Abstract
Aims: To estimate the magnitude and the causes of blindness through a community based nationwide survey in Oman. This was conducted in 1996–7.
Methods: A stratified cluster random sampling procedure was used to select 12 400 people. The WHO/PBD standardised survey methodology was used, with suitable adaptation. The major causes of blindness were identified among those found blind.
Results: A total of 11 417 people were examined (response rate 91.8%) The prevalence of blindness in the Omani population was estimated to be 1.1% (95% CI 0.9 to 1.3), blindness being defined according to the WHO Tenth Revision of the International Classification of Diseases. Prevalence of blindness was clearly related to increasing age, with estimates of 0.08% for the 0–14 age group, 0.1% for the 15–39 age group, 2.3% for the 40–59 age group, and 16.8% for the group aged 60 +. There was a statistically significant difference between the prevalence in females (1.4%) and males (0.8%). The northern and central regions had a higher prevalence of blindness (1.3% to 3%). The major causes of blindness were unoperated cataract (30.5%), trachomatous corneal opacities (23.7%), and glaucoma (11.5%)
Conclusions: Despite an active eye healthcare programme, blindness due to cataract and trachoma remains a public health problem of great concern in several regions of the sultanate. These results highlight the need, when planning effective intervention strategies, to target the eye healthcare programme to the ageing population, with special emphasis on women.
Keywords: blindness, epidemiology, cataract, trachoma, Sultanate of Oman
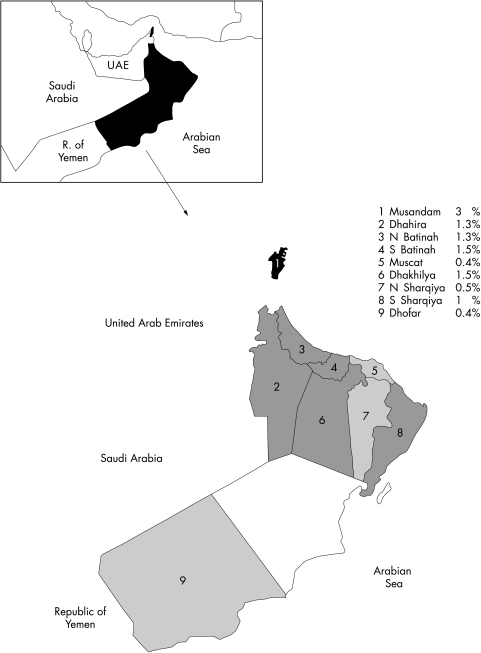
The Sultanate of Oman is located in the south eastern corner of the Arabian Peninsula and has common borders with Saudi Arabia, the United Arab Emirates, and the Republic of Yemen (see Fig 1). The sultanate with 212 460 square kilometres area is the second largest country in the peninsula. The climate is hot and humid in the coastal areas during the summer and hot and dry in the interior with the exception of high mountains and the southern Governate of Dhofar, which has a temperate climate throughout the year.
Figure 1.
Map of the Sultanate of Oman: prevalence of blindness by region (First Administration Unit) (OES 1997). Low prevalence of blindness (light grey area) regions: Muscat, North Sharqiya, Dhofar; causes: cataract 30%, glaucoma 25%, post segment 20%. High prevalence of blindness (dark grey area): regions: Dhahira and Musandam, N and S Batinah, Dhakhilya, S Sharqiya; causes: corneal opacities 36%, cataract:30% post segment 15%.
The economic performance of the sultanate is closely tied to the oil industry. Oman is a major energy exporter. The mineral industry includes the mining of chromites, the refining of copper with the silver and gold as byproducts. In 1997, gross domestic product (GDP) per capita was estimated to be US$9000.1 The GDP is defined as gross value of the goods and services produced inside the country minus raw materials and the other goods and services consumed during the process of production The agriculture sector contributes about 3% of the GDP and employs an estimated 9% of the labour force. The gross national product (GNP) per capita of Oman in 1997 was $7900. The GNP is defined as GDP plus net factor income. During the same period, the GNP of the United Kingdom and the United States was $20 870 and $29 080 respectively. The neighbouring countries of Saudi Arabia, the United Arab Emirates (UAE), and Yemen had GNPs of $7150, $17 400, and $270 respectively in 1997.2
The last general census of the population was undertaken in December 1993. On this basis, the population projection for 19963 suggested that there were 1 650 000 Omani people (male:female ratio 1.05:1). The age group under 15 years comprises 50% of the total population while 15.3% of the total were in the “0 years and above” age group. About half of the population lives in the capital city, Muscat, and in the Batinah coastal plain. About 140 000 Omanis live in the southern region of Dhofar and about 30 000 in the Musundam peninsula on the Strait of Hormuz. The sultanate is divided into 10 health regions.
