Abstract
Aims: To report remodelling of enlarged dysmorphic filtration blebs with conjunctival compression sutures and autologous blood injection.
Methods: A retrospective analysis of consecutively recruited patients with enlarged and dysmorphic filtration blebs who were managed with conjunctival compression sutures and subconjunctival autologous blood injections. Under topical anaesthesia, conjunctival (8.0-9.0 Nylon or 8.0 Vicryl) compression sutures were placed either side of blebs that were not showing signs of spontaneous resolution. In each case up to 0.75 ml of autologous blood was then injected into the areas of the bleb to be flattened. Supplemental injections of autologous blood were given in clinic as required.
Results: In 11 eyes of 11 patients, conjunctival compression sutures were placed and autologous blood was injected, on average, 568 days following filtration surgery (range 41–2023). Supplemental autologous blood injections were required in eight patients, with three injections being given in one patient. In each case, the sutures were well tolerated and satisfactory compression of the conjunctiva was achieved. The highest intraocular pressure following injection was 25 mm Hg (mean 17.3, SD 4.2) and in none of the cases did blood enter the anterior chamber or parts of the filtration bleb bounded by the sutures.
Conclusion: Conjunctival compression sutures with autologous blood provide a simple and effective means for remodelling the filtration bleb. The procedure can be performed under topical anaesthesia and does not hinder further bleb surgery, should this be required.
Keywords: filtration bleb
The desired result of filtering surgery is a long term reduction of intraocular pressure (IOP) with minimal impact on visual function and patient comfort. The morphology of the filtration bleb is an important factor in achieving this aim. Ideally, the bleb should be diffuse and cause as little change as possible of the ocular surface contour. In the majority of cases the bleb is relatively asymptomatic. In some patients, however, bleb morphology is unsatisfactory and can cause considerable discomfort.1 Asymmetric scarring at the filtration site can result in the formation of elevated blebs that encroach on the cornea which, if sufficiently large, can result in elevation of the upper lid. Disruption of the tear film can ensue, leading to the formation of dellen.2 Diffusely enlarged blebs tend to result from overfiltration and can be associated with a significant reduction in visual acuity secondary to ocular hypotony.3 In the early postoperative period spontaneous resolution can be expected for moderate degrees of overfiltration. However, with long standing hypotony or significant bleb dysmorphology, surgical intervention is usually required.
The treatment of these dysmorphic or overfiltering blebs includes conjunctival cryotherapy,4 suturing of the bleb, bleb excision,5 and scleral6,7 or conjunctival grafts,8 each of which carries a significant risk of postoperative complications. Autologous fibrin9 or blood10 have been used to seal any points of overfiltration or leakage. Blood is useful in that it can affect large areas of conjunctiva but has the disadvantage that marked increases in IOP can occur if blood tracks into the anterior chamber.11,12
Recently, conjunctival compression sutures have been used to induce adherence of conjunctiva to underlying tissues.13,14 The limitation of this technique is that it only affects the area of conjunctiva that is compressed and in our hands this has been insufficient in cases with diffuse conjunctival chemosis. However, when these sutures are used with the subconjunctival injection of autologous blood they can provide an effective management of hypotonous maculopathy following filtration surgery with mitomycin C.15 We now report our experience with a development of this technique in which we have combined the use of the compression suture with the subconjunctival injection of autologous blood for the management of chronic diffusely enlarged filtration blebs.
METHODS
Patients were considered for treatment if they had enlarged and uncomfortable filtration blebs for at least 1 month following trabeculectomy that were not showing signs of resolution. Following informed consent, topical anaesthesia was achieved using 1% amethocaine or 0.5% benoxinate drops delivered 5 minutes before surgery. Supplemental drops were given as required. Once the conjunctiva was sufficiently anaesthetised, a suture was placed just anterior to the limbus at 50% of the corneal stromal depth. The first case in the series had a compression suture with 8.0 Vicryl (Ethicon, Bracknell, UK); all subsequent procedures were performed with 8.0 or 9.0 Nylon (Monofilament Nylon, Alcon Surgical, Hemel Hempstead, UK) on a cutting or round bodied needle. The suture then ran posteriorly to compress the underlying conjunctiva either side of the central portion of the filtration bleb and was anchored using a deep bite in conjunctiva-Tenon's. Placement of the posterior suture was facilitated by having the patient look inferiorly as much as possible. In one case, a corneal traction suture was required to achieve sufficient globe depression. Once satisfactory conjunctival compression was achieved the suture ends were tied to achieve the required degree of conjunctival compression. Depending on the extent and location of conjunctival chemosis, a second compression suture was then placed on the other side of the filtration bleb.
