Abstract
Aims: To determine the incidence of increased iris pigmentation in eyes treated with chronic latanoprost. This is an observational, cohort study.
Methods: The anterior segments of both eyes of 43 patients with glaucoma were photographed after unilateral latanoprost therapy. Two independent, masked observers analysed the slides of both eyes of the study participants, and compared the iris pigmentation of both eyes of each patient using a stereo viewer.
Results: 30 patients (69.7%) had a definite acquired iridial anisochromia; 15 patients (50%) had increased superficial iris pigmentation with a “granular” appearance (type 1 change), and 15 patients (50%) had an increased “stromal pigmentation”—that is, the affected iris appeared darker than the fellow eye, but without a “granular” appearance (type 2 change).
Conclusion: The incidence of increased iris pigmentation induced by latanoprost is much higher than previously reported. The high prevalence of mixed iris colour found in this population and the fact that the patients studied were undergoing unilateral therapy may explain these results.
Keywords: iris colour, latanoprost
Darkening of the iris colour is a well known side effect of both naturally occurring prostaglandins and prostaglandin analogues, such as isopropyl unoprostone1 and latanoprost.2–4
The reported incidence of increased iridial pigmentation after long term therapy with latanoprost varies from 10.8% in a Scandinavian study2 to 22.9% in a UK study.3 The higher figure in the latter study may be explained by the higher number of patients with green-brown or grey/blue-brown eyes in that country. Mixed colour irides, compared with irides of other colours, are believed to have the greatest chances of darkening during latanoprost therapy.4
Nevertheless, the exact incidence of increased iris pigmentation in latanoprost treated eyes is difficult to determine, because variations in either illumination or film processing occur frequently; therefore, the ability of consecutive photographs to record subtle changes in iris colour is probably not high.5
The chances increase of detecting a change in iris colour when unilateral latanoprost is administered. In these cases, the untreated eye serves as a control, provided the irides have similar pigmentation at base line. In addition, cases of unilateral latanoprost therapy allow simultaneous photography of both irides, which provides the best scenario to detect subtle changes in iris colour. For instance, both the trichomegaly induced by latanoprost6 and the increase in iris pigmentation induced by unoprostone were first described in patients undergoing unilateral treatment.
We studied the incidence of latanoprost related increases in iridial pigmentation in patients undergoing unilateral treatment with this prostaglandin analogue.
PATIENTS AND METHODS
We studied 45 consecutive patients with uncontrolled asymmetric or unilateral glaucoma who were candidates for unilateral therapy with latanoprost. The reason for unilateral therapy with latanoprost was either the absence of response or ocular intolerance to other drugs.
This was a prospective, observational, cohort study. We obtained informed consent from all patients after the procedure was fully explained, and only those patients willing to participate in the study were accepted. No institutional review board approval was required for this study.
To be included in the study, all patients had to meet the following inclusion criteria: unilateral or asymmetric glaucoma, needing latanoprost therapy in only one eye, absence of any degree of iris heterochromia or iris atrophy on detailed slit lamp examination, normal corneas bilaterally, intraocular pressure (IOP) readings lower than 35 mm Hg in both eyes, and no history of intraocular surgery in the previous 6 months.
Patients with a history of previous therapy with any prostaglandin analogue, anterior uveitis, or hyphaema were excluded from the study.
Only patients with a minimum of 12 month follow up were included in the final analysis. Latanoprost therapy was withdrawn in two patients because of an inadequate IOP control. This happened at the 6 month visit in both cases, so both patients were excluded.
Forty three patients satisfied all the inclusion criteria. Patients were examined 1 month after the start of latanoprost therapy, and then every 3 months.
Photographs of the anterior segments of both eyes were taken at baseline and in every follow up visit. Baseline slides were reviewed by two independent observers, as soon as the film was processed, to check that there were no degree of iris heterochromia or iris atrophy present.
Twenty one healthy volunteers served as controls, and their anterior segments were also photographed.
All photographs were taken by the same ophthalmologist, in exactly the same fashion, using the same Nikon photographic slit lamp (Nikon FS-2), equipped with a Nikon FE reflex camera (Nikon Corporation, Tokyo, Japan). We used Kodak Elitechrome 100 ASA colour slide film (Eastman Kodak Company, Rochester, NY, USA) in all cases. The flash setting was in position 1, the background illumination was turned off, and the slit was completely open. The illumination arm of the slit lamp was angled approximately 30 degrees to the left, while the observation arm remained in the straight position. All photographs were magnified ×16.