In 1970s, blinding eye diseases particularly trachoma were highly prevalent. Trachoma was estimated to be 70%–80% among the Omani population of all ages in highly endemic areas of central and northern Oman, while the Dhofar region was comparatively free from the trachoma infection.4,5
In 1991, a World Health Organization review of the world's available data, estimated the prevalence of blindness in Oman at 2%. At that time, major causes of blindness were due to trachoma, other causes of corneal opacities, cataract, and glaucoma.6 Following this estimation, the national programme for the prevention of blindness was reorganised, expanded, and renamed as the “Eye Health Care Programme” (EHCP). Eye healthcare services were established at the three levels from primary health care to tertiary eye care centres. Standard operating procedures were laid down for all three levels of eye care.
In the absence of reliable population based data, a survey was conducted between October 1996 and February 1997 for evaluation and future planning. This study was limited to the Omani population. An Omani person is defined as an indigenous person and excludes the expatriate population.
The survey had following main objectives:
to estimate the prevalence of blindness in the Omani population
to estimate the distribution and causes of blindness.
SUBJECTS AND METHODS
A population based descriptive cross sectional design was used.
Sampling frame and study design
Projections for the year 1996, based on the 1993 national census, were used to construct a comprehensive sampling frame listing all the localities. Though the total population was 2 125 000 people, including the expatriates, the survey was limited to the Omani population of all ages. The target population was estimated to represent 1 650 000 people.
The random sampling and data collection procedures were adopted from the WHO Programme for the Prevention of Blindness.7–9 In view of the resource constraints (principally logistics), the design did not permit investigation of the prevalence and the causes of low vision. The study was limited to a descriptive approach of the epidemiology of blindness. Based on the reported distribution of eye diseases in the different regions of the sultanate, nine strata were defined: each health region being a stratum while Al Wousta and North Sharqiya were combined in a single stratum. The design ensured that the size of the sample taken from each stratum was proportional to the population size of the stratum. A two stage cluster sampling procedure was used to select 116 clusters with probability proportion to the size, each cluster comprising 12 households with an average of seven family members per household.10,11
To ensure representativeness of the study population, in each cluster, one household was selected at random to serve as the “starting point.” The Omanis living in the 12 adjacent houses were registered to be systematically examined.
Sample size
The sample size calculation8,11 was based on an estimated prevalence of 1.5% within an error bound of 20% with 95% confidence. With simple random sampling, the required sample size was calculated as 6267 people. This number was adjusted upwards to account partly for cluster sampling design effect (conservatively estimated at 1.8) and adjusted further to account for a possible 10% non-response rate. Accordingly, and taking into account the budgetary constraints, the final sample size was 12 400.
Field procedures
Prestudy activities included wide media coverage of the intended survey and its purposes. The survey was conducted in two phases.
In the first phase, the field work consisted of visiting all selected households within the clusters to enumerate all the residents, measuring visual acuity and performing eye examination of registered people.
The work was carried out by 33 teams. Each team consisted of one trained school health medical officer and one nurse with long experience of eye and vision screening. A comprehensive registration was carried out in each eligible household. A “usual” resident was defined as an Omani of any age having resided in the household for 6 months or more over the past year.
Presenting visual acuity measurement was assessed for each eye separately, using WHO tumbling “E” test card (illiterate Snellen optotype) or ability to count fingers. The procedure was carried out at 6 metre and 3 metre distances in outdoor light. Testing was carried out with glasses in those using them for distance viewing. In those who could not achieve the 3/60 level, testing was carried out using a pinhole. Visual acuity of infants, young children unable to be tested, or adults with comprehension problems was assessed by the ability to fix correctly and follow a moving hand held light.
Blindness was defined according to the WHO tenth revision of the International Classification of Diseases.12
All the participants were subjected to basic eye examination of the eyelids and the anterior segment of the globe. The pupillary reflex was checked and the lens status was assessed by the medical officer using a torch light and a magnifying (×2.5) binocular loupe.
