Abstract
Aim: To assess the distribution and causes of corneal blindness in a population in southern India.
Methods: A total of 11 786 people of all ages from 94 clusters representative of the population of the Indian state of Andhra Pradesh were sampled using a stratified, random, cluster, systematic sampling strategy. These participants underwent a detailed interview and eye examination including measurement of visual acuity with logMAR charts, refraction, slit lamp biomicroscopy, applanation tonometry, gonioscopy, and stereoscopic dilated fundus evaluation. An eye was considered to have corneal blindness if the visual acuity was <20/200 due to a corneal disease.
Results: Of those sampled, 10 293 (87.3%) people participated in the study. Corneal blindness in at least one eye was present in 86 participants, an age, sex, and urban-rural distribution adjusted prevalence of 0.66% (95% confidence interval 0.49 to 0.86), which included 0.10% prevalence of corneal blindness in both eyes and 0.56% in one eye. The most frequent causes of corneal blindness in at least one eye included keratitis during childhood (36.7%), trauma (28.6%), and keratitis during adulthood (17.7%). Nearly 95% of all corneal blindness was avoidable. Multivariate analysis showed that the prevalence of corneal blindness was significantly higher with decreasing socioeconomic status and with increasing age. Of the 99 eyes with corneal blindness, 51 (51.5%) had visual acuity of inaccurate projection of light or no perception of light.
Conclusions: There is a significant burden of corneal blindness in this population, the majority of which is avoidable. Eye health promotion strategies are warranted to raise awareness about the causes and prevention of corneal blindness.
Keywords: corneal blindness, corneal graft, India
We conducted the Andhra Pradesh Eye Disease Study (APEDS) in the state of Andhra Pradesh which is one of the largest states of India with an estimated population of 76 million in 2001.1 The age distribution of the population of the state is pyramidal like the rest of India, with an estimated 35.6% of the total population 15 years of age or less, 25.7% between 16–29 years, and 38.7% 30 years of age or more.2 The rural population comprises approximately 73% of the total population of the state,1 and agriculture is the primary occupation.
The objectives of APEDS were to determine the prevalence and causes of blindness and visual impairment, risk factors associated with major eye diseases, barriers to eye care services, and quality of life in the visually impaired.3–6 Data on blindness (presenting visual acuity <20/200 or central visual field <20 degrees in the better eye) from APEDS have been reported recently.5 The prevalence of blind people in this population was estimated as 1.84%, of which 7% was due to corneal diseases.5
We now report detailed data on blindness due to corneal disease in one or both eyes in this Indian population. These data would help in assessing the complete burden of blindness due to corneal disease, and would assist in planning effective strategies to reduce corneal blindness in this population.
METHODS
Study design
Various aspects of the study design of APEDS have been described previously.3–6 Briefly, a multistage sampling procedure was used to select 24 urban clusters and 70 rural clusters from one urban and three rural areas from different parts of the state, with the aim of having a study sample representative of the urban-rural and socioeconomic distribution of the population of this state. These four areas were located in Hyderabad (urban), West Godavari district (well off rural), and Adilabad and Mahabubnagar districts (poor rural). The sampling strategy for APEDS has been described earlier. APEDS was conducted from October 1996 to February 2000.
The major difference between the urban and rural sample was that the former was selected from blocks stratified by socioeconomic status and religion, whereas the latter were selected from villages stratified by caste (as a surrogate measure for socioeconomic status) as described previously. A total of 94 clusters were selected for APEDS using stratified random sampling, such that the proportion of each socioeconomic status in the sample would be similar to that in the population of the state. These clusters were mapped and the number of households and members in each household listed. Every second to fifth household was systematically selected in each cluster to obtain roughly equal number of households in each cluster. Approximately half the clusters in each of the four areas were randomly assigned to have people of all ages in the selected households eligible for the study, and the other half to have only those 30 years of age or more eligible for the study. This was done to obtain a similar number of people in the less than and more than 30 year old age groups. A total of 11 786 people were sampled in all the four areas of APEDS, of which 8832 were sampled in the three rural areas. Eligible participants were interviewed by trained investigators. These participants were then invited for detailed eye examination at a local clinic that was especially set up for APEDS. Written informed consent was obtained from the participants in the study before the examination. For those participants who could not read and write, the consent was read aloud to them by the receptionist at the examination site in the presence of all the participants on that day. These participants gave their thumb impression after understanding and agreeing with the content of the consent. APEDS was approved by the ethics committee of the LV Prasad Eye Institute, Hyderabad, India.
Clinical examination
The eye examination conducted in APEDS has been described in detail previously.3–6 Briefly, the eye examination included measurement of presenting and best corrected distance and near visual acuities under standardised conditions with logMAR charts,7 external eye examination, assessment of pupillary reaction, anterior segment examination using slit lamp biomicroscope, measurement of intraocular pressure using Goldmann applanation tonometer, gonioscopy, and lens, vitreous, and posterior segment examination (included examination with the indirect ophthalmoscope using 20 dioptre lens and at the slit lamp using 78 dioptre lens) after dilatation unless contraindicated because of risk of angle closure. Automated visual fields were done with the Humphrey visual field analyser8 using the threshold central 24-2 strategy in those participants assessed to have any suspicion of glaucoma, any other optic nerve pathology, higher visual pathway lesion, or significant macular pathology according to uniform predefined criteria. Photographic documentation was done for anterior pathology using the Nikon photo slit lamp (Nikon Corporation, Tokyo, Japan) and for posterior segment pathology using the Zeiss fundus camera (Carl Zeiss, Jena, Germany), which was used to confirm diagnoses.