The right eye of each patient and volunteer was photographed first and then the left eye, so that any conditions that might have altered the recording of the iris colour, such as the ambient light or the patient’s clothes, were kept exactly the same.
The film was then processed by an authorised Kodak E6 processing laboratory, to ensure that a pair of high quality slides was obtained for each patient.
At the end of the study, two independent, masked observers simultaneously examined the pair of slides of each patient, using a stereo viewer (Stereo viewer model 020, Deep-Vue Corporation, Grove, OK, USA). The pair of slides taken at baseline, and at the 12 month visit were chosen for the “reviewing process.”
The observers were instructed to close each eye alternately, so both slides of each patient could be easily compared. The observers reviewed the slides of all the study patients during the same session.
The observers first reviewed the patients’ baseline slides and the slides of the volunteers, in a masked fashion, and classified the colour of both eyes of the patients and of the volunteers as one of eight shades: homogeneous blue-grey, green, brown, blue-grey/brown, blue-grey/with zones of brown, yellow-brown, green-brown, or green with zones of brown.
If a discrepancy was noted between the two observers regarding the basal iris colour classification of the eyes, the disputed slides were reviewed again by the same observers and a consensus was reached.
The observers then determined if there was significant heterochromia between the eyes of each patient (or volunteer), reviewing the 12 month visit slides, and graded it according to the following scale: no iridial anisochromia, or a mild, moderate, or marked (severe) degree of iridial anisochromia. The slides taken to the healthy volunteers were also included for the reviewing process, in a masked fashion, so the readers did not know whether the pair of slides they were reading belonged to a patient with unilateral therapy with latanoprost or to a healthy volunteer, although they knew that each pair of slides were the right and the left eye of the same person. In addition, the observers described the morphology of the pigment distribution on the iris surface—that is, iris darkening with no change in the morphology of the pigment distribution compared with the other eye, or iris darkening with a definite change in the pattern of the pigment distribution on the iris surface, compared with the other eye. If the latter condition was chosen, the observer then described the pattern of the pigment distribution on the iris surface. The results were then tabulated.
Data are expressed as the mean (SD), occasionally followed by the range (minimum-maximum values). Mann Whitney’s U, χ2, and kappa tests were used, when appropriate, for comparisons between groups, and to check the interobserver agreement.
The statistical analysis was done with the Statview SE+Graphics (Abacus Concepts Inc, Berkeley, CA) program, using a Macintosh PowerBook 1400cs/117 (Apple Computer Inc, Cupertino, CA, USA) personal computer.
RESULTS
The patient demographics were as follows. The mean age of the study patients was 68 (18.6) years (range 28–90 years). There were 24 females and 19 males in the study group. Race was white in all cases.
The distribution of the basal eye colours of the study is shown in Table 1.
Table 1 .
Distribution of the iris colour of the study patients (43 cases), and the volunteers (21 cases)
| Study eyes | Volunteers | |
|---|---|---|
| Blue-grey | 4 (9.3%) | 2 (9.52%) |
| Blue-grey/zones of brown | 6 (13.95%) | 4 (19.05%) |
| Blue-grey/brown | 4 (9.3%) | 0 |
| Green | 0 | 0 |
| Green-zones of brown | 0 | 0 |
| Green-brown | 0 | 0 |
| Brown | 1 (2.33%) | 6 (28.57%) |
| Yellow-brown | 28 (65.12%) | 9 (42.86%) |
Observer 1 identified 33 cases (76.7%) of definite acquired iridial anisochromia in the study population of 43 patients, and observer 2 identified 32 cases (74.4%). Both observers agreed that there was definite iridial anisochromia in 30 patients (69.8%) (kappa = 0.685). Observer 1 rated the degree of iridial anisochromia as mild in 10 cases, moderate in 14, and marked in nine cases, and observer 2 rated the iridial anisochromia mild in 14 cases, moderate in 10, and marked in eight cases (kappa = 0.597) (Table 2).
Table 2 .