In the second phase of the study, all people considered as blind by the field team after completion of the screening procedures, were transported to the regional eye hospital.
There, the referred people were systematically examined by the study ophthalmologists according to the standardised protocol. Visual acuity was reassessed for the confirmation and refraction was performed when necessary. The optic discs, the retinal vessels, and the posterior segment were examined by direct ophthalmoscopy after papillary dilatation. Intraocular pressure was measured in all people aged 40 and above (and anyone below this age when indicated), using an applanation tonometer. Field of vision was tested when applicable.
For each eye, all disorders which were responsible for, or contributed to, visual loss were assessed. A primary cause for the blindness was assigned for each eye. Furthermore, one principal disorder and one principal underlying cause of blindness were assessed for each individual. After considering the existing disorder in either eye, a principal cause responsible for blindness of the person was selected by the study ophthalmologist. In instances of comorbidity where two (or more) disorders were diagnosed, one being secondary to the other, the primary one was considered as the principal cause.
If the patient declined or did not present for this supplementary examination, the study ophthalmologists (equipped with a full set of instruments, including a portable slit lamp) visited her or his house in order to examine the eyes according to the standardised protocol.
Ethical considerations
Informed oral consent of the chief of the householder for the whole family was obtained during the house visit. Those with vision <3/60 due to cataract or those with entropion/trichiasis were offered free surgery. Medical treatment for minor eye ailments such as conjunctivitis and active trachoma was provided in the field. Those needing further specialised diagnosis or treatment were referred to the regional eye hospital.
Training
The field enumerators were oriented to the study objectives and trained over a week in techniques for mapping and registration. A detailed manual for operation was prepared and provided to each enumerator.
One week of the training was carried out for the medical officers and nurses involved in the first phase of the survey. The curriculum included instruction on the principle of the survey and practical training in assessment of visual acuity and eye examination in the field condition of the work.
Three days of task oriented training was conducted for the study ophthalmologists. This included review of the study objectives, clinical procedures along the line of the protocol, with emphasis on the rationale, content, and completion of the study examination form.
Practical exercises in completing the various study forms were carried out at each level of training. Data management staff was also trained.
Quality assurance procedures
In order to maximise the quality of the survey, in addition to training activities, various steps were taken: preparation and provision of a detailed study protocol and specific task oriented manuals of the operation (for each category of personnel involved), use of standard definitions and procedures, permanent supervision of the field teams till the end of the survey, including data analysis.
On completion of the training, a pilot study was carried out in six villages, outside those selected for the main study. It provided a field test of all study procedures, completion of the data forms, and patient logistics (referral and transportation to the regional hospital). It was also used to ensure that the training of the medical officers, nurses, and ophthalmologists was adequate. The assessment of interobserver and intraobserver variations for the clinical findings was ensured. The measurement of visual acuity by the nurses was compared with the results of ophthalmologists in 1287 people, one third presenting visual problems including blindness. The concordance rate was 99.1% (underscoring was 0.3% and overscoring was 0.6%). Each participating ophthalmologist was compared with the senior ophthalmologists to match diagnosis of cataract and trachoma as the principal cause of blindness. The concordance rate was again over 95%.
Data management and data analysis
Completed data collected on the “WHO eye examination forms” were edited at the end of each day by the medical officer in the field or by the participating ophthalmologist in the regional hospitals for accuracy and missing values. Then they were packed and sent to the data manager in the statistical department of the Ministry of Health at Muscat. Final editing and computerised data entry was performed using epi-info 6. Final data cleaning included value frequency analysis and range checks. The cleaned data set was transferred for the statistical analysis using spss/9.0 software.
Statistical considerations
Those included in the sample but not examined were considered “conservatively” to have “adequate vision” and were included in the studied population (denominator). For comparing the estimates of the nine regions, direct age/sex standardisation was used. The age/sex structure of the projected population of Oman in 1996 was used as the reference.
