Abstract
Aim: To evaluate the morphology of the optic nerve head in an unselected population group in south India.
Methods: The study included 70 subjects forming a population based sample, selected in a random manner. Mean age was 47.5 (SD 8.7) years, mean refractive error measured −0.07 (1.11) dioptres (range −4.50 to +2.50 dioptres). Optic disc slides were morphometrically analysed.
Results: Mean optic disc area measured 2.58 (0.65) mm2. It was statistically independent of age and refractive error. Optic disc shape was slightly vertically oval. Mean neuroretinal rim area was 1.60 (0.37) mm2. It was significantly and positively correlated with optic disc size and optic cup size. It was independent of age, sex, refractive error, and axial length. In all subjects included in the study, the rim was smallest in the temporal horizontal optic disc sector. Mean horizontal cup/disc diameter ratio (0.66 (0.07)) was significantly (p<0.001) higher than the mean vertical cup/disc diameter ratio (0.56 (0.08)). Both ratios were highly significantly (p <0.001) and positively correlated with optic disc size. The α zone of parapapillary atrophy (0.84 (0.29) mm2), and β zone (0.13 (0.38) mm2), respectively, occurred in 69 (98.6%) subjects and in eight (11.4%) subjects, respectively. They were significantly larger in the temporal horizontal sector. The α zone was significantly (p<0.001) larger and occurred significantly more often than β zone. Retinal arterioles and venules were wider, and in spatial correlation, the visibility of the retinal nerve fibre layer was significantly better, in the temporal inferior disc arcade and the temporal superior arcade than in the nasal superior arcade and the nasal inferior vessel arcade. Except for the absolute size measurements these optic nerve head parameters did not differ markedly (p >0.05) from the values found in white people.
Conclusions: South Indians and white people do not show marked differences in the morphology of the optic nerve head as measured by morphometric optic disc parameters, with the possible exception of the absolute optic disc dimensions.
Keywords: optic disc, optic nerve head, neuroretinal rim, parapapillary atrophy, retinal nerve fibre layer
The optic disc as the bottleneck of the whole visual afference is of great importance for the diagnosis of optic nerve anomalies and diseases. Since the morphology, including the measurements of the optic disc, depends on the ethnic background of the subject, the purpose of this study was to evaluate the appearance of the optic nerve head in south Indians, with the aim of providing standard measurements of the normal optic nerve head in this population group, and to compare these measurements with the optic disc data of other ethnic groups.1–4 By comparing the results of this study with findings of studies on patients with optic nerve diseases, the results of the present study may also be helpful in describing morphological optic disc parameters for the early detection of optic nerve diseases, including glaucoma in the south Indian population group.
SUBJECTS AND METHODS
The study included 70 subjects (42 women, 28 men) forming a population based sample, selected in a random manner. In 1995, using a stratified simple random sampling technique, a study population of 1932 people from 12 random clusters of a defined urban population in Vellore, Tamil Nadu was identified, of which 1521 subjects could be contacted. Of these 1521 subjects, 972 (63.9% of the invited population) people were examined in the Vellore Eye Survey.5 In September 2000, all these 972 people were invited for a review examination.
With the aim of getting 100 normal subjects randomly selected from the 972 subjects of the original population that was examined, we invited a subset of 300 people previously diagnosed as normal with the aim of recruiting a minimum of 100 control subjects. “Normal” meant no occludable anterior chamber angles upon gonioscopy. The normal subset was selected in a random manner as follows: people who participated in the previous study were assigned hospital numbers in chronological order. From the database we extracted information on which population cluster they belonged to and arranged them in chronological order of the date of examination in the hospital. The first 25 people from each cluster were identified and invited for examination. The next 10 people were short listed. If a person from the first list could not be contacted, the next (short listed) person was contacted. A total of 300 people were identified and 120 short listed. The incentive offered was free examination and treatment at the hospital. These individuals were approached by a social worker and invited to undergo follow up examination at the hospital. All selected individuals were given a specific date for examination. In the case of non-response the social worker once again contacted the selected individual population and a fresh appointment date was fixed. If the second appointment was also missed, the next person on the short list from that cluster was invited for examination. Of the 300 people contacted 110 people responded. Seventy five subjects had changed residence and could not be traced, 23 people could not be contacted, one person was an invalid and could not come to the hospital, one person refused the examination, and 90 people did not come for examination despite repeated requests. For 70 (63.6%) of the 110 people, optic disc photographs in sufficient quality were available. Details of the survey methodology and results of the Vellore Eye Study have been published earlier.5 The methods applied and the study itself adhered to the tenets of the Declaration of Helsinki for the use of human subjects in biomedical research. Informed consent was obtained from each subject before enrolment. As the original study was a survey and both phases of the study had no intervention, ethics committee approval was not required. Mean age was 47.5 (8.7) years (median 49 years; range 32–69 years), mean refractive error measured −0.07 (1.11) dioptres (median 0 dioptres; range −4.50 to +2.50 dioptres).
