Abstract
Aims: In many countries the number of corneal donations is far too low to graft all patients on waiting lists within reasonable time. The aim of this study was to define specifically what practical changes are to be implemented to fully meet corneal graft demand.
Methods: The list of potential donors drawn by the coordination team from 1 January to 31 December 1999 was compared with that of all patients who had died during the same period. In each identified record, the parameters which permitted or precluded effective collection of cornea specimens were analysed, and the reasons why other records were not identified were investigated.
Results: Among the 1112 patients who died in 1999, coordinating nurses were able to identify 451 records (40.5 %) including 329 patients aged between 18 and 85 years (29.5%). After excluding 184 patients (55.9 %) who presented with medical contraindications, the coordinating nurses were able to meet the relatives of only 55 out of 145 patients (38%) and obtained their agreement in 39 cases (71% approval rate). Therefore, relatives' refusal was the cause for the absence of collection in only 5.5% of cases (16/290). The number of cornea procurements amounted to 11.8% of identified records and 3.5% of all deceased patients.
Conclusion: French law and regulations regarding tissue collection are based on consent presumption but it requires that verifications be made with the relatives to ensure that potential donors were not, before their death, opposed to such tissue procurement. That provision implies a high degree of organisation on the part of coordinating teams. It was demonstrated that donation shortage is no longer the result of relatives' refusal but rather because of logistical difficulties (potential donors not identified and problems in reaching relatives). It appears necessary therefore to strengthen coordinating teams with sufficient staff levels for wider donor identification. Those teams should also find ways to keep closer contact with relatives, so as to meet the maximum transparency targets required by public opinion and regulations and to graft all patients awaiting corneal transplantation.
Keywords: cornea, corneal transplantation, legislation, jurisprudence, organ procurement, tissue donors
If significant advances have been made in corneal graft (graft safety in cornea banks, better medical follow up, resumption of lamellar keratoplasty, or limbic graft development, etc), the number of retrieved corneas still falls far short of those required to satisfy within reasonable time all patients on waiting lists in a number of European countries.1–3 For instance, France's estimated needs in 1998 totalled 7400 grafts but only 4549 were carried out, including 25% from specimens imported from abroad.4 The causes for that shortage have yet to be clearly defined, as recently underlined by Armitage in an alarming letter.2 If the obligation to obtain relatives' approval is a major hurdle to cornea donations,5 in fact, it appears that graft shortage is mainly due to organisational problems in collection centres, the number of donors being largely higher than that of effective procurements.1,6,7
To better understand that crisis situation, but also to warrant the highest possible safety level and observance of ethical rules, the French government in 1994 instated the French Graft Agency, an organisation in charge of tissue specimen collection and grafts.4 In 1997, following the official publication of the Good Practices for Tissue Sampling, the coordinating teams in charge of identifying and managing relatives became more involved in tissue postmortem collection, cornea in particular, although their staffing levels were only slightly improved.
Confronted with chronic shortage of corneal grafts in this region, we decided to conduct a survey to identify all patients who had died in this hospital over 1 year. We determined the percentage of corneal grafts procured in our hospital and related it to the number of potential donors and we identified the true causes of graft shortage. The aim was to precisely define the practical and logistical changes required to fully meet the local demand for corneal grafts
We believe the conclusions of this study may be used in all countries confronted with corneal graft shortage, in particular those whose regulations, as in France, make it mandatory to meet donors' families before any tissue sampling.
PATIENTS AND METHODS
We retrospectively but accurately identified and counted all patients who died in the Charles Nicolle Hospital, Rouen, France, between 1 January and 31 December 1999. That survey was based on the hospital administrative register where daily entries were made with the names, ages, time of death, medical ward/department, and time of entry to the mortuary of each dead patient. We then compared these records with those of the patients effectively identified by our coordinating team during the same period. When patients had not been identified, we investigated the reasons that could explain the non-identification. When patients could be identified by the coordinating nurse, we analysed the various parameters which permitted or ruled out effective graft sampling. Once the causes were determined, we tried to consider correcting them and hence we extrapolated the number of possible samplings in a centre like this one.
Our coordination team is composed of two coordinating nurses: one is employed on a full time basis and the other one is half time. Both simultaneously handle multiorgan collection and postmortem collection of corneal grafts. They are alternately present from 9 am to 5 pm Monday to Friday and ensure a 24 hour on-call watch for multiorgan collections and organ graft only.
Because of that activity, coordinating nurses only deal with postmortem corneal graft collection during daytime hours (9 to 5) Monday to Friday and when they are not engaged in a multiorgan collection/sampling, in coordinating organ transplantation in the hospital (kidney or heart), or by actions to promote organ and tissue donations.