In calculating 95% confidence interval the cluster sampling design was taken into account and adjusted for.11
RESULTS
A total of 12 439 people were enumerated in the 116 randomly selected clusters, without the need of any replacement of “missing” cluster. Examination was conducted on 11 417 people; 903 of those enumerated were not available for the examination because of temporary absence from the area and another 119 declined to participate in the study. The overall response rate was 91.8%. Comparing the response rate for each age category (male and female together), it was found to range from 81.4% in 40–59 years age category to 98.4% in 0–14 years age group. However, if the differential response rate in term of sex is considered, the response rate among males aged 15–59 is significantly lower (69.5%) (Table 1).
Table 1.
Response rate by sex and age (OES 1997)
| Females | Males | Total | |||||||
| Age | Enumeration | Examination | % | Enumeration | Examination | % | Enumeration | Examination | % |
| 0–14 | 3054 | 3020 | 98.9 | 3230 | 3188 | 98.7 | 6284 | 6208 | 98.8 |
| 15–39 | 2292 | 2190 | 95.5 | 2048 | 1491 | 72.8 | 4340 | 3680 | 84.8 |
| 40–59 | 582 | 55 | 94.8 | 662 | 460 | 69.5 | 1244 | 1012 | 81.4 |
| 60+ | 267 | 251 | 94 | 304 | 265 | 87.2 | 571 | 516 | 90.4 |
| Total | 6195 | 6013 | 97.1 | 6244 | 5404 | 86.6 | 12439 | 11417 | 91.8 |
The age and sex distribution of those enumerated and included in the study corresponded fairly well to the population of Oman. However, the age and sex distribution of those examined is significantly different from the population of the sultanate (goodness of fit for males: p = 0.000001; goodness of fit for females: p = 0.002). The demographic analysis reveals a distortion in relation to the male population of the reference. The 15–39 age group is under-represented in the sample and in comparison, the sample suffered an over-representation of the younger age group (Table 2).
Table 2.
Comparison (in %) of the Omani population and the examined study population (OES 1997)
| Male | Female | |||
| Omani population* | Examined population | Age | Omani population* | Examined population |
| 48.6 | 58.9 | 0 to 14 | 48.5 | 50.3 |
| 36.2 | 27.6 | 15 to 39 | 36.2 | 36.4 |
| 10.5 | 8.5 | 40 to 59 | 10.8 | 9.2 |
| 4.7 | 4.9 | 60 and + | 4.4 | 4.1 |
*National census projection for the year 1996.
Of 420 patients requiring a supplementary examination, 346 (82.4%) were examined in the regional hospital, 66 (15.7%) were examined at their home, eight (1.9%) were dropouts. Among the 138 “presumed blind” cases referred for a supplementary examination at the regional eye hospital, four people dropped out.
The primary parameter used in the study was the assessment of visual acuity (VA). VA was unable to be assessed in nearly 2105 (18%) of the study individuals, primarily in young children; 9056 (79.3%) people were assessed without glasses and 346 (3%) were assessed with their distance vision glasses.
The prevalence of blindness at the national level was 1.1% (95% CI: 0.9 to 1.3) amounting to 17 000 blind people in the Omani population. Table 3 shows that the prevalence of blindness clearly related to the increasing age: blindness in childhood (0–14 years of age) is grossly estimated to be 8/10 000. At the other end of the age spectrum, the prevalence was estimated at 1680/10 000 (16.8%).
Table 3.
Prevalence of blindness by age, sex, and regions (OES 1997)
| Prevalence (%) | 95% CI | |
| Age (years) | ||
| 0 to 14 | 0.08 | 001 to 0.14 |
| 15 to 39 | 0.1 | 0.00 to 0.2 |
| 40 to 59 | 2.3 | 1.5 to 3.2 |
| 60 and + | 16.8 | 13.3 to 20.4 |
| Sex | ||
| Male | 0.8 | 0.5 to 1 |
| Female | 1.4 | 1.0 to 1.7 |
| Health region | ||
| Muscat | 0.4 | 0.1 to 0.8 |
| Dhofar | 0.4 | 0.1 to 0.8 |
| Dhakhilya | 1.5 | 1.0 to 2.3 |
| North Sharqiya | 0.4 | 0.0 to 1.0 |
| South Sharqiya | 1.0 | 0.3 to 1.7 |
| North Batinah | 1.3 | 0.8 to 1.9 |
| South Batinah | 1.5 | 1.0 to 2.0 |
| Dhahira | 1.3 | 0.7 to 1.9 |
| Musandam | 3.0 | 2.6 to 3.4 |
| Overall prevalence | 1.1 | 0.9 to 1.3 |
After adjusting the age differences between male and female in the examined population (females were younger, which is consistent with the census data) the higher prevalence in females (1.4%) compared to males (0.8%) was statistically significant (χ2 = 6.19, p=0.012; OR =0.64 (95% CI: 0.44 to 0.92)).
