Abstract
Aims: To report the clinical features and outcomes of polypoidal choroidal vasculopathy (PCV) in Chinese patients with or without laser treatment.
Methods: A consecutive series of 204 indocyanine green angiographies (ICGA) performed for patients with a provisional diagnosis of age related macular degeneration were reviewed retrospectively. Inclusion criteria were ICGA with angiographic features of PCV and patients of Chinese ethnic origin. Medical records were then reviewed and patients were recalled for further assessments.
Results: 22 eyes of 19 patients (9.3%) were included. The mean follow up period was 27.4 months (range 4–60 months). The mean age of patients at presentation was 65.1 years (range 51–77 years). The commonest clinical feature at presentation was subretinal haemorrhage (63.6%), followed by retinal exudation (59.1%) and haemorrhagic pigment epithelial detachment (59.1%). There was a predominance of males (68.4%), unilaterality (84.2%), and macular location of polyps (63.6%). Nine eyes received laser photocoagulation. The median initial visual acuity for both the laser and non-laser groups was 6/18. Stable or improved vision was attained in 56% and 31% of laser and non-laser groups, respectively (Fisher’s exact test, p=0.38). Mean loss of Snellen lines was 3.1 and 1.1 for the two groups, respectively (two sample t test, p=0.31). At the last follow up, 15 (68.2%) eyes had poor visual acuity of 6/60 or worse, mostly attributed to disciform scar or exudative maculopathy.
Conclusions: There is a predominance of males, unilaterality, and macular location of polyps in Chinese patients with PCV. The overall visual prognosis is guarded regardless of treatment. There is a large amount of variation in the natural course of PCV among different ethnic groups.
Keywords: Chinese, choroidal vasculopathy, laser photocoagulation
Idiopathic polypoidal choroidal vasculopathy was first described by Yannuzzi in 1982 as a cause of recurrent haemorrhagic pigment epithelial detachment.1 Since then, various terms have been used to describe this disorder including “posterior uveal bleeding syndrome,” “multiple recurrent retinal pigment epithelial detachments in black women,” and “polypoidal choroidal vasculopathy” (PCV).2–5 The lesions in PCV arise from the inner choroidal vascular network with the clinical appearance of aneurysmal reddish orange, spheroidal polyp-like terminations.5,6 The disorder seems to have a predilection to occur in darkly pigmented individuals like black people.6 Indocyanine green angiography (ICGA) is the tool of choice for diagnosing PCV.7 With the increasing widespread use of ICGA and awareness of the disorder throughout the world, reports describing PCV in ethnic groups like white people and Japanese people have been published.8–11
The potential treatments of PCV include ICGA guided laser photocoagulation, which has been used successfully in treating polypoidal lesions in selected cases.5,12–14 Laser treatment is advocated if subretinal fluid, hard exudate, or haemorrhage threatens or involves the fovea.5 In some cases with thick submacular haemorrhage, surgical removal of the subretinal blood followed by laser photocoagulation has also been performed with beneficial effects.15 However, the optimal management of PCV is still uncertain, as the number of cases reported in the literature is not large, the natural course of PCV in different races may be different, and no randomised controlled clinical trial has been performed to see whether laser treatment is beneficial.
The purpose of this study is to analyse the clinical features and outcomes of PCV in Chinese patients with or without laser treatment.
MATERIALS AND METHODS
A consecutive series of 204 ICGA performed in our tertiary referral institutes for patients with a provisional diagnosis of age related macular degeneration were reviewed retrospectively from 1 May 1996 to 30 December 2000. Inclusion criteria were ICGA with angiographic features of PCV and patients of Chinese ethnic origin. Medical records of the patients were reviewed to collect data on the clinical history and clinical findings of the disease. Patients were then recalled for further assessments. Supplementary details on ocular and systemic diseases were obtained with the clinical data crosschecked. A complete ophthalmic examination was then performed which included the best corrected visual acuity, slit lamp examination with biomicroscopy, and binocular indirect ophthalmoscopy. The visual acuity was measured using Snellen charts, and the data were transformed into a number for statistical analysis, by a scale of 16 lines, which ranged from line 1 representing 6/6 to line 16 representing light perception.