All subjects underwent standardised ophthalmic examination including keratometry, refractometry, measurement of visual acuity, applanation tonometry, slit lamp biomicroscopy of anterior segment of the eye, gonioscopy, ophthalmoscopy, and sonographic determination of the anterior chamber depth and axial length of the globe. Using a conventional fundus camera (Carl Zeiss, Oberkochen, Germany; camera model number FF450), 30° sequential stereo colour optic disc photographs were taken in medical mydriasis for all subjects. The optic disc slides were projected in a scale of 1–15. The outlines of the optic cup, optic disc, and peripapillary scleral ring were plotted on paper and morphometrically analysed. To obtain values in absolute size units—that is, mm or mm2, the ocular and photographic magnification was corrected using the Littmann method.6 The optic cup was defined on the basis of contour and not of pallor. The border of the optic disc was identical with the inner side of the peripapillary scleral ring. Parapapillary atrophy was differentiated into a peripheral α zone with irregular pigmentation, and a central β zone with visible sclera and visible large choroidal vessels. To compare various optic disc regions with each other, the intrapapillary region was divided into four sectors. The temporal superior sector and the temporal inferior disc sector were right angled and were tilted 15° temporal to the vertical optic disc axis. The two other sectors covered the remaining area: the temporal horizontal sector was 60 degrees wide, and the nasal disc sector covered 120°. In each of the four sectors, the size of the neuroretinal rim and optic cup were measured separately. The diameters of the retinal arterioles were measured at the optic disc border in the inferotemporal, superotemporal, superonasal, and inferonasal region. The method has already been described in detail.7
Additionally, the visibility of the retinal nerve fibre layer was evaluated. Using a subjective score ranging between “8” for “very good detectability” to “0” for “no retinal nerve fibre layer detectable,” the visibility of the retinal nerve fibre layer was evaluated in eight fundus sectors: temporal inferior, temporal horizontal, temporal superior, superior, nasal superior, nasal horizontal, nasal inferior, and inferior. The intraobserver variation of this method had been evaluated in a previous study.8
RESULTS
Optic disc
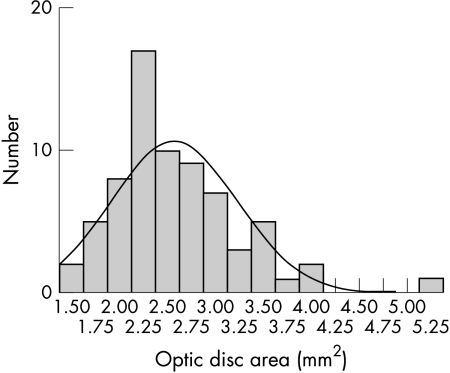
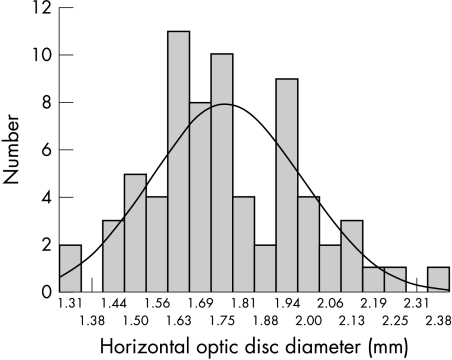
The area of the optic disc with a mean of 2.58 mm2 showed an interindividual variability of 1:3.6 (Table 1) (Fig 1). In the south Indians, optic disc area was statistically independent of age (correlation coefficient r = −0.07; p=0.59) and refractive error (correlation coefficient r = 0.11; p=0.38). Male subjects had a larger, however not statistically significantly larger (p=0.60), optic disc than female subjects (Table 1). The optic disc area was statistically independent of the axial length of the eye (correlation coefficient r = −0.08; p=0.53) and the depth of the anterior chamber (correlation coefficient r = −0.08; p=0.54). Mean horizontal diameter of the optic disc was 1.77 (SD 0.22) mm (Fig 2) which was significantly (p<0.001) smaller than the vertical disc diameter (Table 1).
Table 1.
Optic disc measurements in a randomly selected sample of 70 subjects from Vellore, Tamil Nadu
| Mean (SD) | SE | Median | Range | |
| Optic disc | ||||
| Area (mm2) | 2.58 (0.65) | 0.08 | 2.44 | 1.43–5.15 |
| Disc area in women | 2.51 (0.53) | 0.08 | 2.42 | 1.43–3.60 |
| Disc area in men | 2.68 (0.81) | 0.15 | 2.56 | 1.44–5.15 |
| Disc diameter (mm) | ||||
| Horizontal | 1.77 (0.22) | 0.03 | 1.73 | 1.31–2.40 |
| Vertical | 1.87 (0.24) | 0.03 | 1.85 | 1.42–2.74 |
| Horizontal/vertical disc diameter | 1.06 (0.06) | 0.01 | 1.06 | 0.91–1.21 |
| Neuroretinal rim | ||||
| Area (mm2), total | 1.60 (0.37) | 0.04 | 1.50 | 1.08–2.85 |
| Temporal horizontal | 0.18 (0.07) | 0.01 | 0.16 | 0.07–0.37 |
| Temporal inferior | 0.42 (0.13) | 0.02 | 0.40 | 0.22–0.87 |
| Temporal superior | 0.43 (0.11) | 0.01 | 0.41 | 0.24–0.80 |
| Nasal | 0.58 (0.14) | 0.02 | 0.55 | 0.36–1.01 |
| Width (mm) | ||||
| Temporal horizontal | 0.19 (0.05) | 0.006 | 0.18 | 0.09–0.37 |
| Temporal inferior | 0.29 (0.06) | 0.007 | 0.28 | 0.20–0.44 |
| Temporal superior | 0.30 (0.06) | 0.007 | 0.30 | 0.18–0.53 |
| Nasal | 0.31 (0.05) | 0.006 | 0.30 | 0.20–0.50 |
| Inferior to temporal rim width ratio | 1.67 (0.54) | 0.06 | 1.58 | 1.02–3.83 |
| Superior to temporal rim width ratio | 1.71 (0.40) | 0.05 | 1.61 | 1.02–2.70 |
| Optic cup | ||||
| Area (mm2), total | 0.98 (0.40) | 0.05 | 0.88 | 0.22–2.30 |
| Diameter (mm) | ||||
| Horizontal | 1.16 (0.23) | 0.03 | 1.12 | 0.64–1.82 |
| Vertical | 1.06 (0.23) | 0.03 | 1.04 | 0.45–1.70 |
| Horizontal/vertical cup diameter ratio | 1.11 (0.12 | 0.01 | 1.07 | 0.84–1.43 |
| Cup/disc diameter ratios | ||||
| Horizontal | 0.66 (0.07) | 0.008 | 0.66 | 0.43–0.80 |
| Vertical | 0.56 (0.08) | 0.01 | 0.57 | 0.31–0.70 |
| Horizontal/vertical cup/disc diameter ratio | 1.18 (0.13) | 0.02 | 1.18 | 0.91–1.56 |
| Cup/disc area ratio | 0.37 (0.08) | 0.01 | 0.37 | 0.15–0.55 |
SD = standard deviation; SE = standard error.
Figure 1.
