Abstract
Aim: The role of neoadjuvant chemotherapy was studied when first line enucleation cannot be safely performed in unilateral extensive retinoblastoma (major buphthalmia or radiologically detectable optic nerve involvement).
Methods: Six patients, referred for unilateral retinoblastoma, presented with major buphthalmia (two) or optic nerve invasion (four): they were treated by neoadjuvant chemotherapy using etoposide and carboplatin.
Results: Good tumour response was observed in the two patients with buphthalmia and in three of four cases with optic nerve involvement. Meningeal progressive disease was observed in the last patient. The five patients without disease progression were then operated on: anterior enucleation in the patients with buphthalmia and enucleation via a double neurosurgical and ophthalmological approach with prechiasmatic optic nerve section in the other three cases. Postoperative chemotherapy was performed in these five patients. Local radiotherapy to the chiasmatic region and posterior part of the optic canal was necessary in only one patient. The non-operated patient died with disease progression 6 months after the diagnosis. The other five patients are alive with a follow up of 12, 15, 21, 36, and 40 months after stopping treatment.
Conclusion: Neoadjuvant chemotherapy can be useful in extensive unilateral retinoblastoma with buphthalmia and/or radiological optic nerve invasion at diagnosis.
Keywords: retinoblastoma, chemotherapy, enucleation
Retinoblastoma is the most frequent eye tumour in children; it is unilateral in 60% of cases. In the great majority of cases of unilateral retinoblastoma, the tumour is extensive and vision is compromised. Treatment of this form is essentially based on primary enucleation. The prognosis is better when tumour resection is macroscopically and microscopically complete—that is, when the surgical procedure is performed without effraction of the eyeball and with healthy optic nerve resection margins. These two conditions cannot be achieved in the case of major buphthalmia1 and/or radiologically detectable optic nerve invasion at diagnosis. The chemosensitivity of retinoblastoma with extraocular, orbital, or metastatic involvement,2 and intraocular forms3–7 has been established. We therefore decided to investigate the use of neoadjuvant etoposide-carboplatin combination chemotherapy in the rare forms with major initial buphthalmia and/or radiologically detectable optic nerve invasion at diagnosis.
PATIENTS AND METHODS
Between December 1997 and November 2000, among 267 patients referred for retinoblastoma to our four institutions, six (2.5%) presented with extensive unilateral retinoblastoma with two cases of isolated major buphthalmia and four cases with radiologically detectable optic nerve invasion at diagnosis, two of whom had intraorbital optic nerve invasion, and the other two had pre-chiasmatic optic nerve invasion. This population comprised four boys and two girls, aged 18 months to 8 years. An initial staging assessment was systematically performed at diagnosis (bone marrow aspirate, bone marrow biopsy, lumbar puncture with cerebrospinal fluid cytology, bone scan, and axial magnetic resonance imaging): this assessment was negative in all six patients.
Initial treatment consisted of neoadjuvant chemotherapy combining etoposide and carboplatin, as described in the treatment of extraocular forms of retinoblastoma.2 The two patients with buphthalmia received a single course of etoposide-carboplatin. Patients with optic nerve invasion received two or three courses of etoposide-carboplatin. One of these patients received an additional preoperative course of etoposide-endoxan.8 A first evaluation was performed after completion of neoadjuvant treatment. The two buphthalmic patients were evaluated clinically. For the other four patients, the efficacy of chemotherapy was assessed by computed tomography (CT) and/or magnetic resonance imaging (MRI) and cytological examination of cerebrospinal fluid obtained by lumbar puncture.
Patients with no signs of progression were operated after neoadjuvant chemotherapy, by anterior enucleation for patients with major buphthalmia, and via a double anterior (ophthalmological) and subfrontal (neurosurgical) approach for cases with radiologically detectable optic nerve invasion at diagnosis. The intraoperative assessment determined the presence or absence of perforation of the eyeball for buphthalmic patients and the integrity of the zone of posterior section for patients with initial optic nerve invasion. The efficacy of neoadjuvant chemotherapy was also evaluated by histological examination of enucleation specimens.
Postoperative treatment was determined by the results of surgery and histological examination of the operative specimen. Patients with isolated initial buphthalmia received conventional adjuvant chemotherapy. Patients with initial radiologically detectable optic nerve invasion received adjuvant chemotherapy comprising conventional chemotherapy2,8–10 and high dose CARBOPEC chemotherapy (cyclophosphamide-etoposide-carboplatin) with peripheral haematopoietic stem cell support.11 The indication for postoperative radiotherapy was based on the level of optic nerve section and the histological results. Post-treatment follow up was based on clinical and radiological examination.