Fundus photography, fluorescein angiography (FA), and ICGA were performed through a fundus camera with images digitally stored and processed (Imagenet 2000, Topcon, Paramus, NJ, USA). All images were reviewed on a computer monitor to get the optimal magnification and image enhancement. Indocyanine green (ICG) dye was given intravenously as a single bolus of 50 mg with the last photographs taken at least 30 minutes after the injection. Informed consent was obtained in all patients before angiographies.
The polyps were defined by ICGA when one or more focal vascular dilatations in the inner choroid were seen in the early phase of ICGA. In the late phase of ICGA, the core of the polypoidal lesions may become hypofluorescent due to washout of the dye and show a ring-like staining of the polyps. This might not be seen if there was active leakage from the polyps. The location of the polyps was defined as macular when they were within the temporal vascular arcade, or peripapillary when the polyps were located within one disc diameter from the optic disc margin.
In symptomatic cases, the option of observation versus treatment such as laser photocoagulation would be explained to patients. In cases where patients preferred the latter, argon or diode laser photocoagulation was performed directly on the dilated polypoidal terminals as guided by ICGA. These cases included both peripapillary and macular polypoidal lesions in symptomatic patients. The end point of the laser treatment was to create moderate intense laser burns for the closure of the polypoidal lesions.
For statistical analyses, Fisher’s exact test and two sample t test were performed. A p value of 0.05 or less was considered to be statistically significant.
RESULTS
Among the 204 ICGA reviewed, 22 eyes of 19 patients (9.3%) met the inclusion criteria. All except one patient, who has emigrated, came back for clinical re-evaluation. The Chinese ethnic origin in these 19 patients was confirmed by questioning the family history of the two previous generations.
Demographic details
The mean age of the patients at the time of presentation was 65.1 years (range 51–77 years). There was a male predominance (68.4%) in this study with 13 men and six women. The mean follow up period was 27.4 months (range 4–60 months). Three of the 19 patients (15.8%) had bilateral disease as shown clinically and angiographically. Other demographic details and clinical features of the patients was listed in Table 1.
Table 1.
Demographic and clinical features of patients (n=19, 22 eyes)
| Patient No | Sex/age | Eye | Follow up (months) | Initial BCVA | Final BCVA | Change of lines | Location of polyps | Laser | Medical disease | Ocular disease | Reason for poor visual outcome |
| 1 | F/70 | Left | 44 | 6/12 | 6/15 | Within 1 line | P | Yes | Nil | Nil | NA |
| 2 | M/63 | Right | 38 | 6/12 | FC | −8 | M | No | Smoker | Nil | Disciform scar |
| 3 | F/77 | Left | 24 | 1/60 | FC | Within 1 line | M | No | Nil | IOL | Exudative maculopathy |
| 4 | F/52 | Right | 12 | 6/30 | 6/60 | −2 | M | No | Smoker | Nil | Disciform scar |
| 5 | F/56 | Right | 24 | 6/18 | FC | −8 | M | No | Smoker | Nil | Disciform scar |
| 6 | F/62 | Right | 16 | 6/90 | FC | −2 | M | Yes | IHD, smoker | Nil | Disciform scar |
| 7 | F /72 | Right | 60 | 6/12 | 6/60 | −7 | P | No | Nil | Nil | Exudative maculopathy |
| 8 | M/67 | Right | 4 | 6/60 | 6/60 | Within 1 line | P | No | Nil | Nil | Disciform scar |
| 9 | F/72 | Right | 5 | 6/30 | 6/18 | +3 | M | No | Nil | Nil | NA |
| 10 | M/68 | Right | 37 | 6/18 | 6/120 | −7 | P | Yes | COAD | Nil | Disciform scar |
| 11 | M/76 | Left | 24 | 6/60 | 6/120 | −2 | M | No | DM | Nil | Exudative maculopathy |
| 12 | M/64 | Left | 60 | 6/18 | 6/60 | −5 | M | No | Nil | Nil | Disciform scar |