Histogram showing the distribution of optic disc area in a randomly selected sample of 70 subjects from Vellore, Tamil Nadu.
Figure 2.
Histogram showing the distribution of horizontal optic disc diameter in a randomly selected sample of 70 subjects from Vellore, Tamil Nadu.
The shape of the optic disc was slightly vertically oval with the vertical disc diameter being about 6% longer than the horizontal disc diameter (Table 1). In 57 (81.4%) eyes, the vertical optic disc was longer than the horizontal axis, and in 10 (14.3%) eyes, the horizontal optic disc was longer than the vertical optic disc axis. In three eyes, the horizontal disc diameter equalled the vertical disc diameter.
Neuroretinal rim
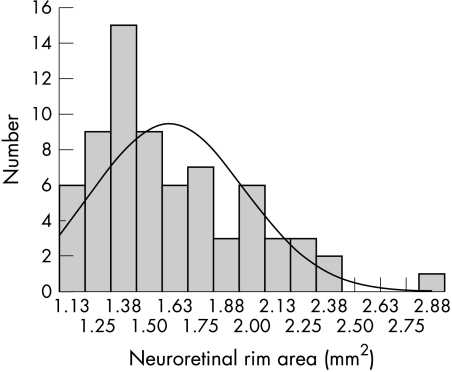
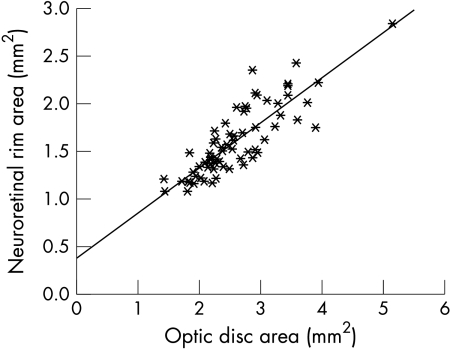
Mean area of the neuroretinal rim was 1.60 mm2 (SD 0.37 mm2) (Fig 3). It was significantly and positively correlated with the size of the optic disc (Fig 4) and area of the optic cup (correlation coefficient r = 0.47; equation of the regression line: neuroretinal rim area (mm2) = 0.44 × (optic cup area (mm2)) + 1.59; p<0.001). The rim size was statistically independent of age (p=0.27; correlation coefficient r = −0.14), sex (p=0.88), refractive error (p=0.37), axial length of the globe (correlation coefficient r = −0.04; p=0.77), and depth of the anterior chamber (correlation coefficient r = −0.04; p=0.78).
Figure 3.
Histogram showing the distribution of neuroretinal rim area in a randomly selected sample of 70 subjects from Vellore, Tamil Nadu.
Figure 4.
Histogram showing the correlation between neuroretinal rim area and optic disc area in a randomly selected sample of 70 subjects from Vellore, Tamil Nadu. (Correlation coefficient r = 0.85; equation of the regression line: neuroretinal rim area (mm2) = 0.48 × optic disc area (mm2) + 0.37; p <0.001.)
The shape of the neuroretinal rim showed a characteristic pattern. In all subjects included in the study, the rim was smallest in the temporal horizontal optic disc sector. Correspondingly, the rim was highly significantly (p<0.001) thinner in the temporal horizontal disc sector than in any of the three other disc sectors. The width of the neuroretinal rim did not vary markedly between the three other optic disc sectors (Table 1). Accordingly, the area of the neuroretinal rim was significantly (p<0.001) the smallest in the temporal horizontal disc sector. The ratio of inferior to temporal rim width did not vary significantly from the superior to temporal rim width ratio (Table 1). In all eyes, both ratios were higher than 1.0 according to the finding that, in all subjects, the rim width was smallest in the temporal optic disc sector. The rim width ratios were statistically dependent on the shape of the optic disc (p=0.03 and p=0.006). The more vertically configured the optic disc was, the higher was the inferior to temporal rim width ratio and the superior to temporal rim width ratio. Both rim width ratios were statistically independent of refractive error and age (p>0.25).
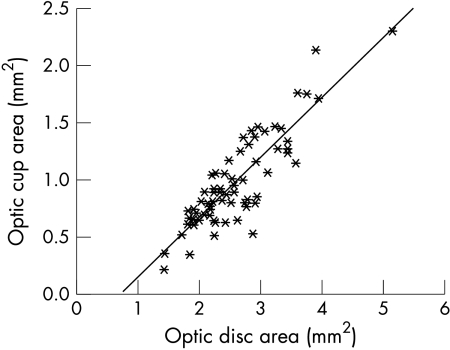
Optic cup
Mean area of the optic cup was 0.98 mm2 (Table 1). The area of the optic disc was significantly and positively correlated with the size of the optic cup (Fig 5). The larger the optic disc, the larger the optic cup. The area of the optic cup was independent of age (p=0.90), refractive error (p=0.53), sex (p=0.56), axial length of the globe (correlation coefficient r = −0.09; p=0.44), and depth of the anterior chamber (correlation coefficient r = −0.09; p=0.45).
Figure 5.
Scattergram showing the correlation between optic cup area and optic disc area in a randomly selected sample of 70 subjects from Vellore, Tamil Nadu. (Correlation coefficient r = 0.87; equation of the regression line: optic cup area (mm2) = 0.52 × optic disc area (mm2) − 0.37; p <0.001.)
The horizontal optic cup diameter was significantly (p<0.001) longer than the vertical cup diameter (Table 1) indicating a horizontally oval shape of the optic cup.
Cup/disc ratios
The mean horizontal cup/disc diameter ratio was 0.66 (SD 0.07) and mean vertical cup/disc diameter ratio was 0.56 (SD 0.08) (Table 1). The vertical cup/disc diameter ratio was highly significantly (p<0.001) larger than the horizontal one. Consequently, the quotient of the horizontal to vertical cup/disc diameter ratio was higher than 1.0. In three (4.3%) subjects, it was smaller than 1.0. Both the horizontal cup/disc diameter ratio and the vertical ratio were highly significantly (p<0.001) and positively correlated with the optic disc size (correlation coefficient r = 0.75; equation of the regression line: vertical cup/disc diameter ratio = 0.034 × (optic disc area (mm2)) + 0.44; p<0.001). The correlation coefficients were higher for the vertical ratio (correlation coefficient r = 0.75) than for the horizontal ratio (correlation coefficient r = 0.41). The quotient of vertical to horizontal cup/disc diameter ratio was statistically independent of the optic disc size (p=0.33).