Portable equipment was used to examine those who where physically debilitated and were unable to come to the clinic. This examination was essentially similar to the one at the clinic except that gonioscopy, posterior segment examination using 78 dioptre lens, automated visual fields, and photography were not done.3–6
Definition and causes of blindness
We have previously reported the data on blind people in this population (presenting visual acuity <20/200 or central visual field <20 degrees in the better eye).5 The cause of blindness was assigned as described previously.4,5 In this report, an eye was considered to have corneal blindness if the visual acuity in that eye was <20/200 as a result of a corneal disease. This determination was initially made by the ophthalmologist examining the study participants at the APEDS clinic, who was trained in the study procedures by the principal investigator (LD), and later confirmed by the principal investigator and co-investigator (RD) using the photographic documentation. If a study participant had more than one ocular pathology, the predominant cause of blindness was discerned based on the clinical examination and review of the photographic documentation. The corneal diseases were defined and classified using predetermined criteria based on history and clinical examination. If there was a doubt regarding the cause of blindness, that particular study participant was re-examined by the principal investigator.
Data management and analysis
Data were entered on self coded forms by the investigators and the examiners which were then entered into a computer by two data entry operators using foxpro software with internal consistency checks.3–6 Data entered by one data entry operator were checked by the other data entry operator after completion of each cluster. This was done randomly on 10% of all the data entered for each cluster. To determine and verify outliers, monthly range and consistency checks were performed using spss (SPSS for Windows, Rel 10.0.5. 1999. SPSS Inc, Chicago, IL, USA). Statistical analyses were done with the spss.
The prevalence of corneal blindness was adjusted for the estimated age, sex, and urban-rural distribution of the population in India for the year 2000,2,9 to obtain composite estimates for the overall prevalence of corneal blindness. The design effect of the sampling strategy was calculated using the prevalence of corneal blindness in each cluster,10 and the 95% confidence intervals (CI) of the estimates were adjusted accordingly by assuming normal approximation of binomial distribution for prevalence of 1% or more, and Poisson distribution11 for prevalence less than 1%.
Data on blindness due to corneal disease were analysed for corneal blindness in both eyes, in one eye, and in at least one eye. The demographic associations of corneal blindness with age, sex, socioeconomic status, and area of residence were assessed with univariate analysis using the χ2 test, followed by multivariate analysis using multiple logistic regression. The effect of each category of a multicategorical risk factor variable was assessed by keeping the first or the last category as the reference.
These data on corneal blindness were extrapolated to the population of Andhra Pradesh and India.2,9 The prevalence of corneal blindness was also estimated for India in the years 2010 and 2020 if the current age-sex specific rates continue, by applying these rates to the estimated age, sex, and urban-rural distribution of the population of India in 2010 and 2020.2,9
RESULTS
Of the eligible 11 786 sampled people, 10 293 (87.3%) participated in the study from the four areas of APEDS. Of these, 7775 (75.3%) were from the three rural areas; 5439 (52.8%) were females, and 122 (1.2%) were examined at home.
Prevalence of corneal blindness
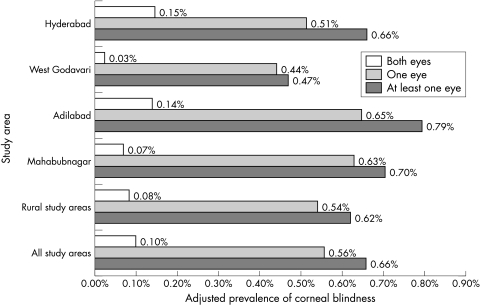
Of the 10 293 participants who were examined, 13 had corneal blindness in both eyes and 73 had corneal blindness in one eye. The prevalence of corneal blindness for the four areas of APEDS combined, adjusted for age, sex, and urban-rural distribution was 0.66% (95% CI 0.49 to 0.86; design effect 1.35) in at least one eye, which included 0.10% prevalence of corneal blindness in both eyes, and 0.56% prevalence of corneal blindness in one eye. The prevalence of corneal blindness in at least one eye was the highest in Adilabad (one of the poor rural areas) and was the lowest in West Godavari (the well off rural area), whereas the prevalence of corneal blindness in both eyes was similar in Hyderabad (the urban area) and Adilabad (poor rural area) as shown in Figure 1.
Figure 1.
Prevalence of corneal blindness in both eyes, one eye, and at least one eye for the four areas of APEDS. Prevalence for all the study areas combined adjusted for age, sex, urban-rural distribution of population of India in 2000,2,9 and for the rest adjusted for age and sex distribution of population of India in 2000.2
Causes of corneal blindness
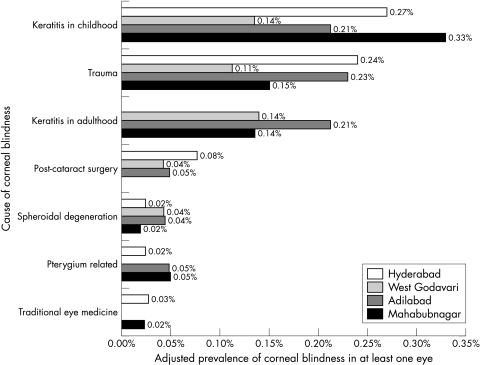
The prevalence of causes of corneal blindness for all areas of APEDS combined is shown in Table 1. All corneal blindness resulting from trauma irrespective of age and sequelae was classified under trauma. Keratitis during childhood and trauma were the leading causes of corneal blindness in at least one eye. The causes of corneal blindness in at least one eye for the four areas are shown in Figure 2. The prevalence of keratitis during childhood was the highest in poor rural Mahabubnagar followed by urban Hyderabad. The prevalence of keratitis during adulthood was the highest in poor rural Adilabad and was not seen in Hyderabad. Corneal scar post trauma was similar in Hyderabad and Adilabad, and higher than the other two areas. Corneal blindness following application of traditional eye medicine was seen only in Hyderabad and Mahabubnagar.