| M/64 | Right | 60 | 6/15 | 6/120 | −9 | M | Yes | Nil | Nil | Disciform scar | |
| 13 | M/61 | Left | 22 | 6/60 | LP | −5 | M | No | Nil | IOL, high myope | Myopic maculopathy |
| 14 | M/65 | Right | 27 | 6/60 | 6/120 | Within 1 line | M | Yes | DM, HT, IHD | IOL | Disciform scar |
| 15 | M/63 | Right | 21 | 6/18 | 6/18 | +3 | P | Yes | Nil | VH and phthisis bulbi in left eye | NA |
| 16 | M/68 | Right | 8 | 6/60 | 6/15 | +6 | M/P | Yes | Nil | Nil | NA |
| 17 | F/59 | Right | 18 | 6/30 | 6/60 | −2 | M | Yes | Nil | Nil | Exudative maculopathy |
| F/59 | Left | 18 | 6/21 | 6/15 | +2 | M | Yes | Nil | Nil | NA | |
| 18 | F/51 | Right | 60 | 6/18 | 6/120 | −6 | M | No | Nil | Nil | Disciform scar |
| 19 | M/71 | Right | 17 | 6/7.5 | 6/7.5 | Within 1 line | P | No | DM | Nil | NA |
| M/71 | Left | 17 | 6/9 | 6/9 | Within 1 line | P | No | DM | IOL | NA |
BCVA = best corrected visual acuity, M = macular, COAD = chronic obstructive airway disease, P = peripapillary, DM = diabetes mellitus, VH = vitreous haemorrhage, HT = hypertension, IOL = intraocular lens, IHD = ischaemic heart disease, NA = not applicable.
Medical history
Eleven of the 19 patients (57.9%) had no significant past medical illness. Three patients had diabetes mellitus. One patient was taking antihypertensive treatment for essential hypertension. Ischaemic heart disease was noted in two patients. Four patients were smokers.
Symptoms on presentation
The commonest presenting symptom was blurring of vision (57.9%, 11 of 19 patients). Other symptoms included metamorphopsia, floaters, and central scotoma. One patient was asymptomatic and was found to have PCV on routine examination for diabetic retinopathy. The duration of symptoms ranged from 1 week to 20 years.
Visual acuity on presentation (Table 2)
Table 2.
Visual acuity of patients (n=22 eyes)
| Eyes on presentation | Eyes on last follow up | |||||
| Visual acuity | Non-treated group (n=13) | Laser group (n=9) | Total (n=22) | Non-treated group (n=13) | Laser group (n=9) | Total (n=22) |
| ≥6/12 | 4 (30.8) | 1 (11.1) | 5 (22.7) | 2 (15.4) | 1 (11.1) | 3 (13.6) |
| <6/12 to >6/60 | 5 (38.5) | 5 (55.6) | 10 (45.5) | 1 (7.7) | 3 (33.3) | 4 (18.2) |
| ≤6/60 | 4 (30.8) | 3 (33.3) | 7 (31.8) | 10 (76.9) | 5 (55.6) | 15 (68.2) |
(%) = percentage of the corresponding subgroup.
On presentation, five of the 22 eyes (22.7%) had a visual acuity better or equal to 6/12. Ten (45.5%) eyes had visual acuity between 6/15 and 6/60. The remaining seven (31.8%) eyes had visual acuity equal to or worse than 6/60 on presentation.
Fundus features on presentation (Table 3)
Table 3.
Fundus findings on presentation (n=19, 22 eyes)
| Clinical feature | No of eyes (%) |
| Subretinal haemorrhage | 14 (63.6) |
| Retinal exudate | 13 (59.1) |
| Haemorrhagic pigment epithelial detachment | 13 (59.1) |
| Serous pigment epithelial detachment | 5 (22.7) |
| Retinal haemorrhage | 5 (22.7) |
| Visible polyp | 4 (18.2) |
| Diffuse retinal pigment epithelial degeneration | 3 (13.6) |
| Drusen | 2 (9.1) |
| Serous retinal detachment | 1 (4.5) |
| Vitreous haemorrhage | 1 (4.5) |
The commonest clinical feature was subretinal haemorrhage (63.6%). This was followed by retinal exudation (59.1%) and haemorrhagic pigment epithelial detachment (PED) (59.1%). Serous PED was observed in five (22.7%) eyes. Retinal haemorrhage was seen in five (22.7%) eyes, and diffuse retinal pigment epithelial degeneration was seen in three (13.6%) eyes. Serous retinal detachment was only found in one eye. There was also one case of mild vitreous haemorrhage due to breakthrough bleeding from the polyps. The presence of drusen was rare and was only observed in two (9.1%) eyes. The characteristic polyps in PCV were seen during clinical examination with slit lamp biomicroscopy in four (18.2%) eyes.