The cup/disc area ratio was on an average 0.37 (SD 0.08). As the cup/disc diameter ratio, the cup/disc area ratio was highly significantly and positively correlated with the optic disc area (correlation coefficient r = 0.41; p<0.001). It was independent of age (p=0.52), refractive error (p=0.94), and sex (p=0.24).
Parapapillary atrophy
The α zone of the parapapillary atrophy was significantly (p<0.001) the largest in the temporal horizontal sector followed by the temporal inferior sector, in which it was significantly (p<0.001) larger than in the temporal superior sector, in which it was significantly (p<0.001) larger than in the nasal sector (Table 1). Correspondingly, the width of the α zone was significantly (p<0.001) larger in the temporal horizontal sector than in the temporal inferior sector, in which it was significantly (p<0.001) wider than in the temporal superior sector, in which it was significantly (p<0.001) wider than in the nasal sector (Table 1).
The α zone was found in 69 (98.6%) out of the 70 subjects (Table 1). Frequency of the α zone did not vary significantly between the temporal horizontal sector, the temporal inferior sector, and the temporal superior sector. In all three sectors, it occurred significantly (p<0.001) more often than in the nasal sector.
In a similar manner, the β zone was larger, however not significantly (p=0.069) larger, in the temporal horizontal sector than in the temporal inferior sector and temporal superior sector (Table 1). The latter two sectors did not vary significantly (p=0.33) in area of beta zone. In both sectors, beta zone area was significantly (p=0.01) larger than in the nasal sector (Table 1). Correspondingly, the width of β zone was significantly (p=0.01) larger in the temporal horizontal sector than in the temporal inferior sector and the temporal superior sector. The latter two sectors did not vary significantly in the width of the β zone (p=0.40). In both sectors, the β zone was significantly (p=0.01) wider than in the nasal sector (Table 1).
The β zone was detected in eight (11.4%) of the 70 subjects (Table 1). The frequency of the β zone did not vary significantly between the temporal superior sector, the temporal inferior sector, and the temporal superior sector. In all three sectors, it occurred significantly (p<0.01) more often than in the nasal sector.
Comparing α zone with β zone, the α zone was significantly (p<0.001) larger and occurred significantly (p<0.001) more frequently than the β zone in each of the four sectors.
The size of the α and β zones were statistically independent of refractive error (p=0.77 and p=0.15, respectively) and age (p=0.45 and p=0.79, respectively). The size of the α zone was significantly and positively correlated with the optic disc area (correlation coefficient r = 0.37; equation of the regression line: area of the α zone (mm2) = 0.12 × optic disc area (mm2) + 0.42; p=0.002) and area of the neuroretinal rim (area of α zone (mm2) = 0.20 × neuroretinal rim area (mm2) + 0.40; p=0.004). Size of β zone was independent of optic disc area (p=0.52) and rim size (p=0.19). The areas of both zones were significantly (p=0.025) and positively correlated with each other (correlation coefficient r = −0.27; equation of the regression line: area of α zone (mm2) = −0.21 area of β zone (mm2) + 0.87).
Retinal vessel diameter
The diameter of the retinal arterioles was significantly (p<0.001) larger in the temporal inferior arcade and the temporal superior arcade than in the nasal superior arcade or the nasal inferior arcade (Table 1). Correspondingly, the retinal venules were significantly (p<0.001) wider in the temporal inferior arcade and the temporal superior arcade than in the nasal superior arcade or the nasal inferior arcade (Table 1).
Retinal nerve fibre layer visibility
The retinal nerve fibre layer was significantly (p=0.035) more visible in the temporal inferior arcade than in the temporal superior arcade in which was significantly (p<0.001) more detectable than in the nasal superior arcade or the nasal inferior arcade (Table 1). Between the two latter regions, retinal nerve fibre layer visibility did not vary significantly (p=0.34). Total retinal nerve fibre layer visibility was not significantly correlated with optic disc area (p=0.67), refractive error (p=0.87), and sex (p=0.34). The retinal nerve fibre layer decreased marginally statistically significantly with increasing age (equation of the regression line: retinal nerve fibre layer visibility = −0.14 × age (years) + 35.1; correlation coefficient: −0.23; p=0.07).
