Abstract
Aim: To describe the methods used and initial results of a prospective study designed to determine whether screening and prophylactic treatment will reduce the incidence of primary angle closure glaucoma (PACG) in Mongolia.
Methods: A total of 4725 individuals aged 50 years and above were recruited to the study and randomised to intervention or control groups. All subjects had non-mydriatic optic disc examination. The intervention arm had measurement of anterior chamber depth (ACD) by A-scan ultrasound and intraocular pressure (IOP) with Tonopen. Gonioscopy was performed on test positive cases (ACD <2.53 mm or IOP ≥24 mm Hg either eye). Those with occludable angles were offered laser iridotomy. Primary outcome will be incidence of PACG at 5 year follow up.
Results: Glaucoma was diagnosed in 128 (2.7%) subjects. Of the remaining 4597, 2293 were randomised to intervention. Intervention as allocated was received by 2280 (99.4%) individuals. 160 (23.4%) of 685 test positive cases had occludable angles, of which 156 were treated with iridotomy.
Conclusions: This trial is a further step in determining whether screening and prophylactic treatment for primary angle closure in east Asian populations will reduce the incidence of glaucoma.
Keywords: screening, primary angle closure glaucoma
In populations of east Asia primary angle closure glaucoma (PACG) is a significant cause of visual morbidity.1,2 Treatment with laser peripheral iridotomy in the early stages of primary angle closure appears to control disease progression.3,4
A-mode ultrasound measurement of the axial anterior chamber depth (ACD) has been suggested as a screening tool for primary angle closure5 and is effective in the early detection of gonioscopically occludable angles in the population of Mongolia.6 The equipment required is portable and easy to use by non-medical personnel. Thus, it fulfils some of the requirements for a screening test7 that can be used in the community.
This paper describes the methodology of a randomised controlled trial designed to determine whether screening and prophylactic treatment with laser iridotomy of an adult population of Mongolia can reduce the incidence of glaucomatous optic neuropathy.
MATERIALS AND METHODS
Ethical approval for this study was given by the Ministry of Health, Ulaanbaatar, Mongolia. Subjects aged 50 years and older from in and around the town of Bayanhongor in south west Mongolia and from three districts of Ulaanbaatar city were invited to attend the trial centres. People with an established or suspected diagnosis of glaucoma were excluded from the study, as were those not permanently resident in the selected study areas.
Informed written consent was obtained from all individuals recruited to the study. A polaroid photograph of each study participant was taken to aid future identification. Subjects were randomised to intervention or control arms of the trial using a computer generated allocation schedule and sealed envelopes that had been prepared in London. Following randomisation all subjects underwent an optic disc assessment by direct ophthalmoscopy (Vista 20 ophthalmoscope, Keeler LTD, Berks, UK) with reference to standard photographs. If a disc was judged glaucomatous (see diagnostic criteria) a 56 point threshold visual field test was carried out (Henson CFA 3000, Tinsley Medical Instruments, Newbury, Berks, UK). In cases of uncertainty a second ophthalmologist would assess the optic disc using slit lamp biomicroscopy. Optic discs of both eyes of all subjects were photographed using a non-mydriatic fundus camera (Canon CR4-45NM, Japan). Subjects in either control or intervention groups with glaucomatous optic discs underwent a full slit lamp examination.
Subjects randomised to the intervention group underwent screening. Axial anterior chamber depth (ACD) measurements were taken on right and left eyes using the A-scan mode of an ultrasound biometer (Allergan-Humphrey model 820, Allergan, London, UK). Intraocular pressure (IOP) was measured with a Tonopen (Mentor Ophthalmics, MA, USA). Subjects in the intervention group who screened positive (ACD <2.53 mm or IOP ≥24 mm Hg), or who had glaucomatous optic discs and visual fields, received a more detailed assessment including gonioscopy. The drainage angle was examined with a two mirror Goldmann gonioscopy lens and graded as open or occludable. Individuals with occludable angles were offered bilateral laser iridotomies using a portable YAG laser (Visulas II, Carl Zeiss Ltd, Germany). Subjects with primary open angle glaucoma, ocular hypertension, or advanced PACG were managed on an individual basis.
All individuals recruited to the trial will be examined 5 years after entry into the study. Optic disc and visual field data from the baseline examination will be compared with findings on follow up examination to determine and compare the incidence of PACG in the control and intervention arms.
Outcome measures and sample size calculation
The primary outcome in this study is the number of incident cases of PACG in each study group at 5 years from entry into the trial, which will be calculated using “intent to treat analysis.” A target sample size of 5000 was calculated to have 85% power of detecting a 70% reduction of 5 year incidence of PACG in the intervention arm. The 5 year incidence of PACG was estimated as 1.4% (95% confidence interval (CI) 0.68% to 2.1%) using age specific prevalence data from the Mongolian glaucoma surveys6,8 with methods described by Leske.9 The sample size allows for a loss to follow up of at least one third of the recruited population.