Proportion of patients showing an acquired darkening of the iris colour, and degree of the anisochromia found
| Observer 1 | Observer 2 | |
|---|---|---|
| Patients showing iris heterochromia | 33 (76.7%) | 32 (74.4%) |
| Patients with mild heterochromia | 10 (23.3%) | 14 (32.5%) |
| Patients with moderate heterochromia | 14 (32.5%) | 10 (23.3%) |
| Patients with marked heterochromia | 9 (20.9%) | 8 (18.6%) |
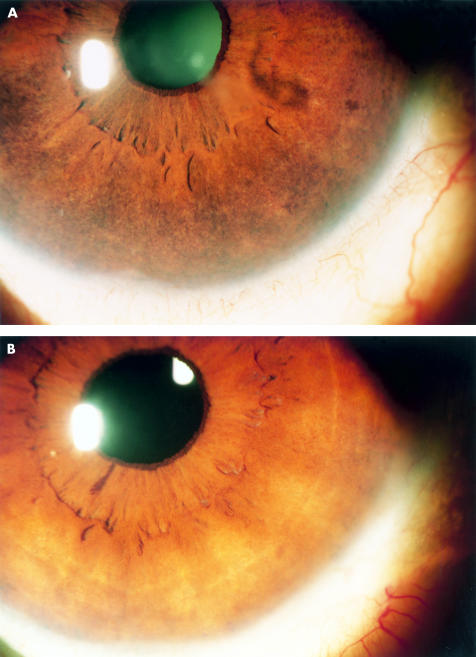
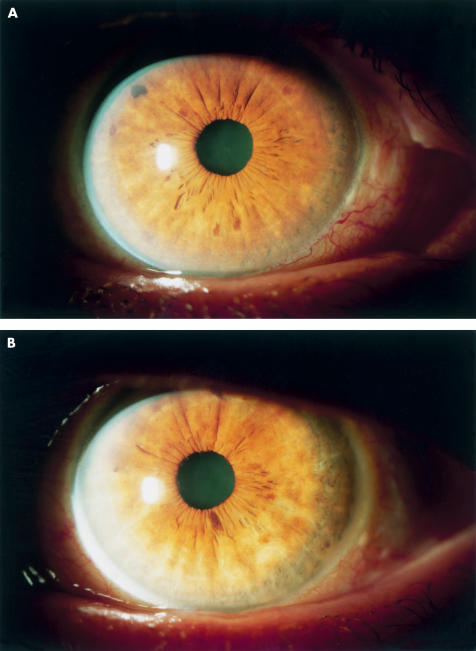
Regarding the morphological description of the iris pigmentation in the darker eye of the patients with acquired iris heterochromia, both observers agreed that 15 patients (50%) had an increase in the superficial pigmentation of the iris with a “granular” appearance (type 1 change). This type of pigmentary change was more evident in the iris periphery than in the pupillary zone in all cases (Fig 1). The observers also agreed that 15 patients (50%) had an increase in the stromal pigmentation, meaning that the affected iris appeared darker than the other eye, although there were no apparent “superficial” changes in the iris pigmentation (type 2 change) (Fig 2).
Figure 1 .
Anterior segment photography of a patient under unilateral treatment with latanoprost. (A) The right (treated) eye, and (B) the untreated left eye. Note the peripheral hyperpigmentation of the treated eye, with a granular appearance (type 1 change).
Figure 2 .
Anterior segment photography of a patient under unilateral treatment with latanoprost. (A) The right (treated) eye, and (B) the untreated left eye. Note that the colour of the treated eye is darker than the fellow eye, but there are no superficial changes in the iris pigmentation (type 2 change).
Both observers found no case of definite iridial anisochromia in the slides of the healthy volunteers.
DISCUSSION
The incidence of increased iridial pigmentation resulting from latanoprost therapy that we found in our population is higher than previously reported. The UK multicentre latanoprost study3 reported that 47 of 205 patients had darkening of the iris colour after 1 year of latanoprost treatment (overall incidence 22.9%). Other studies found a lower incidence of this complication,2,5,7 which seems to occur more frequently in mixed colour irides than in homogeneous ones.4
One possible explanation for this apparent discrepancy is that the prevalence of the different eye colours in our Mediterranean population differs from those found in other studies. For example, in the UK study3 up to 54% of the treated patients had mixed green-brown or blue/grey-brown irides. In our study, up to 38 patients (88.3%) had mixed colour irides, most of which were yellow-brown. It is well known that green-brown and yellow-brown irides have the greatest propensity to develop increased iris pigmentation in response to latanoprost therapy.4
Another explanation is that in a study of patients undergoing unilateral treatment with latanoprost the chances of detecting even slight degrees of acquired iridial anisochromia are increased, compared with when serial photographs are taken during the follow up of patients undergoing bilateral therapy. When the latter method is used, mild degrees of change in iris colour might remain unnoticed.
Nevertheless, it seems clear from our results that significant darkening of the iris should be expected to occur in a high number of patients treated with latanoprost, at least in a Mediterranean population.
To the best of our knowledge, it is not known why some irides develop a change in their pigmentation in response to latanoprost therapy, while others, even of the same basal iris colour, do not.