Regional prevalence varied from 0.4% in the capital region of Muscat to 3% in Musandam in the extreme north of the country (Table 3 and Fig 1).
Table 4 sets out the causes of blindness by sex. It is observed that anterior segment causes accounted for 31.6% of all causes of blindness, while lens related blindness accounted for 31.3% and posterior segment for 27.8%. A further 9.5% was the result of disorganised/absent globes. In all categories of blindness (except in the case of disorganised/absent globe), females predominate.
Table 4.
Causes of blindness by sex (OES 1997)
| Causes | Male | Female | Frequency | % |
| Anterior segment causes | 11 | 33 | 44 | 31.6 |
| Trachomatous corneal opacities | 8 | 25 | 33 | 23.7 |
| Non-trachomatous corneal opacities | 3 | 8 | 11 | 7.9 |
| Causes related to lens | 17 | 25 | 42 | 31.3 |
| Unoperated cataract | 17 | 24 | 41 | 30.5 |
| Uncorrected aphakia | 0 | 1 | 1 | 0.8 |
| Posterior segment causes | 13 | 22 | 35 | 27.8 |
| Glaucoma | 5 | 11 | 16 | 11.5 |
| Optic atrophy | 6 | 1 | 7 | 5.0 |
| Macular degeneration | 1 | 3 | 4 | 2.9 |
| Retinal detachment | 0 | 2 | 2 | 1.5 |
| Congenital anomalies | 0 | 2 | 2 | 1.5 |
| Vascular retinopathies | 1 | 0 | 1 | 0.8 |
| Refractive error | 0 | 2 | 2 | 1.5 |
| Uveitis | 0 | 1 | 1 | 0.8 |
| Disorganised/absent globe | 6 | 7 | 13 | 9.5 |
| All causes | 49 | 85 | 134 | 100 |
In the group of regions Muscat, Dhofar, and North Sharqiya, having a blindness rate of 0.5%, the causes of blindness such as cataract, glaucoma, and diseases of the posterior segment constituted 30%, 25%, and 20% of the total respectively. In contrast, in the group of regions Dhahira and Musundam, North and South Batinah, Dhakhilya, South Sharqiya, having blindness rate >0.5%, the causes of blindness such as trachomatous and non-trachomatous corneal opacity, cataract and posterior segment diseases constituted 36%, 31%, and 15% of the total, respectively.
DISCUSSION
The results of this survey provide the first population based data on the prevalence and causes of blindness in Oman.
A high response rate among the eligible people was achieved (91.8%). The representativeness of the enumerated sample was acceptable. However, owing to high absenteeism of males in the working age group, the representativeness of the examined population was not as close as expected. In order to compensate this deficit, age/sex standardised estimates were calculated.
The survey revealed that 1.1 % of the population was blind. Four people among the presumed blind dropped out. No information was available to document these cases, so they have been considered as “lost to follow up.” If it is considered that the four presumed blind people were in fact blind, the reported prevalence of blindness would have been underestimated to the extent of 0.15%.
The prevalence of blindness was nearly double among females (1.4%) than males (0.8%). This may indicate a greater propensity for the blindness in women perhaps due to trachoma and lower uptake of cataract surgical services. This definitively requires further operational research studies.
This study confirmed that blindness increases dramatically with age: 93% of the blind were in age of 40 years and older. Unoperated cataract, which is age related, accounted for 30.5% of all blindness. Other age related causes of blindness included glaucoma (11.5%), age related macular degeneration (ARMD) (2.9%), and diabetic retinopathy (0.8%). In Oman, infant and childhood mortality rates are decreasing steadily and people are living longer. Demographic trends indicate that elderly population (60 years and above) will double by the year 2020. As a result of this demographic/epidemiological transition, the burden of blinding diseases will increase. This should be considered in the planning of future eye care services, to address unmet needs and increased demand.