For a few years now, we have been using an active system to detect dead patients, the ward teams having always refused to inform the coordination team of the death of one of their patients. Consequently, the coordinating nurse each morning contacts the hospital mortuary to draw a list of all patients who had died since noon the previous day and who are thus eligible for tissue sampling within 24 hours following their death. The coordinating nurse excludes all patients under age from that preselection because of the foreseeable difficulties when confronted with relatives. She also excludes patients over 85—a rule since 1998—because the lower quality of their corneal endothelium often led the cornea bank manager to discard those grafts, and that created a source of discouragement for the collecting team. The coordinating nurse also excluded, on principle, all patients who had died in the infectious disease departments, in dermatology, and cancer centres because the highly time consuming record analysis almost systematically resulted in a medical contraindication to tissue sampling. This was the occasion to update a register with the names and medical characteristics of identified potential donors.
The coordinating nurse then contacts the medical team that followed up the dead patient to check for a possible contraindication to cornea sampling. The selection criteria are specified in the guidelines of the French Graft Agency in compliance with the rules of the American Eye Bank and European Eye Bank associations.8 We excluded also from our preselection those deceased patients who had a history of neurosurgery and those who died from cancer with metastases.
When procurement could be considered, the coordinating nurse would contact the registry officer of the hospital to be kept informed of the dead patient's relatives' visit to the hospital to carry out hospital formalities. Upon their arrival, the coordinating nurse, signalled through her personal phone, can be with them within 5 minutes and take them to a special office. The meeting with the relatives includes the coordinating nurse and an ophthalmologist. Four points are emphasised to the relatives—the benefit provided to two blind individuals, the absence of any mutilation whatsoever to the patient during sampling, that only cornea will be collected, and procurement will not hamper in any way the formalities necessary for the funeral ceremony and burial.
If the relatives have not shown up within 24 hours of the patient's death, or if they have already carried out and completed administrative formalities and left the hospital before the nurse's first call to the registry officer, or if they came outside of administration working hours, the procurement is declared lost. Indeed, the coordination team have not deemed it reasonable to contact relatives by phone to ask for their agreement, fearing a violent and negative reaction.
Once the relatives' permission is secured, the coordinating nurse must obtain the formal signature of the hospital administrative manager and notify the ophthalmological team. Cornea removal is then performed by a resident ophthalmologist in a surgical room adjacent to the mortuary, usually between midday and the mortuary closing time of 6 pm.
RESULTS
From 1 January to 31 December 1999, 1112 patients died in our hospital in the departments identified by the coordinating nurse.
Of those 1112 deceased patients, 451 (40.5%) were identified as potential donors by the coordinating nurses during their working hours but 661 patients (59.5%) could not be identified (Table 1).
Table 1.
Distribution of the 1112 records of dead patients according to their identification or not by the coordination team
| Number of patients (%) | Number of patients (%) | ||
| Dead patients identified by the coordinating nurse | 451 (40.5%) | Records effectively analysed | 329 (29.5%) |
| Records excluded because of potential donors' age | 122 (11%) | ||
| Dead patients not identified by the coordinating nurse | 661 (59.5%) | Patients deceased during weekends or holidays | 299 (27%) |
| Coordinating nurse unavailable | 301 (27%) | ||
| Forensic contraindication to procurement | 35 (3.2%) | ||
| Taken away by funeral services before identification | 26 (2.3%) | ||
| Total | 1112 (100%) | 1112 (100%) |
Considering that 122 patients were either under age or over 85, coordinating nurses effectively analysed 329 potential donors' records—that is, 29.5% of all deceased patients. Of the 661 deceased patients who were not identified, 299 died during week ends or holidays, more than 24 hours before the coordinating nurse's return, 301 patients who died during the week could not be identified because the coordinating nurse was busy elsewhere, 35 were subject to forensic medicine restrictions, and 25 were taken away by funeral services before coordinating approaches (Table 1).