This increase in the pigment content of the iris seems to be well tolerated by the eye, and no sign of dispersion of pigment into the anterior chamber angle has yet been described. However, patients of Mediterranean descent should be informed that the chances are high of developing this change in the iris colour.
It is noteworthy that only two of the study patients noticed the darkening of the iris colour, even though it occurred unilaterally. This may indicate that high magnification slides are more sensitive than “naked eye” observation for detecting changes in iris colour and that the change in colour is not important cosmetically.
Some investigators have speculated that prostaglandins may actually restore the natural colour of the iris, because the darkening occurs, in their opinion, more often in the peripheral, lighter part of the mixed colour irides, thus producing a more uniform iris colour.7 According to our data, this is not the case, because the increase in pigmentation in the type 1 change was so marked that the iris colour became much darker in the periphery than in the pupillary zone of the iris. In addition, the granular appearance of the surface of the peripheral iris resulting from the development of multiple, tiny, heavily pigmented dots was not seen in the pupillary zone of the same iris. Therefore, at least type 1 increase in iris pigmentation does not produce a uniform iris colour.
Wistrand et al4 originally described that the increase in iris pigmentation could be either “concentric”—that is, spreading from the brown or yellow-brown pupillary zone into the peripheral iris, or a “more diffuse spread of pigment.”
We found two distinct patterns of increased iris pigmentation: the superficial (type 1 change) and the stromal (type 2 change).
In type 1 change, the increase in iris pigmentation is much more pronounced in the periphery of the affected iris that in the pupillary zone. On the other hand, in type 2 change, the degree of iris darkening seems to be the same in all areas of the iris. We did not find any case of the “concentric” pattern of increase in iris pigmentation, “spreading” from the pupillary zone described by Wistrand et al.4
We can only speculate about the origin of the granular appearance of the iris surface, found in the type 1 colour change.
Mastropasqua et al8 suggested that the latanoprost induced increase in the pigmentation of the peripheral iris could be related to “trapping of dispersed pigment in the anterior uvea.” If this hypothesis is true, it would explain the granular appearance in some of our patients. Nevertheless, the histological analysis of a human iris that had a latanoprost induced change in colour did not show any extracellular pigment in the iris stroma. 9
On the other hand, it is interesting that tiny irregularities are frequently observed in the pigment distribution on the iris surface in mixed colour irides, as if some superficial melanocytes are darker than the surrounding superficial cells (Fig 3). Considering this, the superficial change may represent simply an increased number of and a darkening of the colour of the superficial pigment irregularities normally present in the periphery of mixed colour irides.
Figure 3 .
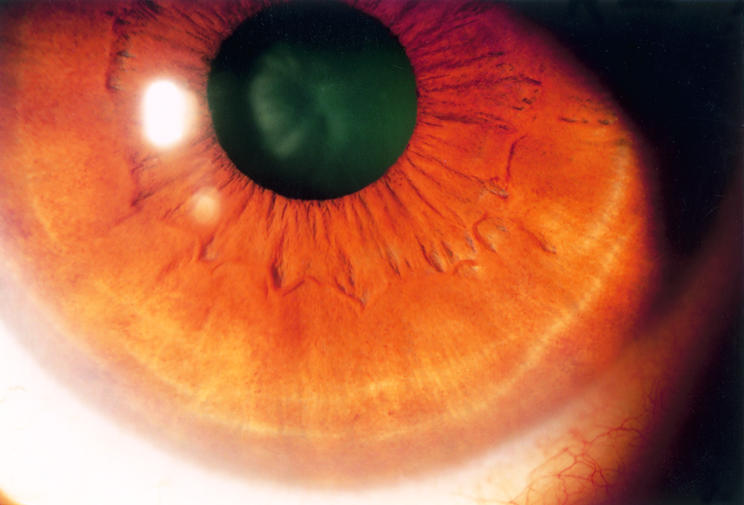
Anterior segment photography of a control eye with a mixed “yellow-brown” colour. Note the tiny “pigmented” irregularities present on the surface of the peripheral iris.
Recently, Lindquist and coworkers10 showed that active melanin synthesis occurs in adult monkey irides, but in only a small number of melanocytes. Those authors also found that latanoprost seems to increase the number of melanocytes synthesising melanin and the melanin content of these cells. Stromal melanocytes mainly aggregate in the anterior border layer of the iris, and because they are oriented parallel to the surface,11 are therefore the first to influence the iris colour when observed from outside. Furthermore, Imesch et al12 suggested that the iris colour seems to be associated with the number and area of melanin granules within superficial iris stromal melanocytes.
