Trabeculectomy remains the standard surgical glaucoma procedure against which other procedures are measured. The incidence of failure of trabeculectomy in higher risk cases can be reduced with the use of the adjuvant antiproliferative agents 5-fluorouracil and mitomycin C.1,2 The standard method of delivery of these adjuvant agents to the surgical site is via several small pieces of microsurgical sponge spear.
A recent change in our practice in augmented trabeculectomy has been to use cut pieces of polyvinyl alcohol (PVA) sponge, instead of cut pieces of cellulose sponge for antiproliferative agent delivery to the surgical site. This change in practice was because the PVA sponges seemed to be less friable after cutting than the cellulose sponges, and less likely to leave remnants behind after removal. We carried out this study to try to confirm these suspicions. In addition, we wanted to assess whether residual microfragments of different sponge surgical spears routinely used for blood and fluid absorption during glaucoma drainage surgery are left behind.
Materials, methods, results
Four different microsurgical sponge spears were assessed: two brands of cellulose ophthalmic spears (Cellulose Spears, Eyetec Ophthalmic Products, Altomed Ltd, UK and Visispear Eye Sponge, Visitec, Becton Dickinson and Company, USA), one brand of PVA ophthalmic spear (PVA Spears, Eyetec Ophthalmic Products, Altomed Ltd, UK), and one brand of reprocessed PVA ophthalmic LASIK spear (Lasik Spear Classic, Eyetec Ophthalmic Products, Altomed Ltd, UK).
Each type of sponge spear was cut with sharp scissors into small fragments, which were then soaked in 5-fluorouracil 25 mg/ml or mitomycin C 0.2 mg/ml. Fresh cadaveric pig eyes were prepared with a fornix based conjunctival flap as if for trabeculectomy. In each eye, four antiproliferative agent soaked sponge fragments were placed with non-toothed forceps for 4 minutes on the scleral bed beneath the fornix based conjunctival flap. The sponges were removed with non-toothed forceps, and the subconjunctival space was irrigated with 10 ml balanced salt solution. The sclera and conjunctiva were fixed and processed for microscopic examination.
We also assessed whether the whole microsurgical sponge spears used for intraoperative blood and fluid absorption leave behind any microfragments. The same four types of sponge spear were each used to wipe away balanced salt solution on fresh cadaveric pig sclera, prepared with half thickness scleral incisions to simulate initial creation of a scleral flap in glaucoma drainage surgery. The sclera was then fixed and processed for microscopic examination.
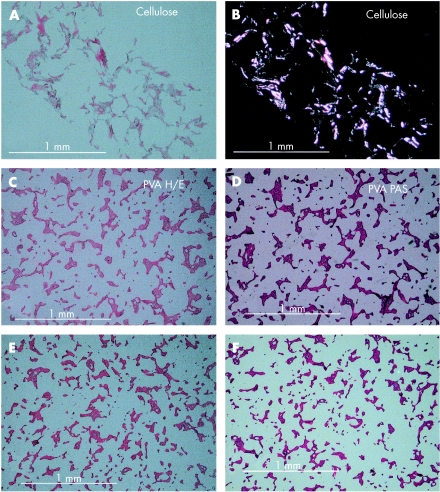
Before processing the cadaveric pig eyes, it was found that cellulose sponge was identifiable by microscopy by its birefringence in plain polarised light. PVA and reprocessed PVA were found to stain with periodic acid Schiff (PAS) stain (Fig 1). The observer of the microscopy slides was blind as to which sponge spear had been used in each case.
Figure 1.
Microscopic appearance of microsurgical sponge. (A) Cellulose, haematoxylin and eosin. (B) Cellulose, birefringence in plain polarised light. (C) Polyvinyl alcohol (PVA), haematoxylin and eosin. (D) PVA, periodic acid Schiff (PAS). (E) Reprocessed PVA, haematoxylin and eosin. (F) Reprocessed PVA, PAS. Bar = 1 mm.
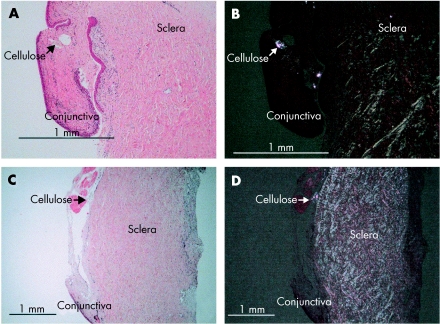
In four repeated experiments, cut pieces of both brands of cellulose microsurgical sponge spears left behind microfragments at the conjunctiva-sclera interface, when soaked with 5-fluorouracil or with mitomycin C (Fig 2). The PVA ophthalmic spears and the reprocessed PVA ophthalmic spears did not leave behind any microfragments, whether soaked with 5-fluorouracil or mitomycin C.