Given the size of the sample chosen for the study, the prevalence of blindness in children could not be reliably estimated. However, the study gave an estimated figure of 8/10 000 population. This compares with the estimates from 2 to 4/10 000 and from 10/10 000 in industrialised and developing countries respectively.13 Although not a major problem in terms of absolute number, childhood blindness accounts for a significant number of years with blindness. In planning, to deal with the causes of blindness in the children in future, services have to be strengthened at all levels. For conditions requiring surgical treatment such as congenital cataract and glaucoma, specialised centres would need to be developed at the tertiary level. This should also include services for refractive and low vision care.
As selection of clusters was proportional to the size of the strata and communities, some regions contributed few clusters in the national sampling frame and the final sample. This would limit the valid comparison between regions. However, to provide a basis for such a comparison age/sex standardised prevalence were calculated. Marked regional variation was observed in the prevalence of blindness among regions (Fig 1) ranging from 0.4% in Muscat to 1.7% in Dhakhilya to an extreme of 3% in Musandam. From an epidemiological point of view, it may be stated that Oman presents two zones in relation to blindness prevalence—one zone comprising Dhofar and Muscat regions (in fact the prevalence of blindness in this zone compares favourably with the reported prevalence in industrialised countries),13 the second zone comprises the rest of the country. In this study, Dhakhilya, North Batinah, and South Batinah accounted for more than 60% of the total blindness in Oman. This regional variation could be the result not only of ecological but also socioeconomic differences.
The blindness rates in 1976, 1981, 1990, and 1996 were reported to be 2.4%–5.6%, 2%–6%, 2%, and 1.1% respectively. The GDPs in the same year were $2285, $6820, $11 584, and $9000 respectively. It seems that with the rise of national GDP per capita, the blindness rate declined. Since information on GDP is available at national level only, the GDP of groups of region with high and low blindness rate could not be compared.
While analysing the survey results, causes of blindness were classified both in terms of structure of the eyeball (anatomy) and diseases (aetiology). Causes related to the anterior segment of the eye accounted for 31.6%. This included corneal opacities from different origins such as trachoma (23.7%) and corneal infections (7.9%), both largely preventable at the primary healthcare level. In addition, there was 9.5% with total disorganisation of the eyeball. This was also likely to be the result of corneal infection or trauma. Unoperated cataract accounted for 30.5% of all causes of blindness. The prevalence of blinding cataract correlates with the uptake of services available. To increase uptake among populations where this is low, active outreach through community based primary eye care services need to be pursued. Blinding disorders of the posterior segment of the eyeball (27.8%), do not usually respond to the prevention and control measures. Given the trends towards and increase in the future incidence of these conditions, subspecialty eye care (to deal with conditions like diabetic retinopathy and causes of low vision) needs to be developed and strengthened in selected centres.
In summary, about 17 000 people were blind in Oman at the time of survey. Of these, 75% were the result of conditions that could have been prevented or could be treated. Unfortunately, this study does not provide any data on low vision. The limitation of the study because of resource constraints precluded an estimation of the prevalence of low vision. However, based on the WHO Data Bank,13,14 it could be estimated that low vision exists in Oman at a magnitude of 2.5–3 times that of blindness, giving an estimated total of 42 500–51 000 people with low vision.
Earlier estimates of blindness were based on the investigations in limited areas of the sultanate. In 1988, the extrapolation of the data of existing limited studies estimated that blindness prevalence could be 2%. Between 1991 and the time of this survey, significant resources had been provided for the prevention of blindness in Oman, including strengthening, expansion and reorganisation of the national eye care system from the community level to the secondary and tertiary levels. Additionally, the overall socioeconomic situation of the Omani national has improved significantly.
The global prevalence of blindness is estimated to be 0.7%, ranging from 0.3% and 0.5% in the industrialised countries. In the developing countries, it is estimated to be more than 1.5%.13,14 The Middle Eastern crescent (as defined by the 1993 World Bank Report) presents an overall prevalence of 0.7%. Surveys conducted in the eastern15 and in the south western provinces16 of Saudi Arabia reported prevalence of blindness to be 1.5% and 0.7% respectively. The major causes of blindness were cataract, refractive errors, trachoma, glaucoma, post-surgical complications, corneal scarring, and trauma. In the Republic of Yemen, a limited survey in 198914 estimated the prevalence of blindness to be 0.7%. The main causes of blindness were cataract, glaucoma, trachoma and other causes of a disorganised globe. A population survey was conducted in Lebanon in 199617 and 10 418 people were examined. The prevalence of blindness was estimated to be 0.6% and that of low vision at 3.9%. The major cause of blindness was cataract (41.3%).
