as a person, and just under half were dissatisfied with their diagnostic consultations. The level of dissatisfaction may reflect inadequacy felt by health professionals because of their inability to treat macular disease. Participants offered a variety of reasons for dissatisfaction with the diagnostic consultation in response to an open ended question. The attitude of the specialist was the most commonly cited reason and this embraced several different types of behaviour which patients found unsatisfactory. Diagnosis of a disease such as macular disease, which carries with it the prospect of a diminished quality of life and possible erosion of independence, is likely to have a considerable, negative impact. When this bad news is delivered in an unsympathetic way by an unsupportive consultant, the patient is likely to feel all the more shocked. The second most common reason for dissatisfaction was lack of information. Fallowfield13 asserted that it is fundamentally important for patients to be given adequate information and that the information is believed, understood, and remembered. In a study of patients with early breast cancer, those who received inadequate information about their condition experienced more anxiety and depression than those who were satisfied with the level of information given.14 The evidence from the present study also underlines the likelihood that benefits would accrue from providing patients with clear information at the diagnostic consultation, given in such a way as to help their understanding and recall. In addition, the provision of appropriately written information would allow people to revisit the information and learn about their condition at their own pace.
One piece of information that most participants were given was that “Nothing can be done to help with your macular disease.” Whereas often nothing can be done medically, resources are available to help with adjustment to macular disease, including rehabilitation services and low vision aid provision and training. Fifty four responders to the survey reported feeling suicidal when told “Nothing can be done.” Dodds et al15 noted the possibility of suicidal tendencies in those with newly diagnosed visual impairment. A constructive approach to macular disease by consultants would avoid fuelling negative emotions. Seven hundred and fifty two participants (60%) reported feeling resigned when they were told that nothing could be done for their macular disease. Resignation can be seen as a qualitatively different reaction from the negative emotional reactions that form the remainder of the list. Being resigned may be a form of acceptance of the situation, and it may be the first step in adjusting to the condition. Participants were invited to mention any other reactions to being told that nothing could be done and 12 wrote that they were determined to find out more about macular disease or determined to explore all avenues. A few said they were relieved that only one eye was affected or that it was not something more serious. Such reactions are likely to be associated with better adjustment. Others (n=14) said that they accepted it because of their age. When no medical treatment is available for macular disease, there is a need for health professionals to emphasise the benefits to the quality of life of patients that can be gained by use of the available rehabilitation and low vision services. Patients can benefit substantially if health professionals are aware of the importance of information and support when no medical treatment can be prescribed.
Many people in the survey indicated that their GPs were not at all well informed about macular disease and many participants reported that they were unsupportive. The high number of participants who did not respond to the questions about GPs was interesting. A number wrote on the questionnaires that they had had no contact with their GPs about their eye condition, and it is possible that others did not respond for the same reason. GPs are generally more accessible than ophthalmologists and could be a valuable source of information and support as well as being the means of directing people to rehabilitation and low vision services. The lack of contact with GPs is, therefore, a cause for concern. However, even those who had consulted their GPs about macular disease often found that their GPs were poorly informed about the condition, and there was a positive correlation between perceived knowledge and perceived helpfulness/supportiveness of GPs. The data indicate the need for GPs to learn about macular disease and for an appraisal of the potential role for GPs in the management of macular disease. Starr et al16 stressed the importance of the role of primary care physicians in detecting macular disease and in helping patients to learn about their condition. Non-responders were significantly older than responders for both questions, possibly because older people are reluctant to trouble their doctors. Cross tabulation calculations showed that people who were not registered as partially sighted or blind, and who therefore probably had milder macular disease, were over-represented among the non-responders. If GPs had some contact with all patients with macular disease, patients would be more likely to feel they have a route to further care if needed and GPs could monitor the progression of the condition. Such contact is particularly important for older people as they may be unaware of a gradual deterioration.17 The lower number of missing responses to the question “To what extent has your GP been helpful and supportive” may be because the question did not specifically refer to macular disease. Some participants may have responded in terms of their GPs' overall supportiveness.
A large majority of the sample (1111) reported that they had experienced visual changes such as flashing lights, blurred vision, and hallucinations. Since these phenomena are common in macular disease,12 it would be helpful to inform people when they are first diagnosed of the possibility of having these experiences. It may be that people are reluctant to report symptoms that are commonly associated with more sinister conditions, such as dementia, for fear of a disturbing explanation. This may be the case if patients feel that their doctor is uninterested in them. Even when the subject of hallucinations was broached by participants, fewer than half were given an explanation. Some of the explanations were not reassuring and may even have served to exacerbate fears that their hallucinations were a symptom of dementia. This evidence points to the need for better information for doctors so that they are in a position to reassure their patients that such symptoms are likely to be short lived, benign, and are frequently experienced by people with macular disease. It also illustrates the need for doctors to be more forthcoming with information and ready to discuss any anxieties patients may have.
Where patients have treatable conditions, successful outcomes may help ameliorate the negative emotions that are evoked by unsatisfactory consultations and contacts with health professionals. If patients are told that no treatment is available for their failing sight during consultations that they find distressing in other ways, or if they are discharged from the clinic, they will be given an unnecessarily poor start to an adaptation process that will, anyway, not be easy. Research has suggested that with advances in technology in medicine have come unfortunate consequences for the patient. Fitzpatrick18 commented that:
“Workers in the healthcare system, particularly doctors, are less sensitive to the concerns of their patients and to the personal significance for the patient of the disorders that they present.”