DISCUSSION
Optic disc area
In the south Indian population group examined in this study, the optic disc area showed an interindividual variability of 1:3.6 (Fig 1). A similar observation has been made in previous studies on white people, in which the optic disc area showed an interindividual variability of about 0.80 mm2 to almost 6.00 mm2 in a normal population.4,9–12 In both population groups, there were normal eyes with rather small optic discs, and there were normal eyes with very large optic discs. In both population groups, optic disc area was independent of age beyond an age of about 10 years.4,9,11,12 With regard to sex, the results are not conclusive. In the present investigation, male subjects had a larger, however not significantly (p=0.60) larger, optic disc area than female subjects (Table 1). One may argue that the difference of 2.68 mm2 (men) to 2.51 mm2 (women) would have become statistically significant with a larger number of subjects included in the study. The Rotterdam Study, as one of the largest epidemiological studies on the morphology of the optic nerve head in white people, has demonstrated that the mean optic disc area is on average 3.2% larger in men than in women.11 Similar findings have been reported in the Baltimore Eye Survey as well as in a recent meta-analysis.4,13
In a similar manner, optic disc area was statistically independent of refractive error and axial length in the present study on south Indians as well as in several studies on white people if highly myopic eyes and highly hyperopic eyes were excluded from the analysis.4,9,11,12 In the large Rotterdam study, however, disc area linearly increased slightly and significantly by 1.2% (0.15%) for each dioptre increase towards myopia.11 All studies agree that optic disc size is significantly larger with highly myopic eyes, and that it is significantly smaller in eyes with marked hyperopia (more than +5 D), than in eyes with a normal refractive error.14
In the south Indian population group included in this study, optic disc area did not differ significantly from the optic disc area found in a study on 319 white subjects in which a similar planimetric technique of evaluating optic disc photographs and the same method to correct the magnification of fundus images were applied.9 Accordingly, the horizontal cup/disc diameter ratio measured in the present study did not vary significantly from the horizontal cup/disc diameter ratio determined in previous studies on a group of 1246 white eyes (0.66 (0.07) (median 0.66) versus 0.61 (0.19) (median, 0.66); p=0.60).15 The vertical cup/disc diameter ratio was even slightly smaller in the present study compared with the studies on white subjects (0.56 (0.08) (median 0.57) versus 0.57 (0.18) (median 0.60) versus; p=0.02). Correspondingly, comparing the optic disc area measurements obtained in the present study with the optic disc measurements of white people examined in the Baltimore Eye Survey (mean optic disc area 2.63 mm2) and in the Rotterdam Study (2.42 mm2), the differences were not remarkable.4,11 One has to take into account, however, that all optic disc measurements in mm or mm2, as given in the present study, are more or less relative measurements since it has been uncertain whether the technique of correcting the magnifying effect of the ocular optic media and of the fundus camera on the size of the optic disc image has been completely correct. This limitation of the study does not hold true for the main results of the study—that is, the correlation between the optic disc parameters and the description of the size and frequency of the optic disc features. The question arises whether correlations between disc size and other parameters which were significant for white groups are also valid for south Indians. To mention some examples, in non-highly myopic white people, the optic disc size is correlated with the size of the globe, the count of rods, cones, and retinal ganglion cell axons; the number and area of lamina cribrosa pores; and the frequencies of some optic nerve anomalies and diseases such as optic disc drusen, pseudopapilloedema, non-arteritic anterior ischaemic optic neuropathy, pits of the optic disc, and the morning glory syndrome.15,16 If these correlations also hold true in south Indian eyes, it may be important for pathogenic considerations such as glaucoma susceptibility, and there may be clinical implications for the clinical diagnosis and prevalence of certain optic nerve anomalies and diseases.
The optic disc area measurements reported in the present study are smaller than the optic disc measurements obtained in the Andhra Pradesh Eye Disease Study which was also carried out in south India and in which a similar technique as in the present study was used.17 In the Andhra Pradesh Study, mean optic disc area was 3.37 mm2 (SD 0.68 mm2; range 1.95–6.82 mm2). The question arises whether differences in the technique for correcting the magnification of fundus images may be responsible for the discrepancy between the two studies. To mention examples, optic disc measurements vary according to the method applied. Mean optic disc area of non-highly myopic whites examined in various studies ranged between 2.1 mm2 and about 2.8 mm2.4,9,11,12,15 Future studies examining Indians and white people and using the identical technology such as a confocal laser scanning tomograph of the same brand may eventually answer the question whether the optic disc size differs between both population groups.
Optic disc diameters
The horizontal diameter and the vertical diameter of the optic disc were not interindividually constant; they showed an interindividual variability of about 1:2 (Table 1) (Fig 2). Similar figures have been reported for white people.9 In spite of that, the optic disc diameter has been taken as a relative size unit to interindividually compare the size of intraocular lesions such as malignant melanomas and, more recently, to assess the size of subfoveal neovascular membranes.18 It may lead to an underestimation of the size of the lesion in eyes with a large optic disc and to an overestimation of the size of the lesion in eyes with a small optic nerve head. One may, therefore, suggest, that in studies on white people or on south Indians in which different individuals are compared with each other, fundus lesions should be measured in absolute size units with correction for the photographic magnification instead of taking the interindividually variable disc diameter as the relative measure unit.
Optic disc shape
In the south Indian population group the vertical diameter of the optic disc was about 6% longer than the horizontal one. Similar findings were reported for whites in whom the vertical optic disc diameter was about 6%–10% longer than the horizontal one.9 In both population groups, the disc shape was independent of age, sex, and refractive error.9,15
Neuroretinal rim
The neuroretinal rim as the intrapapillary equivalent of the optic nerve fibres is one of the main targets in the morphometric analysis of the optic nerve head. In the present study, mean rim size measured 1.60 mm2 (SD 0.37 mm2). These figures were smaller than the rim area measurements in the Andra Pradesh Study in which mean rim area was 2.79 mm2 (SD 0.52 mm2).17 One of the reasons for the discrepancy in rim area with no difference in disc area between the two studies may be how the border between optic cup and rim was plotted.
As with optic disc size, the neuroretinal rim area showed a marked interindividual variability of about 1:2.64 (Fig 3). Similar findings have been reported for white people.1,3,4,15,19,20 It demonstrates that owing to the marked interindividual variability in rim area found for both population groups, the neuroretinal rim area as a single parameter may not be precise enough to differentiate between normal eyes and eyes with early glaucoma. To increase the predictive value of the neuroretinal rim area in differentiating normal eyes from eyes with early glaucoma, it may be helpful to use the equation of the regression line describing the relation between disc area and rim area to correct the neuroretinal rim area for its dependence on the optic disc area.