Findings of ICG angiography
The characteristic feature of PCV in ICGA was early choroidal vascular hyperfluorescent showing up the abnormal choroidal vascular polyps. These were observed in all cases in our study. The majority of polyps and localised hyperfluorescent lesions with terminal branching were seen within the first minute after injection of ICG dye. The polyps were found in the macular area in 14 (63.6%) eyes and in the peripapillary areas in seven (31.8%) eyes. One (4.5%) eye had both peripapillary and macular lesions (case 1).
Visual outcome of non-laser group and laser group (Tables 2 and 4)
Table 4.
Change in visual acuity of patients (n=22 eyes)
| Change in visual acuity | Non-treated group (n=13) | Laser group (n=9) |
| Decrease of 2 or more lines | 9 (69.2%) | 4 (44.4%) |
| Stable within 1 line | 3 (23.1%) | 2 (22.2%) |
| Increase of 2 or more lines | 1 (7.7%) | 3 (33.3%) |
(%) = percentage of the corresponding subgroup.
Thirteen eyes did not receive laser treatment. The mean follow up period of these patients was 28.2 months (range, 4–60 months). The median initial visual acuity for the non-laser group was 6/12 (range, 6/7.5 to 1/60). At the last follow up, three (23.1%) eyes had visual acuity within one Snellen line of initial visit. Only one (7.7%) eye had improvement of two or more Snellen lines. The remaining nine (69.2%) eyes had a gradual decrease of visual acuity of two or more Snellen lines. The mean loss of Snellen lines for this non-laser group was 3.1. Ten (76.9%) of these 13 eyes had a final visual acuity of 6/60 or worse, with five (38.5%) eyes having a final visual acuity of 6/60 or worse.
Nine eyes received laser photocoagulation. The mean follow up period of these patients was 27.7 months (range, 8–60 months). The median visual acuity for the laser group was 6/18 (range 6/12 to 6/90). There is no difference in the follow up period between the laser and non-laser groups (two sample t test, p=0.94). Two of the patients required repeated laser treatments for recurrent or persistent lesions. The mean number of laser shots performed was 97.6 (range 29–194). The laser treatment spot size ranged from 50 μm to 200 μm. The highest energy level of the laser treatment ranged from 100 mW to 400 mW.
Among these laser treated eyes, three (33.3%) had improvement of two or more Snellen lines while two (22.2%) had the visual acuity of within one Snellen line at the last visit as compared to the first visit. Four other eyes (44.4%) have decreased visual acuity of two or more lines compared with that on presentation. Stable or improved vision was attained in 56% and 31% of laser and non-laser groups, respectively (Fisher’s exact test, p=0.38). The mean loss of Snellen lines for the treated group was 1.1 lines. The difference in loss of lines between the laser and non-laser groups was not statistically significant (two sample t test, p=0.31). Five (55.6%) of these nine eyes had a final visual acuity of 6/60 or worse, with three (33.3%) eyes having a final visual acuity of 6/120 or worse.
For the laser treated and the non-laser treated groups, there is no statistical difference between two groups with respect to final visual acuity of 6/60 or worse, as well as 6/120 or worse (Fisher’s exact test, p=0.38 and p = 1.0, respectively).
Reasons for poor outcome (Table 1, Table 4)
Of the 15 eyes that had poor visual acuity of 6/60 or worse at the last follow up, 10 (66.7%) were due to the formation of a disciform scar, four (26.7%) were due to exudative maculopathy. Among these 14 eyes with disciform scar and exudative maculopathy, nine (64.3%) and five (35.7%) eyes were from the untreated and lasered group, respectively. There was no statistically significant difference between the number of eyes with disciform scar formation and exudative maculopathy in the lasered and untreated group (Fisher’s exact test, p=0.66).