Table 1.
Prevalence of causes of corneal blindness for the four areas of APEDS combined
| Prevalence of corneal blindness (number of participants with corneal blindness) | |||
| Cause of corneal blindness | In both eyes | In one eye | In at least one eye |
| Keratitis in childhood | 0.062% (7) | 0.176% (22) | 0.238% (29) |
| After exanthematous fever | 0.048% (6) | 0.079% (11) | 0.127% (17) |
| After non-exanthematous fever | 0.014% (1) | 0.008% (1) | 0.022% (2) |
| Unknown aetiology | 0 | 0.089% (10) | 0.089% (10) |
| Trauma | 0.009% (1) | 0.176% (21) | 0.185% (22) |
| Keratitis in adulthood | 0.017% (3) | 0.099% (17) | 0.116% (20) |
| Unknown aetiology | 0.003% (1) | 0.099% (17) | 0.102% (18) |
| Post leprosy | 0.014% (2) | 0 | 0.014% (2) |
| Post-cataract surgery | 0 | 0.043% (5) | 0.043% (5) |
| Aphakic bullous keratopathy | 0 | 0.036% (4) | 0.036% (4) |
| Severe astigmatism | 0 | 0.007% (1) | 0.007% (1) |
| Spheriodal degeneration | 0 | 0.032% (4) | 0.032% (4) |
| Pterygium related | 0 | 0.030% (4) | 0.030% (4) |
| Pterygium | 0 | 0.019% (3) | 0.019% (3) |
| Post pterygium surgery | 0 | 0.011% (1) | 0.011% (1) |
| Traditional eye medicine | 0.013% (2) | 0 | 0.013% (2) |
| Total | 0.101% (13) | 0.556% (73) | 0.657% (86) |
Figure 2.
Causes of corneal blindness in at least one eye for the four areas of APEDS. Hyderabad is the urban area and the rest are rural areas of APEDS. Prevalence adjusted for age and sex distribution of population of India in 2000.2
Twenty two of the 86 participants who had corneal blindness in at least one eye had trauma as the cause of blindness. Of these 22 participants, 15 (68.2%) resided in the rural study areas. The distribution of age at trauma, cause, and place of trauma that resulted in corneal blindness is shown in Table 2. The majority of trauma leading to corneal blindness (71.4%) in the urban area occurred at age ≤15 years, whereas 73.3% of this occurred after 15 years of age in the rural areas. Flying or thrown object resulted in most of the trauma leading to corneal blindness in the urban area. In the rural areas vegetable matter (thorns, branches, plant secretion) was the major cause. In the urban area 42.9% of the trauma leading to corneal blindness occurred while playing, and in the rural areas 46.7% occurred at work.
Table 2.
Age at trauma, cause and place of trauma for the participants who had trauma as cause of corneal blindness in at least one eye in APEDS
| Urban area* (n=7) | Rural areas* (n=15) | All study areas combined | |
| Age at trauma (years) | |||
| ≤15 | 5 (71.4%) | 4 (26.7%) | 9 (40.9%) |
| 16–29 | 0 | 4 (26.7%) | 4 (18.2%) |
| 30–39 | 1 (14.3%) | 2 (13.3%) | 3 (13.6%) |
| 40–49 | 1 (14.3%) | 1 (6.7%) | 2 (9.1%) |
| 50–59 | 0 | 3 (20.0%) | 3 (13.6%) |
| 60–69 | 0 | 0 | 0 |
| ≥70 | 0 | 1 (6.7%) | 1 (4.5%) |
| Cause of trauma† | |||
| Flying/thrown object | 4 (57.1%) | 2 (13.3%) | 6 (27.3%) |
| Explosive | 1 (14.3%) | 1 (6.7%) | 2 (9.1%) |
| Vegetable matter | 1 (14.3%) | 5 (33.3%) | 6 (27.3%) |
| Fall | 0 | 1 (6.7%) | 1 (4.5%) |
| Tool | 0 | 1 (6.7%) | 1 (4.5%) |
| Chemical | 1 (14.3%) | 0 | 1 (4.5%) |
| Others | 0 | 4 (26.7%) | 4 (18.2%) |
| Place of trauma† | |||
| At home | 2 (28.6%) | 4 (26.7%) | 6 (27.3%) |
| At work | 2 (28.6%) | 7 (46.7%) | 8 (40.9%) |
| While playing | 3 (42.9%) | 3 (20.0%) | 6 (27.3%) |
*Hyderabad is the urban area, and West Godavari, Adilabad, and Mahabubnagar are rural areas of APEDS.
†Data on cause and place of trauma not available for one participant.
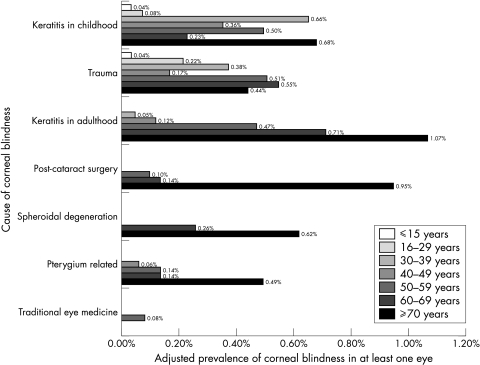
Figure 3 shows the sex and urban-rural distribution adjusted prevalence of the causes of corneal blindness in at least one eye for the different age groups for the four areas of APEDS combined. Corneal scar due to trauma and keratitis in childhood were responsible for a significant proportion of corneal blindness across all age groups. Keratitis and corneal scar post cataract surgery were important causes of corneal blindness for those 50 years of age or more.