In the subjects examined in this study, the neuroretinal rim showed a characteristic configuration. In all eyes, the smallest rim part was in the temporal optic disc sector. This physiological rim configuration is based on the vertically oval shape of the optic disc and the horizontally oval shape of the optic cup. In studies on whites, the ISN‘T rule was defined with the neuroretinal rim being usually broadest in the Inferior disc region, followed by the Superior disc region, the Nasal disc area, and finally the Temporal disc region.9 A similar configuration of the neuroretinal rim was also detected for the south Indian population, with the slight difference that in the population group in the present study, the rim was not significantly broader in the inferior temporal disc sector than in the superior temporal disc sector or the nasal disc region. The most important part of the ISN‘T rule, that the smallest rim part is located in the temporal horizontal disc sector, however, was confirmed for the south Indian population. Correspondingly, the ratios of inferior to temporal rim width and of superior to temporal rim width were comparable in the south Indian population of this study and in the white people examined in previous studies.21 The feature of the neuroretinal rim configuration is of utmost importance in the diagnosis of early glaucomatous optic nerve damage in ocular hypertensive eyes before the development of visual field defects in white on white perimetry.15
Optic cup
Parallel to the optic disc and the neuroretinal rim, the optic cup also showed a high interindividual variability in the eyes examined in the present study. As already shown in the Andra Pradesh Study as well as for eyes of white people, the areas of the optic disc and optic cup were positively correlated with each other: the larger the optic disc, the larger the optic cup (Fig 5).4,9,17,19 In the morphological diagnosis of glaucoma in south Indians as well as in white people, this feature has to be taken into account. Early or moderately advanced glaucomatous optic nerve damage may erroneously be overlooked in small optic discs with relatively small optic cups, if one does not take into account that small optic discs normally have no optic cup. The shape of the optic cup was horizontally oval with the horizontal cup diameter being about 11% longer than the vertical cup diameter.
Cup/disc ratios
Owing to the vertically oval optic disc and the horizontally oval optic cup, the cup/disc ratios were horizontally significantly (p<0.001) higher than vertically. Similar findings have been reported for eyes of white people as well as in the Andra Pradesh Study.9,17 The high interindividual variability of the optic disc and cup diameters explain the fact that the cup/disc ratios ranged in the normal south Indian population of this study between 0.3 and 0.8 (Table 1). Owing to the correlation between disc area and cup area (Fig 5), they are low in small optic nerve heads, and they are high in large optic discs. An unusually high cup/disc ratio, therefore, can be physiological in eyes with large optic nerve heads, while an average cup/disc ratio is uncommon in normal eyes with small optic discs. This finding is important for the diagnosis of glaucoma.
Owing to their marked interindividual variability, the horizontal and vertical cup/disc diameter ratios can have a relatively low diagnostic power to differentiate between normal eyes and eyes with early glaucoma. Their diagnostic power increases significantly if their dependency on the optic disc size is taken into account.20
Parapapillary chorioretinal atrophy
Ophthalmoscopically, parapapillary chorioretinal atrophy has been divided into a central β zone and a peripheral α zone.7 The peripheral zone (α zone) is characterised by an irregular hypopigmentation and hyperpigmentation and thinning of the chorioretinal tissue layer. On its outer side it is adjacent to the retina, and on its inner side it is in touch with a zone characterised by visible sclera and visible large choroidal vessels (β zone), or with the peripapillary scleral ring. Features of the inner zone (β zone) are marked atrophy of the retinal pigment epithelium and of the choriocapillaris, good visibility of the large choroidal vessels and the sclera, thinning of the chorioretinal tissues, and round boundaries to the adjacent α zone on its peripheral side and to the peripapillary scleral ring on its central side. If both zones are present, the β zone is always closer to the optic disc than the α zone.
In the south Indian subjects included in the present study, the α and β zone were largest in the temporal horizontal sector, followed by the inferior temporal area and the superior temporal region. Both zones were smallest in the nasal parapapillary area. The differences between the sectors were highly significant for the α zone (Table 2). Both zones occurred more frequently in the temporal sector than in the nasal sector. A similar distribution has been reported for eyes of white people in previous studies.7 In the present investigation, comparing both zones with each other, the α zone was significantly larger and occurred significantly more often than β zone in each of the four parapapillary sectors (Table 2). Again, the same findings were made for white people.7 Assuming that in south Indian eyes glaucoma is associated with an enlargement of parapapillary atrophy, especially of the β zone, as it has already been demonstrated for white people,7,22 the data found in the present investigation may be helpful in detecting glaucoma in south Indian patients. With β zone found in 11% of the normal south Indian subjects, the presence of the β zone as a morphological parameter may have a relatively high specificity in the differentiation between normal eyes and glaucomatous eyes of south Indian patients.
Table 2.
Optic disc measurements of the parapapillary region
| Mean (SD) | SE | Range | Frequency | |
| α zone area (mm2); total | 0.74 (0.26) | 0.03 | 0.00–1.47 | 69/70 = 98.6% |
| Temporal horizontal | 0.32 (0.13) | 0.01 | 0.00–0.75 | 69/70 = 98.6% |
| Temporal inferior | 0.25 (0.11) | 0.01 | 0.00–0.56 | 69/70 = 98.6% |
| Temporal superior | 0.15 (0.08) | 0.01 | 0.00–0.42 | 68/70 = 97.1% |
| Nasal | 0.02 (0.08) | 0.01 | 0.00–0.49 | 20/70 = 28.6% |
| Width (mm), temporal horizontal | 0.29 (0.11) | 0.01 | 0.00–0.66 | |
| Temporal inferior | 0.15 (0.07) | 0.01 | 0.00–0.34 | |
| Temporal superior | 0.09 (0.04) | 0.005 | 0.00–0.23 | |
| Nasal | 0.01 (0.03) | 0.004 | 0.00–0.21 | |
| β zone; total | 0.10 (0.28) | 0.03 | 0.00–1.27 | 8/70 = 11.4% |
| Temporal horizontal | 0.04 (0.13) | 0.02 | 0.00–0.59 | 8/70 = 11.4% |
| Temporal inferior | 0.03 (0.11) | 0.01 | 0.00–0.64 | 8/70 = 11.4% |
| Temporal superior | 0.02 (0.05) | 0.01 | 0.00–0.28 | 8/70 = 11.4% |
| Nasal | 0.001 (0.01) | 0.001 | 0.00–0.05 | 1/70 = 1.4% |
| Width (mm), temporal horizontal | 0.05 (0.13) | 0.02 | 0.00–0.59 | |
| Temporal inferior | 0.02 (0.06) | 0.01 | 0.00–0.37 | |
| Temporal superior | 0.01 (0.04) | 0.006 | 0.00–0.21 | |