Selected case reports
Case 1 (patient No 16)
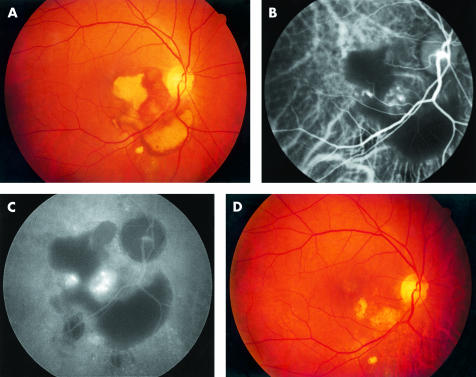
A 68 year old Chinese man presented with a 1 week history of sudden decrease in vision over the right eye. On examination, his visual acuity was 6/60 and 6/9 over the right and left eye, respectively. Dilated fundal examination of the right eye showed a partially reabsorbed, irregularly “C”-shaped subretinal haemorrhage involving the fovea and the inferior macula, extending to the inferior peripapillary area. The total size of the lesion was about four disc areas. Medial to the haemorrhage, there was a reddish subretinal heterogeneous lesion of about a half disc diameter (Fig 1A). Fundal examination of the left eye was unremarkable. No drusen were noted in either eyes. FA and ICGA showed blocked hypofluorescent in the area of haemorrhage. Additionally, early phase of ICGA showed two clusters of polyps in the inferonasal macula characteristics of PCV (Fig 1B), which leaked moderately at the late phase (Fig 1C). After thorough discussion about the option of observation, laser treatment with or without submacular drainage of blood, the patient preferred laser treatment. Argon laser photocoagulation was directly applied to the polypoidal lesions. Two weeks after laser treatment, there was a marked decrease in subretinal haemorrhage. Visual acuity of the right eye improved to 6/15 2 months after treatment. Repeat FA and ICGA confirmed no recurrence of the polypoidal lesions or leakage. His visual acuity 9 months after laser treatment remained at 6/15 and 6/9 over the right and left eye, respectively (Fig 1D).
Figure 1.
Right eye. (A) Fundus photograph showing a partially reabsorbed, irregularly “C”-shaped subretinal haemorrhage involving the fovea and inferior macula that extended to the inferior peripapillary area. The total size of lesion was about four disc areas. Medial to the haemorrhage, there was a reddish subretinal heterogeneous lesion of about a half disc diameter. (B) Indocyanine green angiogram (early phase, 1 minute 26 seconds) showing multiple polypoidal lesions in two clusters in the inferonasal macula. (C) Indocyanine green angiogram (late phase, 27 minutes 57 seconds) showing moderate leakage from the polypoidal lesions. (D) Fundus photograph 8 months later showing laser scars in the inferonasal macula with surrounding retinal pigment epithelial atrophy.
Case 2 (Patient No 19)
A 70 year old Chinese man presented for screening of diabetic retinopathy. He had previously received an uneventful extracapsular cataract extraction with implantation of intraocular lens in the right eye 2 years earlier. His visual acuity was 6/9 and 6/7.5 over the right and left eye, respectively. Dilated fundal examination showed no evidence of diabetic retinopathy over both eyes. However, two small haemorrhagic PEDs with associated retinal haemorrhage were seen in the superotemporal peripapillary region over the left eye (Fig 2A). The lesions appeared to be polyps in the choroidal level. FA showed blocked hypofluorescent by the overlying retinal haemorrhage in the superotemporal peripapillary area. ICGA showed early hyperfluorescent polyps in the peripapillary regions of both eyes (Fig 2B). Late phase of ICGA showed the classic ring-like silhouette staining of the polyps (Fig 2C). The lesions were not treated with laser photocoagulation as the patient was asymptomatic. His vision remained stable 17 months later.
Figure 2.