Figure 3.
Prevalence of causes of corneal blindness in at least one eye for different age groups for the four areas of APEDS combined. Prevalence adjusted for sex and urban-rural distribution of population of India in 2000.2,9
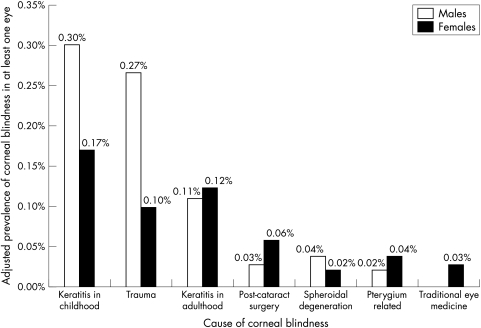
The age and urban-rural adjusted prevalence of the causes of corneal blindness in at least one eye for the two sexes in the four areas of APEDS combined is shown in Figure 4. The adjusted prevalence of corneal blindness in at least one eye for males was 0.77% (95% CI 0.51 to 1.09; design effect 1.26) and for females was 0.54% (95% CI 0.34 to 0.79; design effect 1.21). Corneal blindness due to trauma and to keratitis in childhood was more common in males, and corneal blindness due to traditional eye medicine and post cataract surgery was more common in females.
Figure 4.
Prevalence of causes of corneal blindness in at least one eye for the two sexes for the four areas of APEDS combined. Prevalence adjusted for age and urban-rural distribution of population of India in 2000.2,9
Demographic associations of corneal blindness
The distribution of those with corneal blindness by age, sex, socioeconomic status, and area of residence is shown in Table 3. None of the participants belonging to the upper socioeconomic status (monthly per capita income >US$45) had blindness due to corneal disease. On applying multiple logistic regression (Table 4), the odds of having corneal blindness in one eye or at least one eye increased with increasing age, and were significantly higher for those belonging to extreme lower socioeconomic status compared with the other socioeconomic strata. There were no significant associations of having corneal blindness in one eye or at least one eye with sex and area of residence.
Table 3.
Distribution of corneal blindness in APEDS by age, sex, socioeconomic status, and area of residence
| Corneal blindness | ||||
| Total (n=10293) | Both eyes (n=13) No (%) | One eye (n=73) No (%) | At least one eye (n=86) No (%) | |
| Age group (years)* | ||||
| ≤15 | 2861 | 0 | 2 (0.07%) | 2 (0.07%) |
| 16–29 | 1845 | 1 (0.05%) | 5 (0.27%) | 6 (0.32%) |
| 30–39 | 1863 | 4 (0.21%) | 16 (0.85%) | 20 (1.06%) |
| 40–49 | 1424 | 2 (0.14%) | 8 (0.56%) | 10 (0.70%) |
| 50–59 | 1047 | 4 (0.38%) | 10 (0.95%) | 14 (1.33%) |
| 60–69 | 900 | 1 (0.11%) | 17 (1.89%) | 18 (2.00%) |
| ≥70 | 353 | 1 (0.28%) | 15 (4.25%) | 16 (4.53%) |
| Sex† | ||||
| Male | 4854 | 9 (0.18%) | 39 (0.80%) | 48 (0.98%) |
| Female | 5439 | 4 (0.07%) | 34 (0.62%) | 38 (0.69%) |
| Socioeconomic status‡ | ||||
| Extreme lower | 1354 | 6 (0.44%) | 14 (1.03%) | 20 (1.47%) |
| Lower | 5212 | 5 (0.09%) | 36 (0.69%) | 41 (0.78%) |
| Middle | 3172 | 2 (0.06%) | 21 (0.66%) | 23 (0.72%) |
| Upper | 362 | 0 | 0 | 0 |
| Area of residence§ | ||||
| Hyderabad | 2522 | 5 (0.20%) | 16 (0.63%) | 21 (0.83%) |
| West Godavari | 2503 | 1 (0.04%) | 14 (0.55%) | 15 (0.59%) |
| Adilabad | 2690 | 4 (0.15%) | 17 (0.63%) | 21 (0.78%) |
| Mahabubnagar | 2578 | 3 (0.12%) | 26 (1.00%) | 29 (1.12%) |
*p=0.069 for corneal blindness in both eyes, and p<0.0001 for corneal blindness in one eye and at least one eye; univariate χ2 test.
†p=0.111, 0.282, 0.106 for corneal blindness in both eyes, in one eye and at least one eye, respectively; univariate χ2 test.
‡p=0.006, 0.189, 0.015 for corneal blindness in both eyes, in one eye and at least one eye, respectively; univariate χ2 test. Socioeconomic status defined according to monthly per capita income in Indian rupees: extreme lower ≤200 (US$4.5), lower 201–500, middle 501–2000, and upper >2000. Data on socioeconomic status not available for 193 participants.
§p=0.450, 0.212, 0.222 for corneal blindness in both eyes, in one eye and at least one eye, respectively; univariate χ2 test. Hyderabad is urban area, West Godavari is relatively well off rural area, and Adilabad and Mahabubnagar are poor rural areas.
Table 4.