Calculation of test cut-off values
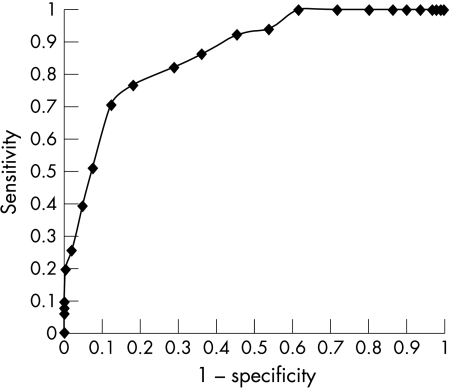
A receiver operator characteristic (ROC) curve demonstrates the performance of slit lamp mounted ultrasound ACD measurements at detecting occludable angles (Fig 1) in the Mongolian population aged 50 and above with a prevalence of occludable angles of 10.1%.6 A cut off of <2.53 mm yielded a sensitivity of 77% (95% CI 65 to 88) and specificity of 83% (95% CI 80 to 86) with a positive predictive value of 32% (Trupepistat computer package, Epistat services, Richardson, TX, USA). The cut off for Tonopen IOP was set at 24 mm Hg. This was based on the mean plus 2 SD of IOP measured with Tonopen of a random sample of 769 Mongolians aged 40 years and above (mean IOP 14.8 (SD 4.4) mm Hg).
Figure 1.
Receiver operator characteristics curve demonstrating performance of slit lamp mounted US anterior chamber depth measurement at detecting occludable angles in the population aged 50 years and over.
Diagnostic criteria
An occludable angle was defined as one in which <90° of the posterior pigmented trabecular meshwork was visible on viewing with a Goldmann two mirror gonioscopy lens in the primary position of gaze without corneal indentation. Glaucoma was defined for the purposes of this study as the presence of glaucomatous optic neuropathy (vertical cup-disc ratio (vCDR) ≥0.7, asymmetry ≥0.2 or neuroretinal rim width ≤0.1 CDR). In cases of early structural damage (0.7 vCDR or 0.2 asymmetry) a reproducible visual field defect was required to confirm the diagnosis. In cases of advanced damage (≥0.8 vCDR or ≥0.3 asymmetry) an associated glaucomatous visual field defect was not an absolute requirement to make the diagnosis. These diagnostic criteria are based on a recently described classification of glaucoma for use in epidemiological studies.10 PACG was diagnosed in cases where there was evidence of glaucomatous optic neuropathy in the presence of an occludable angle.
RESULTS
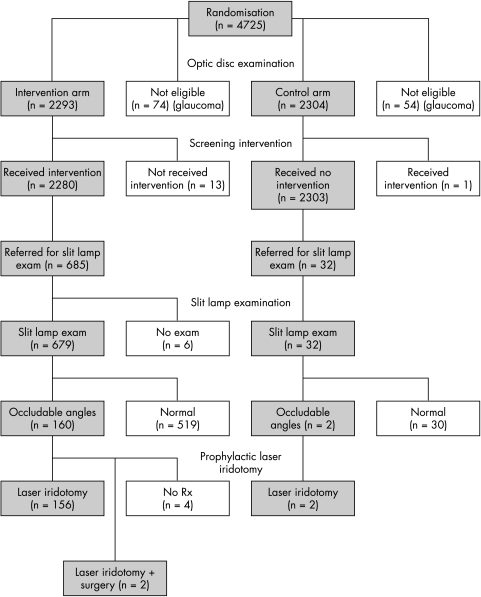
A total of 4725 subjects were recruited to the trial. The flow of participants through the study is shown in Figure 2. At optic disc examination 171 subjects were judged to have disc abnormalities and visual field analysis warranting further examination. Following slit lamp examination 128 of these 171 were excluded from continuing in the trial owing to a diagnosis of glaucoma (50 PACG, 75 POAG, three secondary glaucoma). A total of 4597 subjects were eligible for the study, of which 2293 individuals were randomised to intervention and 2304 to the control group. There was no significant difference in the age (p=0.89, two sided t test) or sex (χ2 = 1.13, p=0.29) distribution between the two groups (Table 1).
Figure 2.
Trial profile.
Table 1.