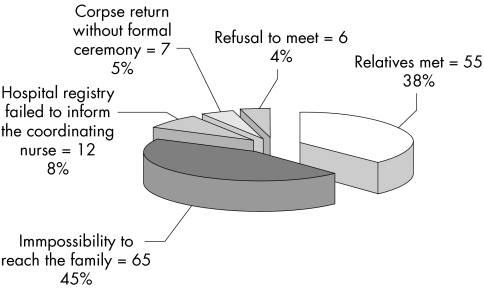
Of the 329 records analysed by the coordinating nurse, 184 patients (55.9 %) had medical contraindications (Table 2) and had to be excluded. The coordinating nurses therefore contacted the hospital registry to meet the relatives of the 145 potential donors with no contraindications to cornea procurement. Figure 1 clearly illustrates the organisational difficulties encountered because it was not possible to meet relatives during their visit to hospital in 45% of cases (n = 65), either because they had already left the premises or did not report to the hospital registry within 24 hours following the death of the patient. Taking account of the “forgetfulness” of some and the wish of some relatives to retrieve their loved one's corpse as soon as possible, coordinating nurses were only able to meet relatives in 55 cases (38%).
Table 2.
Distribution of medical contraindications to cornea collection in 184 of the 329 dead patients identified by the coordination team
| Aetiologies | Number of patients (%) |
| Cancer with metastases | 125 (67.9) |
| History of neurosurgery | 7 (3.8) |
| Alzheimer's disease | 2 (1.1) |
| Known dementia | 9 (4.9) |
| Meningitis | 4 (2.2) |
| Known viral hepatitis | 3 (1.6) |
| Tuberculosis | 2 (1.1) |
| Other causes | 14 (7.6) |
| Cause or death unknown | 18 (9.8) |
| 184 (100) |
Figure 1.
Analysis and distribution of the 145 potential donors identified with no medical contraindications to postmortem cornea collection.
In total, out of the 329 identified potential donors, coordinating nurses met relatives in only 16.7% of cases (n = 55) (Table 3) and obtained their consent in 39 cases (71% consent rate). The number of donors where corneas were effectively removed (n = 39) thus represented only 11.8% of records identified by the coordinating nurse and 3.5% of the overall number of patients who died in the various hospital wards (Fig 2).
Table 3.
Analysis and distribution of the 329 potential donors' records, identified by the coordination team
| Number of patients | % | |
| Medical contraindications to procurement | 184 | 55.9 |
| Impossibility to meet the relatives | 90 | 27.3 |
| Hospital registry failed to inform the coordinating nurse of the relatives' visit | (12) | (3.6) |
| Corpse return without formal ceremony | (7) | (2.1) |
| Refusal to meet | (6) | (1.8) |
| Relatives left the hospital before formalities or did not show up within 24 hours |
(65) | (19.8) |
| Relatives met | 55 | 16.7 |
| Relatives' approval | (39) | (11.8) |
| Relatives' refusal | (16) | (4.9) |
| Total | 329 | 100 |
Figure 2.
Distribution of the 1112 dead patients according to whether their records were analysed or not by the coordination team and to their possible outcome at postmortem cornea collection.
DISCUSSION
French law regarding organ and tissue sampling is based on presumed consent, as in most European countries, as it stipulates that procurements can be performed if the deceased patients did not, before dying, express their refusal. Nevertheless, since a 1992 ministerial circular, confirmed in 1994 by the bioethics laws, the law stipulates that “physicians, if they are not aware of the deceased patient's will, shall seek to obtain the relatives' testimony.” As the word “seek” lacks precision, hospital management staff have demanded that procurement be only performed after relatives have effectively been met by the coordination teams. That additional provision probably contributed to the fall in the number of corneal procurements in France, which dropped from 3774 in 1991 to 2383 in 1993.9 The number of corneal specimens imported into France increased in parallel from 221 in 1991 to 1016 in 1998.4
This study clearly reflects the magnitude of the drop in the number of grafts collected. Among the 145 potential donors identified as free of medical contraindications and not expressing their refusal to donate through hospital or national registries over one year, procurement could effectively be performed in only 39 cases (26.9%).
This figure suggests that the drop in the number of samplings is directly linked to a high refusal rate from relatives and that donation awareness campaigns are necessary to sensitise public opinion. That is not true; among the 329 potential donors identified by our coordination team, relatives' refusals precluded procurement in only 16 cases (5.5%) whereas 59.5% of all patients who died in our hospital escaped identification by our coordination team. When relatives were met by our coordination team, their consent to cornea donation was granted in 71% of cases and hypothesising on increasing that proportion to 100% as a result (unlikely) of a major awareness campaign, only 55 patients instead of 39 would have been effectively sampled in our series (4.9% v 3.5% of patients who died in the hospital). Mack et al6 reported 3.7% corneal samplings, in relation to the number of deaths and Carrey et al10 reported 6% when relatives' approval rate ranged from 39.5%7 to 44%,11 57%,10 or even 81.6%12 and 82%.13
The first cause for excluding identified donors is, in fact, the medical contraindication noted in 55.9% of cases. That figure may look high, but is quite close to the 53% reported by Carrey et al from 1044 patients identified,10 to the 52% reported by Diamond et al11 and slightly higher than Navarro et al's 32%,3 although the latter applied more restrictive age criteria explaining the 45% of non-collection. There is no doubt that the need to collect grafts within the hospital accounts for the high percentage of pathological contraindications to corneal sampling and perhaps graft collection should be extended to other types of institutions. One readily understands that those selection criteria are necessary and cannot be slackened to make up for graft shortage.