RESULTS
The clinical course of the patients is summarised in Table 1. The preoperative assessment showed clinical regression of the two cases of buphthalmia and reduction of tumour volume for the four patients with initial radiological optic nerve invasion (Fig 1). One of these four patients (with prechiasmatic optic nerve invasion) was not operated on after neoadjuvant chemotherapy because of meningeal progression detected by cytological analysis of cerebrospinal fluid on lumbar puncture performed just before the scheduled date of surgery.
Table 1.
Clinical summary of the patients
| Patients (age) | Clinicoradiological features | Neoadjuvant treatment | Evaluation | Enucleation histology | Postoperative treatment | Post-treatment response |
| 1 (3.5 years) | Buphthalmia | 1 etoposide-carboplatin | Clinical: regression | Necrotic tumour Invasion: prelaminar, choroidal, ciliary bodies | 2 etoposide-carboplatin* 2 cado† | 21 months Cr |
| 2 (22 months) | Buphthalmia | 1 etoposide-carboplatin | Clinical: regression | Necrotic tumour Invasion: intralaminar | 1 etoposide-carboplatin 2 vincristine-endoxan‡ | 15 months Cr |
| 3 (22 months) | Orbital portion of optic nerve | 3 etoposide-carboplatin | CT/MRI: tumour reduction CSF (−) | Necrotic tumour No residual optic nerve invasion | 2 etoposide-cyclophosphamide§ CARBOPEC¶ | 40 months Cr |
| 4 (1 year) | Orbital portion of optic nerve | 3 etoposide-carboplatin 1 etoposide-cyclophosphamide | CT/MRI: tumour reduction CSF (−) | Necrotic tumour Invasion: prelaminar | 3 etoposide-carboplatin 1 etoposide-cyclophosphamide CARBOPEC | 36 months Cr |
| 5 (8 years) | Prechiasmatic portion of optic nerve | 2 etoposide-carboplatin Intrathecal thiotepa | MRI: tumour reduction CSF (−) | Macroscopic invasion of optic nerve resection margins Necrotic tumour | 3 etoposide-cyclophosphamide 1 etoposide-arboplatin CARBOPEC Radiotherapy | 12 months CR |
| 6 (18 months) | Buphthalmia Prechiasmatic portion of optic nerve | 2 etoposide-carboplatin | CT: tumour reduction CSF (+) | No enucleation Early meningeal progression | Died |
*Etoposide 100 mg/m2/day, D1–D5, carboplatin 160 mg/m2/day, D1–D5.2
†CADO: cyclophosphamide 300 mg/m2/day, D1–D5, vincristine 1.5 mg/m2/day, D1, D5, adriamycin 30 mg/m2/day, D4, D5).9
‡Vincristine 1.5 mg/m2/day, D1, D5 cyclophosphamide 1 g/m2/day, D1–D3.9,10
§Etoposide 150 mg/m2/day, D1–D3, cyclophosphamide 1 g/m2/day, D1–D3.8
¶CARBOPEC carboplatin 350 mg/m2/day, D1–D5, etoposide 350 mg/m2/day, D1–D5, cyclophosphamide 1.6 g/m2/day, D2–D5.11
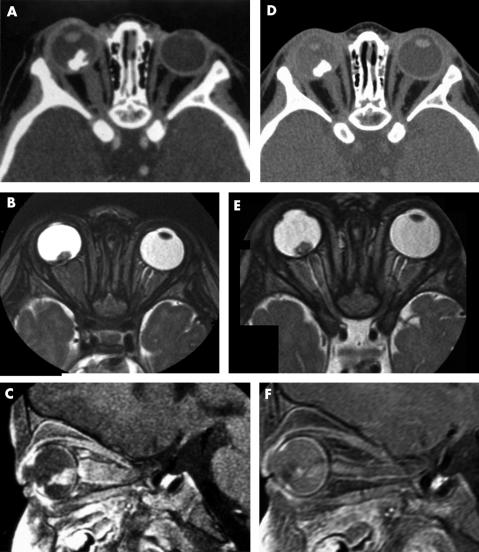
Figure 1.
(A–C) Left unilateral retinoblastoma with orbital optic nerve involvement at diagnosis. Axial post-contrast CT scan (A), axial T2 weighted (B), and enhanced fat saturated T1 weighted sagittal (C) MR images. Intraocular calcified tumour with low signal intensity on the T2 weighted sequence and high signal intensity after gadolinium injection on the T1 weighted sequence. The optic nerve is enlarged and shows the same signal abnormalities as the primitive intraocular tumour. (D–F) Preoperative imaging after two courses of etoposide and carboplatin. Axial post-contrast CT scan (D), axial T2 weighted (E), and enhanced fat saturated T1 weighted sagittal (F) MR images. The intraocular tumour volume remains unchanged but post-contrast MR (F) shows a decreasing enhancement. Optic nerve involvement has significantly decreased, with only slight residual enlargement and enhancement.