At this point blood was drawn from the patient's antecubital vein and 0.1 to 0.2 ml injected subconjunctivally on the side of the compression sutures away from the filtration bleb. When two conjunctival sutures were inserted, injections were therefore made on either side of the bleb. Supplemental injections of blood (to a total volume of 0.75 ml) were made further away from the centre of the filtration bleb to ensure each subconjunctival haematoma covered at least 3 clock hours of bulbar conjunctiva.
Chloramphenicol 0.5% drops (Chauvin, Romford, UK) were given three to four times a day. Topical steroids were not given in order to encourage scarring at the site of the compression. Patients were examined on the first postoperative day and then at weekly intervals for the first month. Sutures were kept in place for at least 8 weeks and then removed at various times once scarring lines were seen in the compressed conjunctiva, or the suture had become loose. For each case, the outcome of surgery was determined by retrospective review of the patients notes.
RESULTS
Eleven eyes from 11 patients were considered suitable for the strap sutures with subconjunctival injection of autologous blood. The mean age of the patients was 68 years (range 47–78, Table 1) of which six were male and five female. All patients had undergone uncomplicated filtration surgery and had then developed diffuse areas of conjunctival chemosis with symptomatic elevation of the filtration bleb. The chemosis affected 90–360 degrees of conjunctiva in eight eyes and 360 degrees in three eyes. In one case the tear film abnormality associated with conjunctival chemosis had resulted in the formation of a dellen. One patient had received two previous treatments for conjunctival chemosis secondary to overfiltration, cryotherapy to either side of the filtration bleb, and conjunctival suturing in combination with excision of bullous conjunctiva. In spite of these treatments, conjunctival chemosis had reoccurred. Ocular hypotony (IOP of 5 mm Hg or less) was present in five cases; in none of the cases could an aqueous leak or cyclodialysis cleft be demonstrated. One case had choroidal (macula) folds but none were noted to have choroidal effusions at the time of treatment. Antifibroblastic agents (5-fluorouracil or mitomycin C) had not been used in any of the cases.
Table 1.
Patient details
| Case | Age | Interval (days) | Extent (degrees) | Repeat injection* | Preop IOP | Highest IOP | Final IOP |
| 1 | 77 | 89 | 270 | 0 | 9 | 20 | 15 |
| 2 | 68 | 270 | 180 | 1 | 5 | 20 | 15 |
| 3 | 67 | 41 | 360 | 0 | 7 | 14 | 10 |
| 4 | 64 | 252 | 120 | 1 | 12 | 20 | 16 |
| 5 | 76 | 692 | 360 | 1 | 12 | 17 | 14 |
| 6 | 78 | 1038 | 360 | 2 | 12 | 16 | 14 |
| 7 | 62 | 123 | 270 | 1 | 5 | 19 | 8 |
| 8 | 67 | 1483 | 100 | 0 | 8 | 25 | 10 |
| 9 | 72 | 161 | 180 | 1 | 2 | 16 | 10 |
| 10 | 68 | 2023 | 90 | 2 | 2 | 9 | 7 |
| 11 | 47 | 70 | 90 | 3 | 0 | 14 | 5 |
*These injections refer to additional subconjunctival injections of autologous blood that were given in clinic.
Sutures were placed on each side of the central portion of the overdraining bleb in 10 eyes while a single suture was placed to one side of the bleb in one eye. The mean interval from filtration surgery to the placement of strap sutures was 461 days (range 41–2023). The sutures could be placed with ease under topical anaesthesia.