| Nasal | 0.001 (0.001) | 0.001 | 0.00–0.03 | |
| Arteriole diameter (mm); | ||||
| Temporal inferior | 0.106 (0.021) | 0.003 | 0.070–0.160 | |
| Temporal superior | 0.104 (0.019) | 0.002 | 0.070–0.170 | |
| Nasal superior | 0.091 (0.023) | 0.003 | 0.050–0.160 | |
| Nasal inferior | 0.092 (0.022) | 0.003 | 0.040–0.150 | |
| Venule diameter (mm); | ||||
| Temporal inferior | 0.131 (0.030) | 0.004 | 0.070–0.200 | |
| Temporal superior | 0.134 (0.030) | 0.004 | 0.070–0.210 | |
| Nasal superior | 0.109 (0.027) | 0.003 | 0.070–0.210 | |
| Nasal inferior | 0.110 (0.027) | 0.003 | 0.070–0.180 | |
| RNFL visibility (relative units); total | 28.84 (4.64) | 0.59 | 16–37 | |
| Temporal inferior | 6.29 (1.22) | 0.15 | 3–8 | |
| Temporal superior | 5.90 (1.18) | 0.15 | 3–8 | |
| Nasal superior | 3.44 (1.13) | 0.14 | 1–6 | |
| Nasal inferior | 3.27 (0.85) | 0.11 | 2–5 | |
| Temporal horizontal | 1.94 (0.60) | 0.08 | 1–3 | |
| Superior | 2.82 (0.78) | 0.01 | 1–4 | |
| Nasal | 2.08 (0.61) | 0.08 | 1–3 | |
| Inferior | 3.07 (0.81) | 0.10 | 1–4 |
Since in white people, the size, shape, and frequency of α and β zones do not differ significantly between normal eyes and eyes with non-glaucomatous optic nerve atrophy, and assuming that the same is valid for south Indians, evaluation of parapapillary atrophy may also be helpful for the differentiation of glaucomatous versus non-glaucomatous optic nerve damage in south Indian patients.23
Future studies on south Indian patients with glaucoma may reveal whether the correlations between the amount of parapapillary atrophy and the severity of glaucomatous optic nerve damage, the association between parapapillary atrophy and fundus tessellation, the spatial relation between enlargement of parapapillary atrophy outside of the optic disc and loss of neuroretinal rim inside of the optic nerve head, and the differences in the occurrence of parapapillary atrophy between the various types of chronic open angle glaucoma are valid in eyes of south Indian glaucoma patients as they are valid for white patients with glaucoma.15
Diameter of retinal arterioles
In the present study, the retinal arterioles were significantly the widest in the temporal inferior arcade and the temporal superior arcade compared to the nasal superior arcade and nasal inferior arcade (Table 2). The sequence of fundus regions with respect to the width of the retinal arterioles was paralleled by the sequence of fundus sectors concerning the ophthalmoscopic visibility of the retinal nerve fibre layer. Similar findings have already been reported for eyes of white people.10,13
Assuming that in south Indians diffuse and localised narrowing of the retinal arterioles occurs in eyes with optic neuropathies, as has already been published for white patients,9,14 again, the data of the present study may serve as normative data to evaluate the differences in retinal arteriole diameter in south Indian patients with glaucoma versus normal south Indian subjects. As has already been shown for white people,15 the retinal vessel diameters reported in the present study may also serve as relative size units to estimate the optic disc diameter ophthalmoscopically.
Retinal nerve fibre layer
In the normal eyes of this study, the visibility of the retinal nerve fibre layer was regionally unevenly distributed. Dividing the fundus into eight regions, the nerve fibre bundles were most visible in the temporal inferior sector, followed by the temporal superior area in which it was more detectable than in the nasal superior region or the nasal inferior sector (Table 2). The retinal nerve fibre layer was least visible in the superior, inferior, temporal horizontal and nasal horizontal regions (Table 2). The same findings have been reported for white people.24 As already pointed out, in a parallel manner, the diameters of the retinal arterioles were wider at the temporal inferior disc border and the temporal superior disc region than at the nasal superior optic disc border and the nasal inferior disc border (Table 2). It is in agreement with the location of the foveola below a horizontal line drawn through the centre of the optic disc, and with the configuration of the neuroretinal rim that is broadest in the temporal inferior disc sector, followed by the temporal superior disc sector. Physiologically, it points towards an anatomical and nutritional relation between retinal nerve fibre layer, retinal arteriole diameter, neuroretinal rim width, and location of the foveola.
The visibility of the retinal nerve fibre layer decreased marginally significantly with age. It is in agreement with a reduction in the visibility of the retinal nerve fibre layer in white people in whom the regression line between age and retinal nerve fibre layer visibility was almost identical to the equation found for south Indians in the present study.24,25 It correlates with an age related decrease in the optic nerve fibre count with an annual loss of about 4000–5000 fibres/year or 0.3% per year out of an original population of approximately 1.4 million optic nerve fibres as has already been reported for white people.25,26 These features of the normal retinal nerve fibre layer are important for the diagnosis of changes of the retinal nerve fibre layer secondary to optic nerve damage.25
There are limitations of the present study. It has remained unclear if the photographic technique, including the method to correct for the magnification of fundus images, was sufficient to give the optic disc measurements in absolute size units and to make the measurements comparable to data of other studies. Independent of the correctness of the optic disc measurements, however, the determinations of the correlations between disc area, cup area and rim area, and the calculations of the cup/disc ratios remain valid. Another limitation of the study is that the number of subjects is relatively small.
In conclusion, south Indians and white people show a similar optic disc morphology including the correlations between optic disc area and size of the optic cup and neuroretinal rim, the independence of optic cup and rim areas on age, refractive error, and sex, the physiological configuration of the neuroretinal rim with its smallest part in the temporal horizontal disc sector, the regional distribution of the visibility of the retinal nerve fibre layer, the spatial relation between the retinal nerve fibre layer visibility, the retinal arteriole diameter, and the shape of the neuroretinal rim, the age related decrease in the retinal nerve fibre layer visibility, the frequency and size of α and β zones of parapapillary atrophy and their regional distribution, and the regional distribution of the retinal vessel diameters. Future studies examining Indians and white people and using the identical technology such as a confocal laser scanning tomograph of the same brand may address the question whether the optic disc size differs between both population groups. The data presented in this study may be important for the evaluation of the optic nerve head in glaucoma and other optic nerve diseases.