In this context, as discussed earlier, Oman presents two distinct epidemiological patterns: areas with prevalence comparable to the industrialised countries and some regions which still present the patterns seen in developing countries.
The trends of the causes for blindness in regions with lower rates of blindness showed fewer communicable diseases and more non-communicable diseases responsible for blindness. In the regions with a high prevalence of blindness, causes of trachomatous and non-trachomatous corneal opacity constituted the major proportion of total blindness.
The results of this survey provide a firm basis for the future planning and strengthening of comprehensive eye care services in Oman. It could also provide baseline information for use in future evaluations of the implementation of such programmes.
Acknowledgments
This work was supported by the World Health Organization, through the Eastern Mediterranean Region Office and its Programme of Prevention of Blindness and Deafness, Geneva.
The authors wish to thank the personnel of the following services of the Ministry of Health of the Sultanate of Oman: Eye Health Care Programme, Directorate General of Health Affairs, Department of School Health, Directorate General of Health Affairs, Regional Directorates of Health Services, Department of Health Research, Directorate of Health Planning.
The authors wish to acknowledge with thanks the assistance provided by Dr R Pararajasegaram in the editing of this paper, by Dr A Alwan for his support, and by Dr S P Mariotti in the preparation of the map.
REFERENCES
- 1.National Accounts Bulletin, Ministry of National Economy Director General of Economics Statistics, Sultanate of Oman, II issue. Oriental printers, 2000:13–26.
- 2.Basic Information, Nation to Nation www:\United Nation.
- 3.Ministry of Health of the Sultanate of Oman. Annual statistical report for 1996: demographic profile. Muscat, Oman, 1997:3–10.
- 4.Dawood WHO unpublished document. Assessment of prevention of blindness programme in Oman. EM/PBL/11, 1980:4–5.
- 5.Ministry of Health of the Sultanate of Oman. Annual statistical report for 1991: data on eye health. Muscat, Oman, 1992:47.
- 6.Thylefors B. WHO unpublished document. Report on prevention of blindness programme in Oman, 1991.
- 7.Thylefors B. A simplified methodology for the assessment of blindness and its main causes. World Health Statistic Quarterly 1987;40:129–41. [PubMed] [Google Scholar]
- 8.World Health Organization. Methods of assessment of avoidable blindness 1980. Offset publication No 54. Geneva: WHO, 1980 .
- 9.World Health Organization. Programme for the prevention of blindness: eye examination record, version iii. Unpublished document. Geneva: WHO, 1988: WHO/PBL/88.1
- 10.Cochrane WG. Sampling techniques. 3rd ed. New York: J Wiley, 1984.
- 11.Bennett S, Woods T, Liyanage WM, et al. A simplified method for cluster sample surveys of health in developing countries. World Health Statistics Quarterly 1991;44:98–106. [PubMed] [Google Scholar]
- 12.World Health Organization. International statistical classification of diseases and related health problems, tenth revision (ICD 10). Vol 1. Geneva: WHO, 1992.
- 13.Thylefors B, Negrel A-D, Pararajasegaram R, et al. Global data on blindness. Bull World Health Organ 1995;73:115–21. [PMC free article] [PubMed] [Google Scholar]
- 14.Thylefors B, Negrel A-D, Pararajasegaram R, et al. Available data on blindness (update 1994). Ophthalmic Epidemiol 1995;2:5–39. [DOI] [PubMed] [Google Scholar]
- 15.Tabara KF, Ross-Degnan D. Blindness in Saudi Arabia. JAMA 1986;255:337–84. [PubMed] [Google Scholar]
- 16.Al Faran MF, Al-Rajhi AA, Al-Omanr OM, et al. Prevalence and causes of visual impairment and blindness in the south western region of Saudi Arabia. Int Ophthalmol 1993;17:161–5. [DOI] [PubMed] [Google Scholar]
- 17.Mansour AM, Kassak K, Chaya M, et al. National survey of blindness and low vision in Lebanon. Br J Ophthalmol 1987;81:905–7. [DOI] [PMC free article] [PubMed] [Google Scholar]