Adenoid cystic carcinoma is a rare subtype of sweat gland carcinoma.1 In the eyelid, it can arise from the glands of Moll, the palpebral lobe of the lacrimal gland, the accessory lacrimal glands in conjunctiva, or from ectopic lacrimal gland tissue.1 We present a rare case of adenoid cystic carcinoma arising from the skin of the eyelid with features simulating the more commonly seen sebaceous gland carcinoma.
Case report
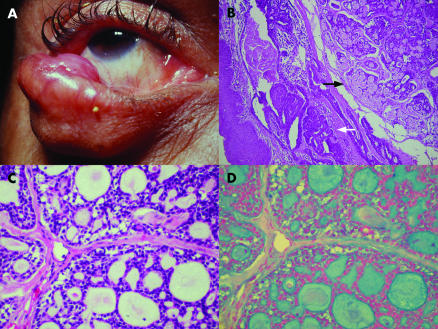
A 57 year old man presented with a lesion in the right inferior lid. He reported a slow growth during the past 10 years. The examination revealed a firm tumour occupying the lateral two thirds of the right inferior lid. There was a loss of cilia but no ulceration of the skin or conjunctiva over the lesion (Fig 1). The remainder of the examination was normal. The clinical impression was sebaceous gland carcinoma and excision with clear margins was carried out.
Figure 1.
(A) Clinically, the lesion occupied the lateral two thirds of the inferior lid with loss of the cilia in the involved area. (B) Histologically the tumour (black arrow) seems to be continuous with normal sweat glands of the skin (white arrow) (haematoxylin and eosin, ×40). (C) At higher magnification showing the characteristic cystic-like spaces (haematoxylin and eosin, ×200). (D) Same area showing positive staining for Alcian blue (Alcian blue ×200).
Histopathologically, the lesion revealed solid nests of basaloid cells associated with numerous cystic spaces containing Alcian blue positive material and scant fibrous stroma. The neoplastic process seems to originate from an area of normal sweat glands of the lid skin. In some areas, the cells assumed a strand-like configuration forming glandular duct-like spaces (Fig 1). There was no continuity to the epidermis, hair sheaths, or conjunctiva, indicating origin of the tumour from skin sweat glands. The surgical margins were free of tumour. The final diagnosis was adenoid cystic carcinoma. After 18 months, no local recurrence or distant metastasis were noted.
Comment
The present case revealed clinical features commonly seen in association with eyelid sebaceous gland carcinoma. These included loss of cilia and a large slowly growing mass. It thus emphasises the need for including adenoid cystic carcinoma in the differential diagnosis of eyelid malignant tumours, albeit such tumours are rare.
In a review of the literature on eyelid tumours, at least three previous reports of adenoid cystic carcinoma can be found1–3; however, in two such reports no definite conclusion about the origin of the tumour is offered.1,2 In the case reported by Mencia-Gutiérrez et al, the tumour appears to be primarily of the skin.3
Fewer than 50 cases of adenoid cystic carcinoma primarily of the skin have been reported.3 Its most common differential diagnosis is the adenoid basal cell carcinoma. While both lesions have an infiltrative growth pattern and share many histological features, like the tendency to invade perivascular and perineural spaces, some aspects can help to differentiate them. Adenoid cystic carcinoma presents lack of retraction artefact, absence of contiguity with the epidermis or hair sheaths, lack of peripheral palisading of the nuclei, and occasional presence of central apoptotic or even necrotic cells. In the rare instances when haematoxylin and eosin stained sections are not sufficient to differentiate the two lesions, adenoid cystic carcinoma pseudocysts stain positively to Alcian blue and periodic acid-Schiff (PAS). The tumour also shows positive immunostaining with EMA (epithelial membrane antigen), amylase, S100 protein, and carcinoembryonic antigen.1,4–6
Adenoid cystic carcinoma of the eyelid skin is a tumour of middle aged adults, present for a long period before the patient seeks medical attention. Unlike most of the sweat gland carcinomas, it tends to recur locally and rarely spreads to lymph nodes or distant organs.4–6 Thus, local resection with verification of the margins is the recommended treatment and regional lymph nodes resection seems not to be necessary.4 When complete excision is not possible radiotherapy and chemotherapy have been employed as adjuvant or palliative treatment.7
References
- 1.Font RL. Eyelid and lacrimal drainage system. In: Spencer WH, ed. Ophthalmic pathology: an atlas and textbook. 4th ed. Philadelphia: WB Saunders, 1996:2307–8.
- 2.Kersten RC, Ewing-Chow D, Kulwin DR, et al. Accuracy of clinical diagnosis of cutaneous eyelid lesions. Ophthalmology 1997;104:479–84. [DOI] [PubMed] [Google Scholar]
- 3.Mencía-Gutierréz E, Guttierréz-Diaz E, Santos-Briz A, et al. Primary cutaneous adenoid cystic carcinoma of the eyelid. Am J Ophthalmol 2001;131:281–3. [DOI] [PubMed] [Google Scholar]
- 4.Cooper HC. Carcinomas of sweat glands. Pathol Annu 1987;22:83–124. [PubMed] [Google Scholar]
- 5.Murphy GF, Elder DE. Non-melanocytic tumors of the skin. Atlas of tumor pathology. 3rd series. Fascicle 1. Washington DC: Armed Forces Institute of Pathology, 1991:105.
- 6.Wick MR, Swanson PE, Barnhill RL. Sweat gland tumors. In: Barnhill RL, ed. Textbook of dermatopathology. New York: McGraw-Hill, 1998:637.
- 7.Kato N, Yasukawa K, Onozuka T. Primary cutaneous adenoid cystic carcinoma with lymph node metastasis. Am J Dermatopathol 1998;20:571–7. [DOI] [PubMed] [Google Scholar]