Footnotes
Proprietary interest: none
REFERENCES
- 1.Chi T, Ritch R, Stickler D, et al. Racial differences in optic nerve head parameters. Arch Ophthalmol 1989;107:836–9. [DOI] [PubMed] [Google Scholar]
- 2.Mansour AM. Racial variation of optic disc size. Ophthalmic Res 1991;23:67–72. [DOI] [PubMed] [Google Scholar]
- 3.Tsai CS, Zangwill L, Gonzales C, et al. Ethnic differencs in optic nerve head topography. J Glaucoma 1995;4:248–57. [PubMed] [Google Scholar]
- 4.Varma R, Tielsch JM, Quigley HA, et al. Race-, age-, gender-, and refractive error-related differences in the normal optic disc. Arch Ophthalmol 1994;112:1068–76. [DOI] [PubMed] [Google Scholar]
- 5.Jacob A, Thomas R, Koshi SP, et al. Prevalence of primary glaucoma in an urban south Indian population. Ind J Ophthalmol 1998;46:81–6. [PubMed] [Google Scholar]
- 6.Littmann H. Zur Bestimmung der wahren Gröβe eines Objektes auf dem Hintergrund des lebenden Auges. Klin Monatsbl Augenheilkd 1982;180:286–9. [DOI] [PubMed] [Google Scholar]
- 7.Jonas JB, Fernández MC, Naumann GOH. Glaucomatous parapapillary chorioretinal atrophy:Occurrence and correlations. Arch Ophthalmol 1992;110:214–22. [DOI] [PubMed] [Google Scholar]
- 8.Jonas JB, Schiro D. Normal retinal nerve fibre layer visibility correlated to rim width and vessel caliber. Graefes Arch Clin Exp Ophthalmol 1993;231:207–11. [DOI] [PubMed] [Google Scholar]
- 9.Jonas JB, Gusek GC, Naumann GOH. Optic disc, cup and neuroretinal rim size, configuration, and correlations in normal eyes. Invest Ophthalmol Vis Sci 1988;29:1151–8. Correction: Invest Ophthalmol Vis Sci 1991;32:1893. [PubMed] [Google Scholar]
- 10.Bengtsson B. The variation and covariation of cup and disc diameters. Acta Ophthalmol 1976;54:804–18. [DOI] [PubMed] [Google Scholar]
- 11.Ramrattan RS, Wolfs RCW, Hofmann A, et al. Determinants of optic disk characteristics in a general population. The Rotterdam Study. Ophthalmology 1999;106:1588–96. [DOI] [PubMed] [Google Scholar]
- 12.Ong LS, Mitchell P, Healey PR, et al. Asymmetry in optic disc parameters:the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci 1999;40:849–57. [PubMed] [Google Scholar]
- 13.Meyer T, Howland HC. How large is the optic disc? Systematic errors in fundus cameras and topographers. Ophthalmic Physiol Opt 2001;21:139–50. [DOI] [PubMed] [Google Scholar]
- 14.Jonas JB, Gusek GC, Naumann GOH. Optic disk morphometry in high myopia. Graefes Arch Clin Exp Ophthalmol 1988;226:587–90. [DOI] [PubMed] [Google Scholar]
- 15.Jonas JB, Budde WM, Panda-Jonas S. Ophthalmoscopic evaluation of the optic nerve head. Surv Ophthalmol 1999;43:293–320. [DOI] [PubMed] [Google Scholar]
- 16.Panda-Jonas S, Jonas JB, Jakobczyk M, et al. Retinal photoreceptor count, retinal surface area, and optic disc size in normal human eyes. Ophthalmology 1994;101:519–23. [DOI] [PubMed] [Google Scholar]
- 17.Sekhar GC, Prasad K, Dandona R, et al. Planimetric optic disc parameters in normal eyes: a population based study in South India. Ind J Ophthalmol 2001;49:19–23. [PubMed] [Google Scholar]
- 18.Verteporfin In Photodynamic Therapy Study Group. Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: two-year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization—verteporfin in photodynamic therapy report 2. Am J Ophthalmol 2001;131:541–60. [DOI] [PubMed] [Google Scholar]
- 19.Caprioli J, Miller JM. Optic disc rim area is related to disc size in normal subjects. Arch Ophthalmol 1987;105:1683–5. [DOI] [PubMed] [Google Scholar]
- 20.Jonas JB, Bergua A, Schmitz-Valckenberg P, et al. Ranking of optic disc variables for detection of glaucoma damage. Invest Ophthalmol Vis Sci 2000;41:1764–73. [PubMed] [Google Scholar]
- 21.Jonas JB, Budde WM, Lang P. Neuroretinal rim width ratios in morphologic glaucoma diagnosis. Br J Ophthalmol 1998;82:1366–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tezel G, Kolker AE, Kass MA, et al. Parapapillary chorioretinal atrophy in patients with ocular hypertension. I. An evaluation as a predictive factor for the development of glaucomatous damage. Arch Ophthalmol 1997;115:1503–8. [DOI] [PubMed] [Google Scholar]
- 23.Jonas JB, Fernández MC, Naumann GOH. Parapapillary atrophy and retinal vessel caliber in nonglaucomatous optic nerve damage. Invest Ophthalmol Vis Sci 1991;32:2942–7. [PubMed] [Google Scholar]
- 24.Jonas JB, Schiro D. Normal retinal nerve fibre layer visibility correlated to rim width and vessel caliber. Graefes Arch Clin Exp Ophthalmol 1993;231:207–11. [DOI] [PubMed] [Google Scholar]
- 25.Jonas JB, Dichtl A. Evaluation of the retinal nerve fibre layer. Surv Ophthalmol 1996;40:369–78. [DOI] [PubMed] [Google Scholar]
- 26.Balazsi AG, Rootman J, Drance SM, et al. The effect of age on the nerve fibre population of the human optic nerve. Am J Ophthalmol 1984;97:760–6. [DOI] [PubMed] [Google Scholar]