Figure 2.
Microscopy of the conjunctiva, sclera interface. (A) Visispear Eye Sponge (cellulose) + mitomycin C, haematoxylin and eosin. (B) Visispear Eye Sponge + mitomycin C, plain polarised light. (C) Cellulose Spear, Eyetec + 5-fluorouracil, haematoxylin and eosin. (D) Cellulose Spear, Eyetec + 5-fluorouracil, plain polarised light. Bar = 1 mm.
When whole sponge spears were used for fluid absorption, none of the four types of microsurgical sponge spear left any microfragments behind on the scleral bed. Full results are shown in Table 1.
Table 1.
Microfragments of surgical sponge spears left at the surgical site
| Sponge absorption | |||
| Sponge pieces + 5-FU | Sponge pieces + MMC | Whole fluid | |
| Cellulose spears, Eyetec | + | + | – |
| Visispear eye sponge, Visitec (cellulose) | + | + | – |
| PVA spears, Eyetec | – | – | – |
| Lasik Spear Classic, Eyetec (reprocessed PVA) | – | – | – |
Comment
This study demonstrates that in cadaveric porcine eyes cut pieces of cellulose sponge used for antiproliferative agent delivery in glaucoma filtering surgery leave behind microfragments at the conjunctival-scleral interface. Cut pieces of PVA sponge or reprocessed PVA sponge do not leave behind microfragments. This is in keeping with the marketing of PVA spears as the ideal microsurgical sponge spear for use in laser in situ keratomileusis (LASIK): when used for fluid absorption at the corneal stromal interface in LASIK, PVA is less likely to fragment and leave interface deposits than cellulose.
Antiproliferative agent delivery to the surgical site in trabeculectomy aims to reduce fibrosis, thereby promoting a functioning filtering bleb. Retained microfragments of antiproliferative soaked cellulose sponge at the surgical site may adversely affect the surgical outcome. Cellulose sponge can be regarded as a slowly degradable material. The time needed for the total disappearance of cellulose sponge from subcutaneous tissue in rats is longer than 60 weeks.3 Cellulose is also known to be capable of initiating a foreign body reaction: in the peritoneal cavity, retained cellulose can lead to a foreign body granuloma and intestinal obstruction.4 Cellulose microfragments retained in the subconjunctival space are therefore a risk to good bleb formation, and likely to be present throughout the important first weeks of healing following trabeculectomy.
Slowly degrading microfragments of foreign body may increase the risk of infection, including blebitis. In addition, retained microfragments soaked in antiproliferative agent will increase the dose of antiproliferative to the area, which in turn increases the risk of adverse effects, such as thin avascular blebs with mitomycin C. The elimination half life for intravenous 5-fluorouracil and mitomycin C is 20 hours and 50 minutes respectively; it is probably longer than this outside the vascular system, in the subconjunctival space. Larger retained sponge fragments soaked in antiproliferative can lead to necrosis of the overlying conjunctiva.5
Uncut whole sponges used for fluid absorption on the scleral bed did not leave behind microfragments on the sclera, whether made of cellulose or PVA. Therefore it may be the cutting of cellulose sponges, to provide smaller fragments for antiproliferative agent delivery, that is responsible for leaving friable cellulose edges.
Experiments using cadaveric porcine eyes might not accurately simulate the human in vivo situation. However, if the simulation is accurate, whole cellulose microsurgical spears appear to be safe for use in blood and fluid absorption in glaucoma surgery, whereas cut pieces of cellulose sponge used for antiproliferative agent delivery leave behind microfragments. We conclude that PVA microsurgical sponge is a safer vehicle for antiproliferative agent delivery in trabeculectomy.
References
- 1.Mora JS, Nguyen N, Iwach AG, et al. Trabeculectomy with intraoperative sponge 5-fluorouracil. Ophthalmology 1996;103:963–70. [DOI] [PubMed] [Google Scholar]
- 2.Palmer SS. Mitomycin as adjunct chemotherapy with trabeculectomy. Ophthalmology 1991;98:317. [DOI] [PubMed] [Google Scholar]
- 3.Martson M, Viljanto J, Hurme T, et al. Is cellulose sponge degradable or stable as implantation material? An in vivo subcutaneous study in the rat. Biomaterials 1999;20:1989–95. [DOI] [PubMed] [Google Scholar]
- 4.Tinker MA, Teicher I, Burdman D. Cellulose granulomas and their relationship to intestinal obstruction. Am J Surg 1977;133:134–9. [DOI] [PubMed] [Google Scholar]
- 5.Shin DH, Tsai CS, Kupin TH, et al. Retained cellulose sponge after trabeculectomy with adjunctive subconjunctival mitomycin C. Am J Ophthalmol 1994;118:111–12. [DOI] [PubMed] [Google Scholar]