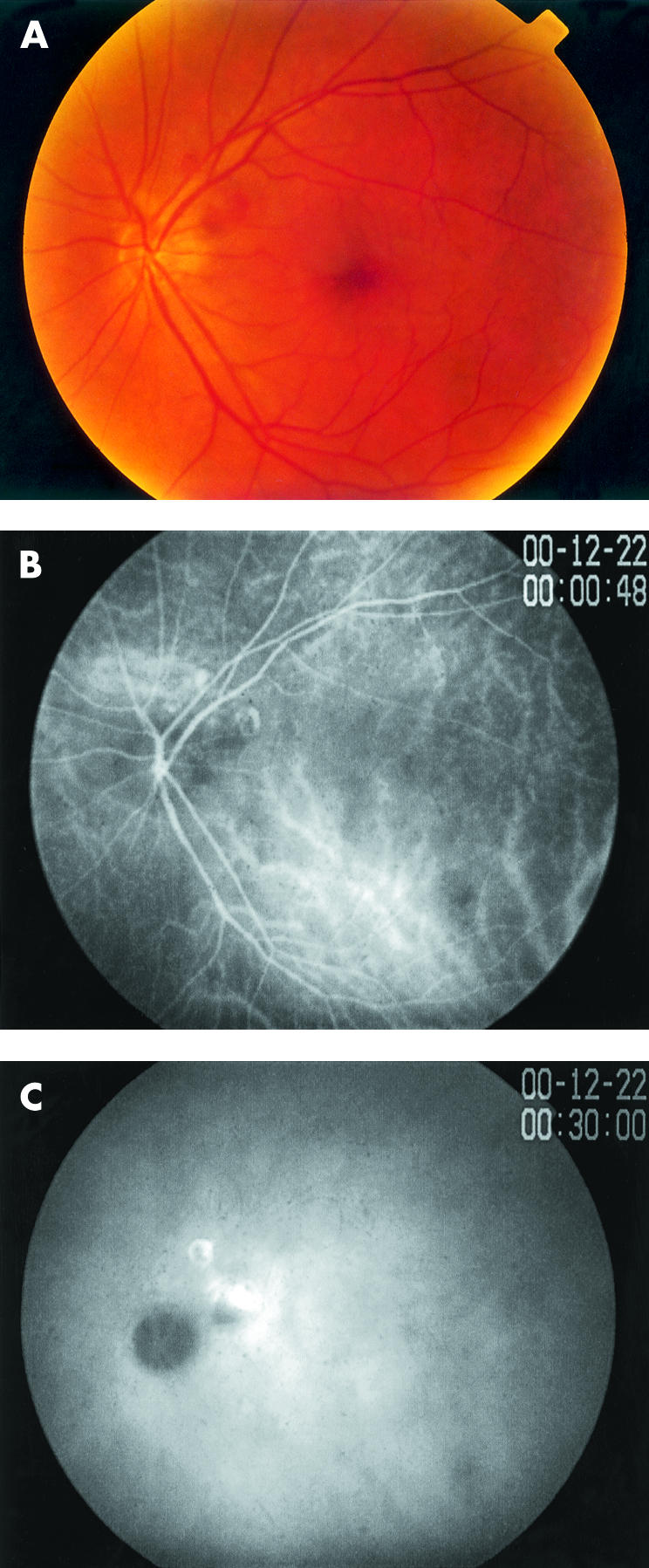
Left eye. (A) Fundus photograph showing two haemorrhagic pigment epithelial detachments with underlying choroidal polyps in the peripapillary region. (B) ICGA (early phase, 0 minutes 48 seconds) showing early hyperfluorescent of the polypoidal lesions. (C) ICGA (late phase, 30 minutes 1 second) showing the classic ring-like silhouette staining of the polyps.
DISCUSSION
Since the original description of PCV by Yannuzzi in 1982 and Stern et al in 1985,1,4 the ophthalmic community throughout the world has become more aware of this disease. PCV has been suggested to be more common in pigmented individuals like black people and Asians. However, no account of this disease exclusively in Chinese patients has been reported. In the present study, only 19 (9.3%) out of 204 patients who had ICGA performed with a provisional diagnosis of age related macular degeneration were found to have PCV. This may suggest that symptomatic PCV in Chinese people is not as common as we have expected. Our institutes serve a population of about three million that enjoys readily accessible medical care at a heavily government subsidised rate. Each consultation that includes angiograms and drugs only costs about £4. However, our study suffers from the limitation of a retrospective study. Some patients might have FA but not ICGA performed. The latter is important in diagnosing PCV. In a similar retrospective study of white elderly people in Italy, the reported frequency was 9.8%.11Table 5 showed the summary of findings of the present and other reported series.6,8–11 In most studies the mean age of presentation was the 60s. However, there is great variation in terms of sex, bilaterality, and location of polyps among different series. Our series showed a predominance of male, unilateral, and macular location of polyps. PCV was thought to be a bilateral peripapillary disease in an early study by Yannuzzi.6 Our study showed that the rate of bilaterality was only 16%, which was similar to that reported by Uyama et al and Scassellati-Sforzolini et al.9,11 Additionally, ours as well as other series suggested a macular predominance of the location of polyps.8,11
Table 5.