Association of corneal blindness in APEDS with age, sex, socioeconomic status, and area of residence with multiple logistic regression
| Odds of having corneal blindness with multiple logistic regression (95% CI) | ||
| In one eye | In at least one eye | |
| Age group (years) | ||
| ≤15 | 1.00 | 1.00 |
| 16–29 | 4.02 (0.78 to 20.65) | 4.90 (0.99 to 24.23) |
| 30–39 | 12.98 (3.00 to 56.31) | 16.65 (3.90 to 71.08) |
| 40–49 | 8.53 (1.81 to 40.14) | 11.01 (2.41 to 50.17) |
| 50–59 | 12.84 (2.78 to 59.37) | 19.13 (4.32 to 84.65) |
| 60–69 | 27.82 (6.44 to 120.26) | 30.38 (7.06 to 130.73) |
| ≥70 | 61.05 (13.83 to 269.56) | 67.48 (15.38 to 296.08) |
| Sex | ||
| Male | 1.00 | 1.00 |
| Female | 0.80 (0.50 to 1.29) | 0.71 (0.46 to 1.10) |
| Socioeconomic status* | ||
| Others | 1.00 | 1.00 |
| Extreme lower | 1.90 (1.04 to 3.45) | 2.45 (1.46 to 4.11) |
| Area of residence† | ||
| Hyderabad | 1.00 | 1.00 |
| West Godavari | 0.79 (0.38 to 1.62) | 0.63 (0.32 to 1.23) |
| Adilabad | 0.98 (0.49 to 1.99) | 0.90 (0.48 to 1.69) |
| Mahabubnagar | 1.44 (0.77 to 2.73) | 1.24 (0.70 to 2.20) |
*Socioeconomic status defined according to monthly per capita income in Indian rupees: extreme lower ≤200 (US$4.5) and others >200.
†Hyderabad is urban area, West Godavari is relatively well off rural area, and Adilabad and Mahabubnagar are poor rural areas.
Visual acuity distribution
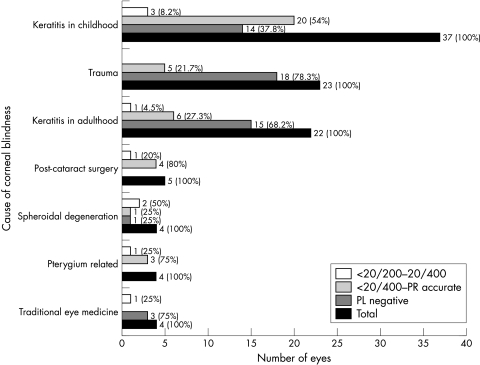
A total of 99 eyes suffered from corneal blindness, which includes 26 eyes of 13 participants who had corneal blindness in both eyes, and 73 eyes of 73 participants who had corneal blindness in one eye. Of these 99 eyes, nine (9.1%) had presenting visual acuity of <20/200–20/400, 39 (39.4%) had <20/400 to accurate projection of light, and 51 (51.5%) had inaccurate projection of light or no light perception. Of the 13 participants with corneal blindness in both eyes, five (38.5%) had visual acuity of inaccurate projection of light or no light perception in both the eyes.
Figure 5 shows the distribution of visual acuity in 99 eyes of 86 participants with corneal blindness based on the cause of blindness. The majority of eyes with corneal blindness caused by trauma, keratitis during adulthood, and traditional eye medicine had inaccurate projection of light or no perception of light. For corneal blindness caused by keratitis during childhood, cataract surgery, and pterygium related, the highest proportion of eyes had visual acuity <20/400 to accurate projection of light.
Figure 5.
Distribution of visual acuity in 99 eyes of 86 participants with corneal blindness based on the cause of blindness. Total represents all eyes blind due to corneal disease (<20/200), and PL negative includes eyes with inaccurate projection of light and no perception of light.
Extrapolations to the population
Extrapolating these data from APEDS to the estimated 76 million population of Andhra Pradesh in the year 2001, 50 160 (95% CI 37 724 to 65 360) people have corneal blindness in at least one eye, of whom approximately 7600 have corneal blindness in both eyes.
If these data are extrapolated to the 1027 million population of India in the year 2001,1 6.8 (95% CI 5.0 to 8.8) million people are estimated to have corneal blindness in at least one eye, of whom one million people have corneal blindness in both eyes. If the current age-sex specific rates of corneal blindness continue, the prevalence in India in the years 2010 and 2020 for corneal blindness in at least one eye would be 0.72% (95% CI 0.54 to 0.93) and 0.81% (95% CI 0.63 to 1.04), respectively. These rates suggest that 8.4 (95% CI 6.3 to 10.9) million people of the estimated 1168 million population of India in 2010,2 and 10.6 (95% CI 8.3 to 13.6) million people of the estimated 1312 million population of India in 2020,2 would have corneal blindness in at least one eye if the current trend continues.
DISCUSSION
The external location of cornea predisposes it to a variety of sight threatening insults. Diseases affecting the cornea are a major cause of blindness worldwide.12 The major causes of corneal blindness globally include trachoma, corneal ulceration, xerophthalmia, ophthalmia neonatorum, traditional eye medicines, onchocerciasis, leprosy, and ocular trauma.13 We provide detailed population based data on corneal blindness in an Indian population that could assist in developing strategies to reduce this blindness.
Prevalence and demographic associations of corneal blindness
These population based data on the magnitude and causes of corneal blindness suggest that 0.66% of this Indian population suffers from corneal blindness in at least one eye. This translates into one out of every 150 people in this population, resulting in a significant burden of corneal blindness. There was a regional variation in the prevalence of corneal blindness. The prevalence of corneal blindness was not very different between the urban and the two poor rural areas of APEDS but was lower in West Godavari, the well off rural area. The major difference between West Godavari and other three areas was the lower prevalence of corneal blindness during childhood. It is possible that this low prevalence is due to the better socioeconomic status in this area that has led to better nutrition and, thereby, reduced prevalence of vitamin A deficiency associated with exanthematous fever. Hyderabad, the urban area, had a high prevalence of corneal blindness, particularly corneal blindness in both eyes. We have previously reported that the reason for this could be that many of those from the rural areas with corneal blindness in both eyes have migrated to urban areas to earn a livelihood by begging because corneal scar is easily visible to the others, and hence it is easy to arouse sympathy in others while begging for money.4,5
The odds of suffering from corneal blindness increased with increase in age, and were higher for those belonging to the extreme lower socioeconomic status. We have reported a similar trend for blindness and moderate visual impairment due to any cause in this population.4–6 A higher prevalence of blindness in those with lower socioeconomic status has been reported from many different parts of the world.14 Our data further highlight the disadvantaged position of those belonging to the extreme lower socioeconomic status in our society—either in terms of predisposition to these corneal diseases or accessibility and affordability of treatment for the corneal diseases leading to blindness.