So, except for medical contraindications, whose proportion cannot be reduced, it clearly appears from these results that logistical issues are the main cause of the low sampling rate. It is worth remembering that when there was no medical contraindication to procurement in a deceased patient, our coordination teams were able to meet the relatives in only 38% of cases and with the staff currently available they can only identify 40.5% of deceased patients in a year. It can thus be concluded that if coordinating nurses could meet the relatives of all potential donors, the number of cornea grafts collected would be multiplied by a factor of 2.63 and if the staff enabled them to identify all patients deceased in the hospital, the number of cornea samples would again be multiplied by 2.47. In total, the number of grafts would then be multiplied by a factor of 6.5.
One solution to increase the number of families contacted would be to get their approval by telephone, because a large number of relatives have already left the hospital when formalities are being initiated, or did not report within 24 hours following the patient's death. Australian coordination teams frequently resort to that method, it is easier for the patients' intentions regarding organ or tissue donation are clearly mentioned on their driver's licences.14 There is no such provision in France and coordination teams are sometimes reluctant to use that means of communication, for fear of a more violent rebuttal by relatives who may feel dragged into a commercial transaction of sorts. Gain et al,12 however, have very recently reported the use of the telephone as a means to contact donors' relatives and their results clearly demonstrate the interest of that means of communication. Their results show that in the absence of medical contraindications to graft collection, they were able to meet only 31.2% of relatives in face to face interviews (142/455), a proportion close to our own results (38%). But the use of the telephone enabled them to contact the relatives of 192 additional patients (42.2% more). In addition, the 55.2% donation approval rate they describe, albeit below the 81.6% rate obtained in face to face interviews, still appears more than respectable. The end result is that they were able to almost double the number of samplings (222 v 116). We believe therefore that coordination teams could use the telephone more freely and train themselves accordingly because such a method certainly requires even more diplomacy than face to face interviews.
The second point that could also be improved is also logistical: the small number of potential donors identified by our coordination teams (40.5%). That figure directly depends on the qualification and number of the coordination team personnel; in our case, one full time and one half time nurses for organ and tissue collection. Carrey et al10 identified 59% of deceased patients with two full time coordinating nurses dedicated to organ and tissue collection. To Philpott et al,14 the appointment of a specific coordinator available 24 hours for cornea collection permitted total elimination of waiting lists for corneal grafts in South Australia. It thus appears necessary to strengthen coordination teams with sufficient staff to ensure both maximum transparency targets and sustained sampling activity to graft all patients on waiting lists for corneal graft.
We are also aware that our conclusions, as they read, could lead to law amendment proposals aimed at alleviating collection procedures. A number of discussions have been ongoing since 1992 at the ministerial level and since 1994 at the level of the French Graft Agency. They only resulted in the implementation of a “refusal database” where any French citizens can register themselves, but whose sole effect was to make procedures even more cumbersome. Thus, while coordinators now have to consult the national database before initiating cornea procurement formalities, it is still necessary to meet the relatives to ensure that the potential donor was not opposed to procurement. It is worth noting that tissue procurement law varies from one country to another and often reflects the views of the general population. Relation with death also differs between countries and certain solutions that can be applied or adapted to one country will not necessarily apply to another. Thus, in a number of countries, all patients being admitted to hospital are requested to state their organ and tissue donation wishes. That proposal is very appealing in that it would simplify proceedings. It was not implemented in France, probably because of fear of scaring patients who enter hospital. Despite the existence of a law based on acceptance presumption, French law makers have imposed that the absence of donors' opposition to donation be ascertained from relatives. Indeed it would be inconceivable to many that collection be carried out without the relatives' consent. It was for the same reason that the option of writing one's consent or refusal to donate on one's driver's licence was rejected, because it would not have avoided the legal obligation to meet the donor's relatives.