Comparison of findings with other PCV studies
| Authors | Ethnic group | No of patients | Mean age | Male sex | Bilaterality | Location of polyps |
| Yannuzzi et al6 (1997) | Black (50%) | 20 | 60 | 15% | 80% | Macular = 25% |
| White (20%) | Peripapillary = 75% | |||||
| Asian (30%) | ||||||
| Lafaut et al8 (2000) | White (100%) | 36 | N/A | 47% | 61% | Macular = 49% |
| Peripapillary = 36% | ||||||
| Arcade = 13% | ||||||
| Midperiphery = 13% | ||||||
| Uyama et al9 (1999) | Japanese (100%) | 32 | 65.7 | 69% | 9% | Macular = 94% |
| Peripapillary = 9% | ||||||
| Ahuja et al10 (2000) | White (74%) | 34 | 65.4 | 35% | 47% | Macular = 68% |
| Black (20%) | Peripapillary = 18% | |||||
| East Asians (6%) | Extramacular = 14% | |||||
| Scassellati-Sforzolini et al11 (2001) | White (100%) | 19 | 73.4 | 47% | 21% | Macular = 53% |
| Peripapillary = 37% | ||||||
| Periphery = 10% | ||||||
| Kwok et al (2002) | Chinese (100%) | 19 | 65.1 | 68% | 16% | Macular = 64% |
| Peripapillary = 32% | ||||||
| Both = 4% |
Ross et al had suggested that certain subgroups of PCV and retinal arterial macroaneurysm might be pathophysiologically related as analogous hypertensive insults to the choroidal and retinal vascular beds.16 It was thought that one third of PCV might be associated with hypertension. In the studies by Ahuji et al10 and Lip et al,14 23.5% and 20% of the patients also had a history of hypertension. However, in our series, only one (5.2%) patient was found to be hypertensive without any evidence of hypertensive retinopathy. It seems that hypertension may not be an important risk factor of PCV in Chinese patients.
Laser treatment of the leaking vascular abnormalities in PCV has been anecdotally described in several studies.5,6,12,15,16 In a larger study by Lafaut et al, 14 eyes received laser photocoagulation to the polyps.8 In the five peripapillary lesions they treated, all the polyps regressed with resolution of the fundal lesions. However, among the nine eyes with polyps in the macula or along major vascular arcades, similar success was only achieved in five eyes. No data on visual outcome were available in this study. Uyama et al performed laser photocoagulation in 17 eyes in which 12 eyes (71%) showed clinical improvement with a decrease of haemorrhage and subretinal fluid.9 Four (24%) eyes worsened with two of them developed disciform scars. However, compared with the untreated group, the latter had a better visual outcome. In a study by Lip et al, laser treatment was performed on three of the five patients.14 The laser treated group had stable vision whereas the vision of patient without laser treatment deteriorated.
In our series, eyes with laser treatment seemed to attain a better visual outcome. Five (56%) eyes in the laser group had stable or improved vision, while only four (31%) untreated eyes achieved the same. The percentages of eyes with poor vision equal to or worse than 6/120 in laser and non-laser groups were 38% and 22%, respectively. However, both comparisons did not reach any statistical significance. This may be partially due to the relatively small sample size. Furthermore, the natural history of PCV has been thought to be less aggressive than that of age related macular degeneration with choroidal neovascularisation. Observation alone might be a sensible alterative in these patients.6,13
In our series, 15 (68.2%) eyes had poor visual acuity of 6/60 or worse at the last follow up. Among them, 10 eyes had disciform scars and four had exudative maculopathy. This suggests an unfavourable course of PCV in Chinese patients. Guarded prognosis has also been suggested in a series of white people.8 However, in a series of 35 Japanese eyes with PCV, 49% attained vision of 6/7.5 or better.9 In a series of eight eyes with PCV of macula, most retained vision of 6/24 or better.13 This supports the suggestion that there is a large extent of variation in the natural course of PCV among different ethnic groups.