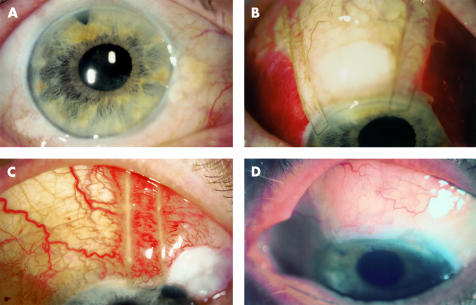
A typical preoperative case is shown in Figure 1A, in which overfiltration has resulted in 360 degrees of conjunctival chemosis. Compression sutures placed on each side of an overdraining filtration bleb are shown in Figure 1B. Autologous blood has been injected subconjunctivally either side of the bleb. It was important that the sutures were pulled tight to ensure adequate conjunctival compression. Blood did not track into the anterior chamber in this or in any of the other cases. The case in which a single strap suture was inserted is shown in Figure 1C and here, the volume of injected blood was reduced to ensure that blood did not track to the unguarded side of the bleb. In each case the subconjunctival haematoma resolved within 4 weeks, by which time sutures were usually subepithelial. Figure 1C shows the degree of inflammation that typically occurred around a compression suture within the first month of placement.
Figure 1.
(A) Pretreatment photograph of case 6 showing 360 degrees of conjunctival chemosis persisting 1038 days following filtration surgery. (B) Photograph of the same eye 1 day after injection of subconjunctival blood and placement of compression sutures. The IOP was 16 mm Hg. No blood has entered the filtration bleb or anterior chamber. The eye has been tilted inferiorly and the pupil is slightly more dilated, obscuring the peripheral iridotomy in this view. (C) Photograph of case 2 after blood injection. Conjunctival chemosis originated at the nasal aspect of the bleb, whereas the temporal aspect was flat. A single compression suture was therefore used. Note the conjunctival injection underlying the compression suture. The highest IOP for this eye was 20 mm Hg. (D) Final review photograph of case 5 showing linear conjunctival scarring and flattening of the conjunctiva after compression sutures and autologous blood. The compression sutures have been removed.
The mean follow up period was 45 weeks (range 8–81), with sutures remaining in place on average for 15 weeks (range 8–23). Repeat subconjunctival blood injections were required in eight cases, and these were given at the slit lamp under topical anaesthesia (benoxinate 0.5%) using a 25 gauge needle. A third injection was required in one case.
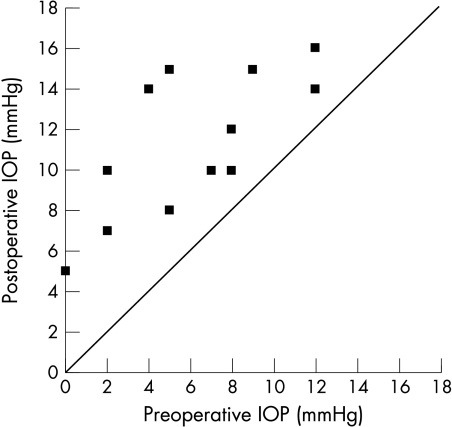
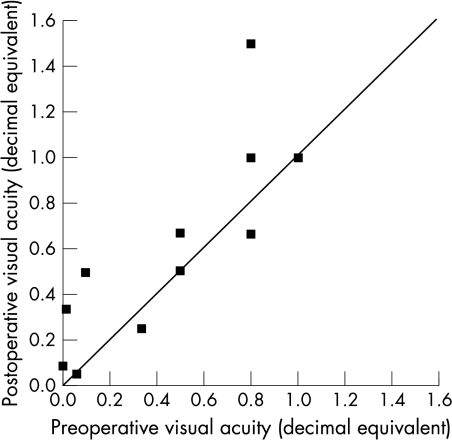
Satisfactory resolution of the conjunctival chemosis was achieved in every case, an example of which is shown in Figure 1D. The change in IOP that occurred following treatment is shown in Table 1. Only moderate increases in IOP were seen immediately following the procedure, the highest postoperative pressure being 20 mm Hg. No case demonstrated a post-injection pressure spike. At final review, the mean IOP was 11.3 mm Hg (range 5–16). The preoperative and final postoperative IOPs are plotted in Figure 2, showing that a moderate increase in IOP occurred following resolution of the conjunctival chemosis. A slight improvement in visual acuity was seen in three cases, as shown in Figure 3.