Causes of corneal blindness
Keratitis during childhood was the leading cause of corneal blindness in our population. Vitamin A deficiency precipitates in malnourished children who get debilitating fever, which can lead to blindness due to xerophthalmia. Males were more likely to be blind after exanthematous fever during childhood compared with females. The reason for this is not clear but it could be that the chances of a malnourished female child dying following vitamin A deficiency are higher compared with their male counterpart, and hence a lower number of females are currently blind because of exanthematous fever during childhood. On considering the age distribution of participants suffering from corneal blindness after fever during childhood, 5.3% were between 16 and 29 years, 52.6% between 30 and 49 years, and 42.1% were 50 years of age or more. Based on these data, it may not be unreasonable to assume that there has probably been an improvement in the vitamin A status of this population over the years. Even though we did not find any child with corneal blindness after fever, it has to be seen in the background of the relatively small sample size of children in APEDS.
Trauma was the second major cause of corneal blindness in our population. Trauma has been reported to be one of the most important causes of unilateral vision loss in developing countries.15 Males have been reported to have a higher chance of suffering ocular trauma compared with females.16–20 In our population, males were three times more likely to have corneal blindness in at least one eye due to trauma compared with females. We have also previously reported from the urban area that males were more likely to suffer from blindness following ocular trauma.16 This predisposition of males to ocular trauma is likely to be related to their lifestyle or occupation.
Workplace accounted for 40% of the corneal blindness caused by trauma in our population. Six (66.7%) of those who had trauma in the workplace were working in farms, and were not wearing any protection while at work. In a study from Australia, 60% of the trauma was reported at the workplace.17 The majority of trauma occurred before 40 years of age in our population. This is of significance as the large number of years that these people live with blindness in one or both eyes could have a range of social and economic consequences.
Corneal scar following keratitis during adulthood was the next common cause of corneal blindness in our population, especially in those 50 years of age or more. A hospital based study from southern India has reported that corneal scarring was the most common indication for penetrating keratoplasty, half of which was due to keratitis.21 Recently, corneal ulceration has also been recognised as a “silent epidemic” in developing countries.22 The incidence of corneal ulceration from Nepal23 has been reported to be seven times more than that reported from southern India,24 and 70 times more than that reported from the United States.25 Treatment of a corneal scar following infection has its own limitations. A corneal transplant is not very successful, and the antibiotics and antifungal treatment are relatively costly for developing countries.26,27
Corneal blindness related to cataract surgery, mostly due to aphakic bullous keratopathy, was not uncommon in this population. Females were more likely to have corneal blindness in at least one eye because of cataract surgery related causes. We have previously reported from the urban area that females had a 2.5 times higher risk of having an adverse outcome after cataract surgery (presenting visual acuity <20/60).28 A higher chance of poor visual outcome after cataract surgery in females has also been reported from the Indian state of Rajasthan.29 The reasons for this could be the disadvantaged position of females in our society which results in poor quality of eye care services being available to them.14
Role of corneal grafting
Some of those who are currently suffering from corneal blindness can be visually rehabilitated by corneal grafting. Corneal grafting is a clinical decision made by a trained corneal surgeon based on a variety of parameters, including visual acuity. According to the visual acuity distribution of the eyes with corneal blindness in this population, a little less than half of the eyes had visual acuity <20/200 to accurate projection of light, which theoretically could potentially benefit from corneal grafting. However, the success of corneal grafting in restoring vision depends on a complex set of factors in a developing country setting. Service delivery of corneal grafting involves four major issues. Firstly, only well trained corneal surgeons with well equipped clinical facilities for proper surgery, long term follow up, and treatment of graft rejections and other postoperative complications that might occur, can successfully perform corneal grafting.22,27 Secondly, the appropriateness of the selection of a candidate for corneal grafting is important as the outcome depends on the pathology responsible for corneal blindness as indicated in the reports from India and elsewhere.26,27,30,31 Hospital based data on survival of corneal grafts done at a reputed eye institute in India showed that the 5 year survival rate for corneal transplants performed for the first time was 46.5% for all pathologies causing corneal blindness considered together, with some causes having particularly dismal 5 year survival rates, 31.5% for adherent leucomas, and 21.5% for aphakic bullous keratopathy.26 In addition, the patients belonging to a lower socioeconomic status had 28% higher risk of corneal graft failure, and also had a 2.5 times higher chance of infection causing graft failure.26,32 In our study population, 73.7% of all participants with visual acuity <20/200 to accurate projection of light belonged to the extreme lower or lower socioeconomic strata. The third major issue is availability of adequate number of good quality donor corneas for corneal grafting from reliable eye bank facilities. Significant developments in this area have been made in India by the Eye Bank Association of India which is a national level non-governmental organisation involved in increasing the collection of donor corneas, testing and distribution of quality donor corneas, and setting standards of eye banking in India.33 The fourth issue is that the surgical costs of treating corneal blindness are generally higher than the majority of population in a developing country can afford, because of issues like the therapeutic costs, the long duration of treatment involving frequent follow up, time lost from work, and various other indirect costs.