It is also quite surprising that tissue/organ procurement raises some degree of reluctance among surgical or medical teams in a hospital where many organ or tissue grafts are performed as routine. Despite a number of awareness sessions being delivered by coordinators in the different departments of the hospital, coordinating nurses have never been informed of a patient's death by the medical teams. This was probably due in part to a failure of the administrative leadership within the hospital, although we believe there is also a share of affect and guilt on the part of the medical teams after the death of one of their patients. We believe that reluctance to contact the coordinating team after a patient's death is not specific to our hospital and we have elected to call the hospital mortuary directly every morning to be informed of recently dead patients.
Another clear example of the reluctance to procurement is the self imposed limits on asking younger patients for donation. Indeed, parents have often been found to be willing to donate their children's organs or tissue if asked,15,16 and there is no reason for an age limit to be set on procurement. Nevertheless, that would not have significantly increased the number of procurements in our study because most deceased patients under age were either infants under 1 year or children with neoplasias.
In conclusion, this study provides a non-complacent picture of the logistical problems at the origin of corneal graft shortage in France and we believe that situation to be similar in a number of other countries. The obligation to meet relatives amplifies logistical difficulties. The proportion of relatives' refusal to approve donation is proportionally low and rather than funding awareness campaigns to promote donations, it would be more appropriate to strengthen coordination teams with additional staff and, more specifically, for each hospital to appoint a coordinator exclusively dedicated to postmortem corneal collection.
Acknowledgments
The authors thank Mr Rousseau-Cunningham for his advice in editing the English manuscript.
REFERENCES
- 1.Delbosc B. Difficult cornea procurement:causes and consequences of the exceptional situation in France. J Fr Ophtalmol 2000;23:196–9. [PubMed] [Google Scholar]
- 2.Panda A, Kumar S, Thakur SK. Decline in eye donation in the UK. Br J Ophthalmol 2000;84:805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Navarro A, Cabrer C, De Cabo FM, et al. Importance of the transplant coordinator in tissue donor detection. Transplant Proc 1999;31:2606. [DOI] [PubMed] [Google Scholar]
- 4.Tuppin P, Dunbavand A, Cohen S, et al. Trends and estimates of regional differences of cornea donation and transplantation in France (1991–1998). J Fr Ophtalmol 2000;23:465–71. [PubMed] [Google Scholar]
- 5.Lee PP, Yang JC, McDonnell PJ, et al. Worldwide legal requirements for obtaining corneas: 1990. Cornea 1992;11:102–7. [DOI] [PubMed] [Google Scholar]
- 6.Mack RJ, Mason P, Mathers WD. Obstacles to donor eye procurement and their solutions at the University of Iowa. Cornea 1995;14:249–52. [DOI] [PubMed] [Google Scholar]
- 7.Loewenstein A, Rahmiel R, Varssano D, et al. Obtaining consent for eye donation. Isr J Med Sci 1991;27:79–81. [PubMed] [Google Scholar]
- 8.Pels E, Tullo A. Directory of European eye banks. 8th ed. Amsterdam: EEBA, 2000.
- 9.Tuppin P, Loty B. The progress of cornea donation and transplantation in France. Cornea 1999;18:682–5. [DOI] [PubMed] [Google Scholar]
- 10.Carrey I, Hudel Y, Salame N, et al. Procurement of corneas: analysis of inventory of hospital coordination. Prospective study at the Besançon Hospital University during the course of one year. J Fr Ophtalmol 2000;23:996–1000. [PubMed] [Google Scholar]
- 11.Diamond GA, Campion M, Mussoline JF, et al. Obtaining consent for eye donation. Am J Ophthalmol 1987. 15;103:198–203 [DOI] [PubMed] [Google Scholar]
- 12.Gain P, Thuret G, Loup Pugniet J, et al. Obtaining cornea donation consent by telephone. Transplantation 2002;73:926–9. [DOI] [PubMed] [Google Scholar]
- 13.Williams KA, White MA, Badenoch PR, et al. Donor cornea procurement:six-year review of the role of the eye bank in South. Aust N Z J Ophthalmol 1990;18:77–89. [DOI] [PubMed] [Google Scholar]
- 14.Philpott M, Bain M, Coster DJ. Procurement of all the donor corneas needed:how is it achieved? Transplant Proc 2000;32:69–71. [DOI] [PubMed] [Google Scholar]
- 15.Walker JA, McGrath PJ, MacDonald NE, et al. Parental attitudes toward pediatric organ donation:a survey. CMAJ 1990;142:1383–7. [PMC free article] [PubMed] [Google Scholar]
- 16.Weiss AH, Fortinsky RH, Laughlin, JB, et al. Parental consent for pediatric cadaveric organ donation. Transplant Proc 1997;29:1896–90. [DOI] [PubMed] [Google Scholar]