Age and sex distribution of trial participants
| Age | Male | Female | Total |
| Intervention group | |||
| 49–59 | 334 (14.6%) | 693 (30.2%) | 1027 (44.8%) |
| 60–69 | 320 (13.9%) | 432 (18.8%) | 752 (32.8%) |
| 70–79 | 168 (7.3%) | 241 (10.5%) | 409 (17.8%) |
| 80+ | 45 (1.9%) | 60 (2.6%) | 105 (4.6%) |
| Total | 867 (37.8%) | 1426 (62.2%) | 2293 (100%) |
| Control group | |||
| 49–59 | 377 (16.3%) | 679 (29.5%) | 1056 (45.8%) |
| 60–69 | 296 (12.8%) | 423 (18.3%) | 719 (31.2%) |
| 70–79 | 194 (8.4%) | 237 (10.3%) | 431 (18.7%) |
| 80+ | 40 (1.7%) | 58 (2.5%) | 98 (4.3%) |
| Total | 907 (39.4%) | 1397 (60.65) | 2304 (100%) |
No significant difference in mean age of intervention (mean 62.3 years, SD 9.29) and control groups (mean 62.3 years, SD 9.38) (p=0.89, two sided t test).
No significant difference in distribution of sex between intervention and control groups (χ2 = 1.13, p=0.29).
Slit lamp examination was advised in 685 subjects from the intervention group following screening, and 32 from the control group (Table 2). All apart from two of those requiring slit lamp examination from the control group, had optic discs thought to be glaucomatous on direct ophthalmoscopy but equivocal or unreliable visual fields. Occludable angles were found in 162 cases at slit lamp examination, of which 62 (38.3%) also had evidence of primary angle closure (PAS, irregular pigmentation of the trabecular meshwork or elevated IOP). Of these 162 subjects, 158 proceeded to have laser peripheral iridotomy and four refused treatment.
Table 2.
Indication for slit lamp examination after optic disc examination plus or minus screening and number of occludable angles detected
| Indication for referral | Test +ve Intervention group (n=685) | True +ve* Intervention group (n=160) | Test +ve Control group (n=32) | True +ve* Control group (n=2) | Total true +ve* (n=162) |
| ACD | 613 | 149 | 0 | 0 | 149 |
| ACD + IOP | 31 | 10 | 0 | 0 | 10 |
| IOP | 25 | 1 | 1 | 0 | 1 |
| CDR | 15 | 0 | 28 | 0 | 0 |
| Other | 1 | 0 | 3 | 2 | 2 |
*True +ve = gonioscopically occludable angle; ACD = anterior chamber depth <2.53 mm; ACD + IOP = anterior chamber depth <2.53 mm and intraocular pressure >24 mm Hg; IOP = IOP >24 mm Hg; CDR = cup disc ratio ≥0.7 or asymmetry ≥0.2.
Optic disc evaluation and photography were not possible in either eye of 24 (0.5%) subjects. A total of 275 (6%) cases had no disc photograph in one eye. Interobserver agreement for measurement of the cup-disc ratio between slit lamp biomicroscopy (WN) and direct ophthalmoscopy (SG and AU) was good (weighted κ = 0.67 and 0.73).
DISCUSSION
To our knowledge this randomised controlled trial of screening is the first of its kind in aiming to reduce the incidence of PACG. The advantage of using the ultrasound A-scan method of ACD measurement as a screening tool is that it is easy to use and interpret by non-medical personnel. Slit lamp optics are not required for this test but the stability of a mounted probe may improve precision when compared with a hand held method.6 A portable, tabletop mounted chin and forehead rest with a joystick guided tonometer mount for the ultrasound probe obviates the need for a slit lamp.
By performing direct ophthalmoscopy and photography of the optic disc we have been able to document the status of the optic nerve in the majority of subjects at baseline. A limitation of the study is that examination and photography of optic discs is done through undilated pupils. Dilated funduscopy would allow a more accurate assessment of the cup-disc ratio (CDR) but is more uncomfortable for the subject and carries the small theoretical risk of precipitating an attack of angle closure in this population. There are limitations to the use of the vertical CDR in our diagnostic criteria for glaucoma. These include interindividual variation in optic disc size11 and number of axons in the optic nerve.12 The additional requirement of functional evidence of glaucoma in the form of a visual field defect should help reduce the number of misclassifications of healthy individuals, although visual field testing in this perimetrically naive population has its own limitations.
By treating all people in the intervention group who had occludable angles with prophylactic laser iridotomy we will have treated some people who would never have developed angle closure. Mongolia is a vast, sparsely populated country in which many people live 500 km or more from the nearest ophthalmologist. In this setting it may be justifiable to treat all those with occludable angles. We hope to assess the magnitude of long term theoretical complications of laser iridotomy by comparing the two trial groups at follow up to establish whether intervention is associated with visually significant lens and corneal changes.