All these facts could explain the change in the superficial pattern of pigment distribution in some of our latanoprost treated patients. The change could represent the latanoprost related activation of melanogenesis in some superficial melanocytes, which increase their melanin content and thus become darker, resembling pigmented dots.
Although the study eyes seemed to tolerate the darkening of the iris induced by latanoprost, it is clear that more studies are needed to increase our knowledge about this peculiar side effect of topically applied prostaglandin analogues.
Rapid responses
Letters on the following British Journal of Ophthalmology papers have been published recently as rapid responses on the BJO website. To read these letters visit www.bjophthalmol.com and click on “Read eLetters”
A randomised controlled trial of written information: the effect on parental non-concordance with occlusion therapy. D Newsham. Br J Ophthalmol 2002;86: 787–91.12084751
Surgery for glaucoma in the 21st century. P T Khaw, A P Wells, K S Lim. Br J Ophthalmol 2002;86:710–11.12084733
Viability of Acanthamoeba after exposure to a multipurpose disinfecting contact lens solution and two hydrogen peroxide systems. K Hiti, J Walochnik, E M Haller-Schober, C Faschinger, H Aspöck. Br J Ophthalmol 2002;86:144–6.11815336
Argon laser and trichiasis: a helpful tip. J Sahni, D Clark. Br J Ophthalmol 2001;85:761.
If you would like to post an electronic response to these or any other articles published in the journal, please go to the website, access the article in which you are interested, and click on “eLetters: Submit a response to this article” in the box in the top right hand corner.
The authors have no proprietary interest in any aspect of this study.
REFERENCES
- 1.Yamamoto T, Kitazawa Y. Iris-color change developed after topical isopropyl unoprostone treatment. J Glaucoma 1997;6:430–2. [PubMed] [Google Scholar]
- 2.Alm A, Stjernschantz J. Effects on intraocular pressure and side effects of 0.005% latanoprost applied once daily, evening or morning. A comparison with timolol. Ophthalmology 1995;102:1743–52. [DOI] [PubMed] [Google Scholar]
- 3.Watson P, Stjernschantz J. The Latanoprost study group. A six month, randomized, double masked study comparing latanoprost with timolol in open-angle glaucoma and ocular hypertension. Ophthalmology 1996;103:126–37. [DOI] [PubMed] [Google Scholar]
- 4.Wistrand PJ, Stjernschantz J, Olsson K. The incidence and time-course of latanoprost-induced iridial pigmentation as a function of eye color. Surv Ophthalmol 1997;41 (Suppl 2):S129–38. [DOI] [PubMed] [Google Scholar]
- 5.Camras CB, Alm A, Watson P, et al. The latanoprost study group. Latanoprost, a prostaglandin analog, for glaucoma therapy. Efficacy and safety after 1 year of treatment in 198 patients. Ophthalmology 1996;103:1916–24. [DOI] [PubMed] [Google Scholar]
- 6.Johnstone MA. Hypertrichosis and increased pigmentation of eyelashes and adjacent hair in the region of the ipsilateral eyelids of patients treated with unilateral topical latanoprost. Am J Ophthalmol 1997;124:544–7. [DOI] [PubMed] [Google Scholar]
- 7.Camras CB. The United States latanoprost study group. Comparison of latanoprost and timolol in patients with ocular hypertension and glaucoma. A six-month, masked, multicenter trial in the United States. Ophthalmology 1996;103:138–47. [DOI] [PubMed] [Google Scholar]
- 8.Mastropasqua L, Carpineto P, Ciancaglini M, et al. A 12-month, randomized, double-masked study comparing latanoprost with timolol in pigmentary glaucoma. Ophthalmology 1999;106:550–5. [DOI] [PubMed] [Google Scholar]
- 9.Grierson I, Lee WR, Albert DM. The fine structure of an iridectomy specimen from a patient with latanoprost-induced eye color change. Arch Ophthalmol 1999;117:394–6. [DOI] [PubMed] [Google Scholar]
- 10.Lindquist NG, Larsson BS, Stjernschantz J. Increased pigmentation of irideal melanocytes in primates induced by a prostaglandin analogue. Exp Eye Res 1999;69:431–6 [DOI] [PubMed] [Google Scholar]
- 11.Dietrich CE. Zur feinstruktur der Melanocyten der menschlichen Iris. Graefes Arch Klin Exp Ophthalmol 1972;183:317–33. [DOI] [PubMed] [Google Scholar]
- 12.Imesch PD, Bindley CD, Khademian Z, et al. Melanocytes and iris color. Electron microscopic findings. Arch Ophthalmol 1996;114:443–7. [DOI] [PubMed] [Google Scholar]