Figure 2.
Plot of postoperative IOP against preoperative IOP (mm Hg). The line of equivalence is shown.
Figure 3.
Plot of postoperative visual acuity against preoperative visual acuity. Visual acuities are expressed as decimal equivalents such that 6/6 =1 and 6/60 = 0.1. The line of equivalence is shown.
DISCUSSION
We have described a simple technique for the management of diffuse conjunctival chemosis associated with the overdraining filtration bleb. Our patients were carefully selected as those who had long standing symptomatic chemosis following filtration surgery. All 11 patients were successfully treated using this technique, as measured by complete resolution of the chemosis. Since the chemosis had been present for some time before surgery, we think it unlikely that our results are due to spontaneous resolution. However, the question remains as to the relative importance of the conjunctival sutures and the autologous blood.
Both techniques have been reported to be successful in the management of ocular hypotony16 and it can be argued that compression on its own may have been sufficient. However, we think that the use of autologous blood was the key factor for two reasons. Firstly, in eight of the 11 cases, conjunctival chemosis resolved only after repeat blood injection even though the compression sutures had achieved adequate conjunctival compression. Secondly, in one of the cases the conjunctiva had been sutured to the underlying sclera in an attempt to reduce the size of the bleb, which on its own had been unsuccessful in resolving the chemosis. In the light of these considerations, we therefore combined the two techniques from the outset in the management of these patients.
Although the technique is simple, it is not entirely straightforward. Successful compression is dependent on the secure placement of the posterior suture, which can be difficult, particularly in eyes with marked chemosis. In these cases, compression of the conjunctiva with a cotton tip applicator just prior to suture placement can help in judging the depth at which the suture should be placed. Small cuts can also be made in the conjunctiva to release some of the retained fluid to facilitate the required level of compression (all cases remained Seidel negative following treatment, possibly due to the effect of the autologous blood). It is important that broad bites are taken since the sutures can tear out when compression is applied. As a result of these safeguards, no blood entered the filtration site of the anterior chamber and marked increases in IOP were not seen after injection; this is an important consideration when dealing with patients with advanced optic disc cupping.11,12
A major advantage of this technique is that it is minimally invasive. Although most of the sutures were subconjunctival by the first month after insertion they could easily be located and removed at the corneal limbus as required. The use of these sutures does not preclude the performance of more complicated surgery should the procedure be unsuccessful. One of the limitations is that some conjunctival healing response is required to ensure persistent compression adjacent to the filtration site. Since antifibroblastic agents had not been used in the eyes in this series, the sutures had been applied to sectors of the conjunctiva in which the fibroblasts are viable and able to make a sufficient healing response. It is likely that the suture may also have a role in the management of acellular blebs since they have been reported to thicken bleb tissue and to promote vascularity.13
Fortunately the incidence of conjunctival chemosis secondary to overfiltration is low and the use of compression sutures, even in a large glaucoma practice, is likely to be infrequent. Some indication can be obtained from the frequency of long term hypotony, which ranged from 1–2% in one large series.17
In summary, the placement of compression sutures with autologous blood is a simple and effective technique for dealing with enlarged, dysmorphic filtration blebs. The compression sutures prevent the entry of blood into the anterior chamber, thereby avoiding marked increases in intraocular pressure. The procedure can be performed under topical anaesthesia, is well tolerated and, since the sutures can easily be removed, should not restrict further conjunctival surgery.
Video Reports (www.bjophthalmol.com).
Capsule staining and mature cataracts: a comparison of indocyanine green and trypan blue dyes. D F Chang
Pearls for implanting the Staar toric IOL. D F Chang
An intraocular steroid delivery system for cataract surgery. D F Chang
Evaluation of leucocyte dynamics in mouse retinal circulation with scanning laser ophthalmoscopy. H Xu, A Manivannan, G Daniels, J Liversidge, P F Sharp, J V Forrester, I J Crane
Dipetalonema reconditum in the human eye. T Huynh, J Thean, R Maini
Surgical revision of leaking filtering blebs with an autologous conjunctival graft. K Taherian, A Azuara-Blanco
Thixotropy: a novel explanation for the cause of lagophthalmos after peripheral facial nerve palsy. M Aramideh, J H T M Koelman, P P Devriese, F VanderWerf, J D Speelman
Acknowledgments
Presented in part at the Association for Research in Vision and Ophthalmology, Fort Lauderdale, Florida, USA, May 1998
We thank Gill Bennerson for her expert photographic assistance.