Health professionals with a concerned, empathic approach are more likely to help patients over the shock of diagnosis. Other research has shown that improved outcomes, including psychological wellbeing, accrue from patient satisfaction with health care.5 A prospective, longitudinal study of patients with newly diagnosed macular disease is planned to examine such relations.
The authors recognise that the participants in this study may not be a representative sample of people with macular disease in the general population, as they were drawn from the membership of the Macular Disease Society. As a result of their membership and the information provided by the society, they are likely to be well informed people who have taken a positive step to help themselves by making contacts and by finding ways of adjusting to life with macular disease. Others may be less knowledgeable about macular disease and about available facilities. Also, the participants include only four people who were unable to complete the questionnaire themselves or to find anyone who they were willing to ask for help. People with a combination of very poor eyesight and lack of social support may be under-represented in the sample. It is unlikely, however, that participants' experiences in the healthcare setting were substantially different from people who are not members of the Macular Disease Society. Although the higher employment categories are over-represented in this sample of the MDS membership compared with the population at large, non-significant cross tabulation tests indicate that perceptions of the quality of consultations and care did not differ across social categories.
In summary, the evidence from this study indicates that many people with macular disease have unsatisfactory experiences with health professionals around the time of diagnosis and subsequently. The data point to shortcomings in the provision of information and in the affective quality of interactions with ophthalmologists and other health professionals. In many cases, these shortcomings could be resolved with more sensitive awareness of patients' anxieties and of their need for information in the consultation. When no medical treatment is available, it becomes all the more important to give as much other help and support as possible together with information about low vision aids and local support services. Such support would offer people with macular disease the best chance of adjusting successfully to living with macular disease, retaining their independence, and protecting their quality of life.
Acknowledgments
Funding was provided by the Macular Disease Society and Alcon Laboratories. Our thanks also go to the Macular Disease Society Council for its support and to the members for their participation.
REFERENCES
- 1.Klein R, Klein BEK, Linton KLP. Prevalence of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology 1992;99:933–43. [DOI] [PubMed] [Google Scholar]
- 2.Evans J, Wormald R. Is the incidence of age-related macular degeneration increasing? Br J Ophthalmol 1996;80:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davis C, Lovie-Kitchen J, Thompson B. Psychosocial adjustment to age-related macular degeneration. J Vis Impair Blind 1995;Jan-Feb:16–26.
- 4.Williams RA, Brody BL, Thomas RG, et al. The psychosocial impact of macular degeneration. Arch Ophthalmol 1998;116:514–20. [DOI] [PubMed] [Google Scholar]
- 5.Stewart MA. Effective physician-patient communication and health outcomes:a review. Can Med Assoc J 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 6.Fallowfield L. Truth sometimes hurts but deceit hurts more. Ann N Y Acad Sci 1997;809:525–36. [DOI] [PubMed] [Google Scholar]
- 7.Pickersgill MJ, Owen A. Mood states, recall and subjective comprehensibility in non-patient volunteers. Personality Individual Differences 1992;13:1299–305. [Google Scholar]
- 8.Ley P. Recall by patients. In: Baum A, Newman S, Weinman J, West R, McManus C, eds. Cambridge handbook of psychology, health and medicine. Cambridge: Cambridge University Press, 1997:315–17.
- 9.Bensing J, Schreurs K, De Rijk A. The role of the general practitioner's affective behaviour in medical encounters. Psychol Health 1996;11:825–38. [Google Scholar]
- 10.Ben-Sira Z. Affective and instrumental components in the physician-patient relationship: an additional dimension of interaction theory. J Health Soc Behav 1980;21:170–80. [PubMed] [Google Scholar]
- 11.Office of Population Censuses and Surveys. Standard occupational classification. 2nd ed. London: HMSO, 1995.
- 12.Brown GC, Murphy RP. Visual symptoms associated with choroidal neovascularisation. Arch Ophthalmol 1992;110:1251–6. [DOI] [PubMed] [Google Scholar]
- 13.Fallowfield L, Jenkins V. Effective communications skills are the key to good cancer care. Eur J Cancer 1999;35:1592–7. [DOI] [PubMed] [Google Scholar]
- 14.Fallowfield LJ, Hall A, Maguire GP, et al. Psychological outcomes of different treatment policies in women with early breast cancer outside a clinical trial. BMJ 1990;301:578–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dodds AG, Bailey P, Pearson A, et al. Psychological factors in acquired visual impairment: the development of a scale of adjustment. J Vis Imp Blind 1991;85:306–10. [Google Scholar]
- 16.Starr CE, Guyer DR, Yannuzzi LA. Age-related macular degeneration: can we stem this worldwide public health crisis? Postgrad Med 1998;103:153–64. [DOI] [PubMed] [Google Scholar]
- 17.Cullinan, T. Visual disability in the elderly. Beckenham: Croom Helm, 1986.
- 18.Fitzpatrick R. Satisfaction with health care. In: R Fitzpatrick, J Hinton, S Newman, G Scambler, J Thompson, eds. The experience of illness. London: Tavistock Publications, 1984.