In summary, our series showed a predominance of male, unilateral, and macular location of polyps in Chinese patients with PCV. Laser treatment of polyps may be useful, but the overall visual prognosis is guarded regardless of treatment. There is a great variation in the natural course of PCV among different ethnic groups.
Acknowledgments
Financial support: Supported in part by Action for Vision (AFV) Eye Foundation, Hong Kong, People’s Republic of China.
REFERENCES
- 1.Yannuzzi LA. Idiopathic polypoidal choroidal vasculopathy. Presented at the Macula Society Meeting; 5 February 1982; Miami, FL.
- 2.Kleiner RC, Brucker AJ, Johnston RL. The posterior uveal bleeding syndrome. Retina 1990;10:9–17. [PubMed] [Google Scholar]
- 3.Yannuzzi LA, Sorenson J, Spaide RF, et al. Idiopathic polypoidal choroidal vasculopathy (IPCV). Retina 1990;10:1–8. [PubMed] [Google Scholar]
- 4.Stern RM, Zakov ZN, Zegerra H, et al. Multiple recurrent seroangineous retinal pigment epithelial detachments in black women. Am J Ophthalmol 1985;100:560–9. [DOI] [PubMed] [Google Scholar]
- 5.Yannuzzi LA, Wong DW, Sforzolini BS, et al. Polypoidal choroidal vasculopathy and neovascularized age-related macular degeneration. Arch Ophthalmol 1999;117:1503–10. [DOI] [PubMed] [Google Scholar]
- 6.Yannuzzi LA, Ciardella A, Spaide RF, et al. The expanding clinical spectrum of idiopathic polypoidal choroidal vasculopathy. Arch Ophthalmol 1997;115:478–85. [DOI] [PubMed] [Google Scholar]
- 7.Spaide RF, Yannuzzi LA, Slakter JS, et al. Indocyanine green videoangiography of idiopathic polypoidal choroidal vasculopathy. Retina 1995;15:100–10. [DOI] [PubMed] [Google Scholar]
- 8.Lafaut BA, Leys AM, Snyers B, et al. Polypoidal choroidal vasculopathy in Caucasians. Graefes Arch Clin Exp Ophthalmol 2000;238:752–9. [DOI] [PubMed] [Google Scholar]
- 9.Uyama M, Matsubara T, Fukushima I, et al. Idiopathic polypoidal choroidal vasculopathy in Japanese patients. Arch Ophthalmol 1999;117:1035–42. [DOI] [PubMed] [Google Scholar]
- 10.Ahuja RM, Stanga PE, Vingerling JR, et al. Polypoidal choroidal vasculopathy in exduative and haemorrhagic pigment epithelial detachments. Br J Ophthalmol 2000;84:479–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scassellati-Sforzolini B, Mariotti C, Byran R, et al. Polypoidal choroidal vasculopathy in Italy. Retina 2001;21:121–5. [DOI] [PubMed] [Google Scholar]
- 12.Gomez-Ulla F, Gonzalez F, Torreiro MG. Diode laser photocoagulation in idiopathic polypoidal choroidal vasculopathy. Retina 1998;18:481–3. [DOI] [PubMed] [Google Scholar]
- 13.Moorthy RS, Lyon AT, Rabb MF, et al. Idiopathic polypoidal choroidal vasculopathy of the macula. Ophthalmology 1998;105:1380–5. [DOI] [PubMed] [Google Scholar]
- 14.Lip PL, Hope-Ross MW, Gibson JM. Idiopathic polypoidal choroidal vasculopathy: a disease with diverse clinical spectrum and systemic associations. Eye 2000;14:695–700. [DOI] [PubMed] [Google Scholar]
- 15.Shiraga F, Matsuo T, Yokoe S, et al. Surgical treatment of submacular hemorrhage associated with idiopathic polypoidal choroidal vasculopathy. Am J Ophthamol 1999;128:147–54. [DOI] [PubMed] [Google Scholar]
- 16.Ross RD, Gitter KA, Cohen G, et al. Idiopathic polypoidal choroidal vasculopathy associated with retinal arterial macroaneurysm and hypertensive retinopathy. Retina 1996;16:105–11. [DOI] [PubMed] [Google Scholar]