The issues discussed above indicate that although corneal grafting can be of use to some people with corneal blindness in a developing country setting, it is not a viable option for a large proportion of those with corneal blindness because many eyes with corneal blindness are not eligible for corneal grafting, it requires very specialised skills, it generally has a poor success rate, and it is very costly.
Need for health promotion strategies
Of the 0.66% prevalence of corneal blindness in at least one eye in our population, nearly 95% of this blindness was avoidable. The avoidable causes of corneal blindness include keratitis in childhood, trauma, aphakic bullous keratopathy, and severe astigmatism post cataract surgery, keratitis in adulthood, traditional eye medicines, and corneal scar post pterygium surgery.
In the background of the fact that most of the corneal blindness is avoidable, and surgical intervention for treating corneal blindness is a difficult option in a developing country setting, the need for decreasing corneal blindness in the long term with effective health promotion strategies is clearly highlighted by these data on corneal blindness. Prevention is obviously more cost effective in the long term as demonstrated by success stories from some parts of the world in reducing corneal blindness due to vitamin A deficiency, onchocerciasis, and leprosy.13,34
Health promotion programmes to reduce corneal blindness need to target those who are identified to be at a higher risk of suffering from corneal blindness, based on the epidemiological data. In order for these programmes to have an impact, the government, non-governmental organisations, eye health professionals including the ophthalmologists, and the community have to be involved, and these programmes need to be integrated with the other relevant health and safety programmes. These health promotion programmes should focus on increasing awareness about the risk and consequences of corneal blindness, possible safety and prevention procedures to be followed to reduce the risk of corneal blindness, and the benefit of early detection and treatment if the need arises.
The major causes of corneal blindness based on our data that need attention in these programmes are keratitis during childhood, trauma and keratitis during adulthood. The possible targets for these programmes are children and young adults, especially males, and a focus on work related trauma.
Attempts should be made to integrate the health promotion programmes with the school health programmes and the child survival and safe motherhood programme of the Department of Health and Family Welfare, Government of India, which have control of blindness in children as one of the objectives through universal immunisation and improving vitamin A status.35 This would also result in involvement of parents and teachers in the initiatives for prevention of corneal blindness allowing the programme to reach the primary healthcare level in the community.
Safety in workplaces has to be improved to reduce trauma causing corneal blindness. Requirements for appropriate eye protection for people performing high risk work can reduce risk of corneal blindness. Attempts would have to be made for legislation promoting safety in workplaces. There are data suggesting a decrease in eye injuries with increased use of eye protection in the workplace, but the use of eye protection is not universal.36 Health promotion programmes would need to encourage compliance with the use of eye protection at work in addition to legislation for safety at work. This kind of programme would have to involve the community on a large scale, as much of the workforce in our country is informal.37
These data also suggest that the quality of cataract surgery has to be reasonable to reduce corneal blindness caused by poor quality cataract surgery. The awareness of the need for good quality cataract surgery should be improved in the eye care personnel, particularly ophthalmologists.38 In addition, to reduce corneal blindness caused by keratitis, the ophthalmologists should be aware of the appropriate treatment of corneal ulcers and should know when and where to refer the patient with corneal ulcer for further management.
In conclusion, there is a significant burden of corneal blindness in this Indian population, encompassing a variety of corneal infections and trauma, the majority of which are avoidable. Health promotion strategies have to be developed and implemented to raise awareness about the causes and prevention of corneal blindness. Prevention through health promotion is clearly the preferred long term option to deal with corneal blindness in India.
Acknowledgments
The authors acknowledge M Srinivas, Partha Mandal, Ashok Nanda, Rohit Khanna, Prashant Sahare, and S Narsiah for clinical examination of APEDS participants, P Giridhar, MN Prasad, K Vilas, and VN Naidu for interviewing the APEDS participants, B Srinivas and M Srikanth for data entry, N Rishita for assistance with statistical analysis, GN Rao for encouraging APEDS, and Catherine A McCarty and Hugh R Taylor for guidance in APEDS design.
Financial support for the Andhra Pradesh Eye Disease Study was provided by the Hyderabad Eye Research Foundation, Hyderabad, India, and Christoffel-Blindenmission, Bensheim, Germany. Dr Rakhi Dandona was supported in part by the RB McComas and Hugh Noel Puckle scholarships from the University of Melbourne, Melbourne, Australia.
References
- 1.Registrar General of India. Provisional population totals: India, census of India 2001. New Delhi: Ministry of Home Affairs, Government of India, 2001. http://www.censusindia.net (accessed December 2001).
- 2.US Census Bureau. International database. http://www.census.gov (accessed December 2000).
- 3.Dandona R, Dandona L, Naduvilath TJ, et al. Design of a population-based study of visual impairment in India: the Andhra Pradesh Eye Disease Study. Indian J Ophthalmol 1997;45:251–7. [PubMed] [Google Scholar]
- 4.Dandona L, Dandona R, Naduvilath TJ, et al. Is current eye-care-policy focus almost exclusively on cataract adequate to deal with blindness in India? Lancet 1998;351:1312–6. [DOI] [PubMed] [Google Scholar]
- 5.Dandona L, Dandona R, Srinivas M, et al. Blindness in the Indian state of Andhra Pradesh. Invest Ophthalmol Vis Sci 2001;42:908–16. [PubMed] [Google Scholar]
- 6.Dandona R, Dandona L, Srinivas M, et al. Moderate visual impairment in India: the Andhra Pradesh Eye Disease Study. Br J Ophthalmol 2002;86:373–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferris FL III, Kassoff A, Bresnick GH, et al. New visual acuity charts for clinical research. Am J Ophthalmol 1982;94:91–6. [PubMed] [Google Scholar]
- 8.Humphrey Field Analyzer II User’s Guide. San Leandro: Humphrey Instruments Inc, 1994.