Proprietary interest: None.
REFERENCES
- 1.Budenz DL, Hoffman K, Zacchei A. Glaucoma filtering bleb dysesthesia. Am J Ophthalmol 2001;131:626–30. [DOI] [PubMed] [Google Scholar]
- 2.Soong H, Quigley H. Dellen associated with filtering blebs. Arch Ophthalmol 1983;101:385–7. [DOI] [PubMed] [Google Scholar]
- 3.Burney E, Quigley H, Robin A. Hypotony and choroidal detachment as late complications of trabeculectomy. Am J Ophthalmol 1987;103:685–8. [DOI] [PubMed] [Google Scholar]
- 4.Costa V, Smith M, Spaeth G, et al. Loss of visual acuity after trabeculectomy. Ophthalmology 1993;100:599–612. [DOI] [PubMed] [Google Scholar]
- 5.Azuara-Blanco A, Katz L. Dysfunctional filtering blebs. Surv Ophthalmol 1998;43:93–126. [DOI] [PubMed] [Google Scholar]
- 6.Kosmin A, Wishart P. A full thickness scleral graft for the surgical management of a late filtration bleb leak. Ophthalmic Surg 1997;28:461–8. [PubMed] [Google Scholar]
- 7.Melamed S, Ashkenazi I, Belcher D, et al. Donor scleral graft patching for persistent filtration bleb leak. Ophthalmic Surg 1991;22:164–5. [PubMed] [Google Scholar]
- 8.Buxton J, Lavery K, Liebmann J, et al. Reconstruction of filtering blebs with free conjunctival autografts. Ophthalmology 1994;101:635–9. [DOI] [PubMed] [Google Scholar]
- 9.Graham S, Murray B, Goldberg I. Closure of fornix-based post trabeculectomy conjunctival wound leaks with autologous fibrin glue. Am J Ophthalmol 1992;114:221–2. [DOI] [PubMed] [Google Scholar]
- 10.Motuz Leen M, Moster M, Jay Katz L, et al. Management of overfiltering and leaking blebs with autologous blood injection. Arch Ophthalmol 1995;113:1050–5. [DOI] [PubMed] [Google Scholar]
- 11.Zaltas M, Schuman J. A serious complication of intrableb injection of autologous blood for the treatment of postfiltration hypotony. Am J Ophthalmol 1994;118:251–3. [DOI] [PubMed] [Google Scholar]
- 12.Alward W. Marked intraocular pressure rise following blood injection into a filtering bleb. Arch Ophthalmol 1995;113:1232–3. [DOI] [PubMed] [Google Scholar]
- 13.Palmberg P, Zacchei A. Compression sutures—a new treatment for leaking or painful filtering blebs. Invest Ophthalmol Vis Sci 1996;37:S444. [Google Scholar]
- 14.Palmberg P. Late complications after glaucoma filtering surgery. In: Leader B, Calckwood J, eds. Proceedings of the 45th Annual Symposium of the New Orleans Academy of Ophthalmology. The Hague: Kugler Publications, 1996.
- 15.Haynes WL, Alward WL. Combination of autologous blood injection and bleb compression sutures to treat hypotony maculopathy. J Glaucoma 1999;8:384–7. [PubMed] [Google Scholar]
- 16.Smith M, Sherwood M, Doyle J, et al. Results of intraoperative 5-fluoruracil supplementation on trabeculectomy for open angle glaucoma. Am J Ophthalmol 1992;114:737–41. [DOI] [PubMed] [Google Scholar]
- 17.Watson P, Jakeman C, Ozturk M, et al. The complication of trabeculectomy (a 20 year follow-up). Eye 1990;4:425–38. [DOI] [PubMed] [Google Scholar]