The acceptance of interventions in the population recruited to this trial was good but may not be representative of what would actually happen in a screening programme. All interventions required for an individual were performed on the same day, undoubtedly maximising uptake.
A potential weakness of any prospective study is the loss to follow up of recruited subjects. In the population studied within this trial the commonest cause of loss to follow up will be death. However, the estimate of mortality rates in this group will in itself be an important secondary outcome as it may have consequences for the age at which screening should begin in any future programme. The other reason for individuals dropping out from the study will be relocation to other areas. Although the Mongolians are traditionally a nomadic population there is much less movement of people now than there was in previous centuries. The majority of our study population live in a town or city and local knowledge within these small tightly knit communities together with good census data and the use of Polaroid photographs increases the chances of maximising follow up.
Before setting up population based programmes for early detection of individuals at risk of PACG in Asia the benefits and cost effectiveness of screening and subsequent interventions in reducing the incidence of glaucoma and any resulting visual morbidity must be demonstrated. This trial is an important step in the attempt to provide some evidence for or against the implementation of such large scale public health initiatives.
Acknowledgments
We would like to thank Pak Sang Lee, MSc, Judy Hall, and Alison Cubbitt for assistance in training of staff and monitoring of data collection. Paul Foster, FRCSEd, and Joe Devereux, FRCOphth, allowed use of their data and gave advice on study design and the manuscript. We are grateful to Professor Hugh R Taylor, MD, FRACO, Professor Richard Hayes, and Darwin Minassian, FRCOphth, for advice on study design. We would also like to thank Dr Davaasambuu Tsedenkhuu, Gombo And, Chimed Oyunsuren, Tsedengombo Lhagvasuren, and the staff of Bayanhongor hospital and the three district hospitals of Ulaanbaatar who worked on this project.
Financial support: This study was funded by the National Lotteries Charities Board, through Fight for Sight. The YAG laser used in this study was donated by the Velux Foundation, Copenhagen.
Proprietary interests: None.
REFERENCES
- 1.Foster PJ, Oen FT, Machin D, et al. The prevalence of glaucoma in Chinese residents of Singapore: a cross-sectional population survey of the Tanjong Pagar district. Arch Ophthalmol 2000; 118:1105–11. [DOI] [PubMed] [Google Scholar]
- 2.Foster PJ, Johnson GJ. Glaucoma in China: how big is the problem? Br J Ophthalmol 2001;85:1277–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nolan WP, Foster PJ, Devereux JG, et al. YAG laser iridotomy treatment for primary angle-closure in East Asian eyes. Br J Ophthalmol 2000; 84:1255–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salmon JF. Long-term intraocular pressure control after Nd-YAG laser iridotomy in Chronic angle-closure glaucoma. J Glaucoma 1993; 2:291–6. [PubMed] [Google Scholar]
- 5.Congdon N, Quigley HA, Hung PT, et al. Screening techniques for angle-closure glaucoma in rural Taiwan. Acta Ophthalmol 1996; 74:113–19. [DOI] [PubMed] [Google Scholar]
- 6.Devereux JG, Foster PJ, Baasanhu J, et al. Anterior chamber depth measurement as a screening tool for primary angle closure glaucoma in an East Asian population. Arch Ophthalmol 2000; 118:257–63. [DOI] [PubMed] [Google Scholar]
- 7.Wilson JMG, Jungner G. Principles and practice of screening for disease. (Public Health Papers No 34) Geneva: WHO, 1968.
- 8.Foster PJ, Baasanhu J, Alsbirk PH, et al. Glaucoma in Mongolia—a population-based survey in Hövsgöl Province, Northern Mongolia. Arch Ophthalmol 1996; 114:1235–41. [DOI] [PubMed] [Google Scholar]
- 9.Leske MC, Ederer FPM. Estimating incidence from age-specific prevalence in glaucoma. Am J Epidemiol 1981;113:606–13. [DOI] [PubMed] [Google Scholar]
- 10.Foster PJ, Buhrmann R, Quigley HA, et al. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol 2002;86:238–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jonas JB, Gusek GC, Naumann GO. Optic disc, cup and neuroretinal rim size, configuration and correlations in normal eyes [published errata appear in Invest Ophthalmol Vis Sci 1991;32:1893. and 1992;32:474–5]. Invest Ophthalmol Vis Sci 1988; 29: 1151–8. [PubMed] [Google Scholar]
- 12.Jonas JB, Schmidt AM, Muller-Bergh JA, et al. Human optic nerve fiber count and optic disc size. Invest Ophthalmol Vis Sci 1992;33:2012–18. [PubMed] [Google Scholar]