- 9.United Nations. World urbanization prospectus. New York: United Nations, 1998.
- 10.Bennett S, Woods T, Liyanage WM, et al. A simplified general method for cluster-sample surveys of health in developing countries. Wld Hlth Statist Quart 1991;44:98–106. [PubMed] [Google Scholar]
- 11.Rosner B. Fundamentals of Biostatistics. 2nd ed. Boston: PWS Publishers; 1986:84–92, 302–68, 404–8.
- 12.Thylefors B, Negrel AD, Pararajasegaram R, et al. Global data on blindness. Bull World Health Organ 1995;73:115–21. [PMC free article] [PubMed] [Google Scholar]
- 13.Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ 2001;79:214–21. [PMC free article] [PubMed] [Google Scholar]
- 14.Dandona R, Dandona L. Socioeconomic status and blindness. Br J Ophthalmol 2001;85:1484–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thylefors B. Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol 1992;20:95–8. [DOI] [PubMed] [Google Scholar]
- 16.Dandona L, Dandona R, Srinivas M, et al. Ocular trauma in an urban population in southern India: the Andhra Pradesh Eye Disease Study. Clin Exp Ophthalmol 2000;28:350–6. [DOI] [PubMed] [Google Scholar]
- 17.McCarty CA, Fu CLH, Taylor HR. Epidemiology of ocular trauma in Australia. Ophthalmology 1999;106:1847–52. [DOI] [PubMed] [Google Scholar]
- 18.Wong TY, Tielsch JM. A population-based study on incidence eof severe ocular trauma in Singapore. Am J Ophthalmol 1999;128:345–51. [DOI] [PubMed] [Google Scholar]
- 19.Katz J, Tielsch JM, Vitale S, et al. Lifetime prevalence of ocular injuries from the Baltimore Eye Survey. Arch Ophthalmol 1993;111:1564–8. [DOI] [PubMed] [Google Scholar]
- 20.Tielsch JM. Frequency and consequences of ocular trauma: a population perspective. Ophthalmol Clin N Am 1995;8:559–67. [Google Scholar]
- 21.Dandona L, Ragu K, Janarthanan M, et al. Indications for penetrating keratoplasty in India. Indian J Ophthalmol 1997;45:163–8. [PubMed] [Google Scholar]
- 22.Whitcher JP, Srinivasan M. Corneal ulceration in the developing world—a silent epidemic. Br J Ophthalmol 1997;81:622–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Upadhyay MP, Karmacharya PC, Koirala S, et al. The Bhakatpur Eye Study: ocular trauma and antibiotic prophylaxis for the prevention of corneal ulceration in Nepal. Br J Ophthalmol 2001;85:388–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gonzales CA, Srinivasan M, Whitcher JP, et al. Incidence of corneal ulceration in Madurai district, south India. Ophthalmic Epidemiol 1996;3:159–66. [DOI] [PubMed] [Google Scholar]
- 25.Erie JC, Nevitt MP, Hodge DO, et al. Incidence of ulcerative keratitis in a defined population from 1950 through 1958. Arch Ophthalmol 1993;111:1665–71. [DOI] [PubMed] [Google Scholar]
- 26.Dandona L, Naduvilath TJ, Janarthanan M, et al. Survival analysis and visual outcome in a large series of corneal transplants in India. Br J Ophthalmol 1997;81:726–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yorston D, Wood M, Foster A. Penetrating keratoplasty in Africa: graft survival and visual outcome. Br J Ophthalmol 1996;80:890–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dandona L, Dandona R, Naduvilath TJ, et al. Population-based assessment of the outcome of cataract surgery in an urban population in southern India. Am J Ophthalmol 1999;127:650–8. [DOI] [PubMed] [Google Scholar]
- 29.Murthy GVS, Ellwein L, Gupta S, et al. A population-based eye survey of older adults in a rural district of Rajasthan: outcomes of cataract surgery. Ophthalmology 2001;108:686–92. [DOI] [PubMed] [Google Scholar]
- 30.Price FW, Whitson WE, Marks RG. Graft survival in four common groups of patients undergoing penetrating keratoplasty. Ophthalmology 1991;98:322–8. [DOI] [PubMed] [Google Scholar]
- 31.Price FW, Whitson WE, Collins KS, et al. Five-year corneal graft survival: large, single-centre patient cohort. Arch Ophthalmol 1993;111:799–805. [DOI] [PubMed] [Google Scholar]
- 32.Dandona L, Naduvilath TJ, Janarthanan M, et al. Causes of graft failure in India. Indian J Ophthalmol 1998;46:149–52. [PubMed] [Google Scholar]
- 33.The Eye Bank Association of India. About us. http://www.ebai.org (accessed December 2001).
- 34.World Health Organization. Global initiative for the elimination of avoidable blindness. (WHO/PBL/97.61). Geneva: WHO, 1997.
- 35.The Ministry of Health and Family Welfare, Government of India. Aided Projects. http://mohfw.nic.in (accessed December 2001).
- 36.McCormack P. Penetrating injury of the eye [editorial]. Br J Ophthalmol 1999;83:1101–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Planning Commission of India, Government of India. 9th Five-year plan. Human and social development. http://planningcommission.nic.in/fiveyr (accessed April 2002).
- 38.Dandona R, Dandona L. Review of findings of the Andhra Pradesh Eye Disease Study: policy implications for eye-care services. Indian J Ophthalmol 2001;49:215–34. [PubMed] [Google Scholar]