The five patients with no signs of progression were operated. The intraoperative assessment showed that enucleation was performed without effraction of the eyeball in the two buphthalmic patients. Three of the four patients with optic nerve invasion were able to be operated on; the optic nerve section was sufficiently posterior and in a macroscopically healthy zone in the two patients with intraorbital optic nerve invasion, while a macroscopically suspicious resection margin was observed in the patient with optic nerve invasion involving the prechiasmatic region. Postoperative histological examination of the enucleation specimens showed largely necrotic retinoblastoma. The two patients with major initial buphthalmia had prelaminar optic nerve invasion associated with massive choroidal and ciliary body invasion in one case and isolated intralaminar optic nerve invasion in the other case; optic nerve resection margins were healthy in both cases.
In one of the patients with intraorbital optic nerve invasion, the optic nerve was sectioned at two places in the intraorbital portion of the nerve: examination of the two fragments of optic nerve did not reveal any tumour invasion and the resection margins were also healthy. In the other patient with intraorbital optic nerve invasion, the optic nerve was sectioned in the intracanalicular portion: histological examination has revealed minimal choroidal invasion and prelaminar optic nerve invasion, but healthy resection margins. Histological examination of the optic nerve in the patient with prechiasmatic optic nerve invasion did not show any tumour invasion of this segment, despite the suspicious macroscopic appearance. The non-operated patient with early meningeal progression died 6 months after the initial diagnosis. The five operated patients have a follow up of 12–40 months after completion of postoperative chemotherapy and are still in complete remission of their disease. Only one patient received radiotherapy, using a proton-photon combination because of a macroscopically suspicious prechiasmatic optic nerve section.
DISCUSSION
Unilateral retinoblastoma represents 60% of all cases of retinoblastoma with a median age of 2 years at the time of diagnosis. Forms with initial buphthalmia and optic nerve invasion diagnosed on imaging have become exceptional in industrialised countries, but are still frequent in underdeveloped countries.12 Enucleation is mandatory in cases of extensive unilateral retinoblastoma. This procedure must be performed under optimal conditions, satisfying the following criteria: section of the optic nerve as posterior as possible in the orbital cavity and absence of effraction of the eyeball. These conditions could not be achieved in the six cases presented here, but the use of neoadjuvant chemotherapy allowed us to perform surgery under favourable conditions in five of these patients who were operated without perforation of the eyeball and with healthy optic nerve resection margins. In the case of optic nerve invasion, surgery performed by two teams (ophthalmological and neurosurgical) was not only as oncologically complete as possible, but also allowed preservation of oculomotor muscles and insertion of an implant, ensuring a better cosmetic result.
Neoadjuvant chemotherapy certainly made interpretation of histological risk factors more difficult. In particular, necrosis may be spontaneous and/or induced by chemotherapy. Nevertheless, histological examination of the optic nerve showing a healthy resection margin suggests the benefit of neoadjuvant chemotherapy in these patients with radiologically documented optic nerve invasion. Buphthalmic patients could not have been operated on immediately without a high risk of ocular rupture. Brief neoadjuvant chemotherapy allowed these patients to be operated on under better oncological conditions.
Neoadjuvant chemotherapy also limits the use of radiotherapy to only those cases with pathological optic nerve resection margins at the time of surgery. No radiotherapy was used after this double surgical approach when optic nerve resection margin was negative. Neoadjuvant chemotherapy can therefore be useful in the management of unilateral forms of retinoblastoma with initial buphthalmia and/or radiologically detectable optic nerve invasion at diagnosis: it allows surgery by a ophthalmological and neurosurgical team under good oncological conditions in the case of optic nerve invasion.
REFERENCES
- 1.Shields JA, Shields CL, Suvarnamani C, et al. Retinoblastoma manifesting as orbital cellulitis. Am J Ophthalmol 1991;112:442–9. [DOI] [PubMed] [Google Scholar]
- 2.Doz F, Neuenschwander S, Plantaz D, et al. Etoposide and carboplatin in extraocular retinoblastoma: a study by the Société Française d’Oncologie Pédiatrique. J Clin Oncol 1995;13:902–9. [DOI] [PubMed] [Google Scholar]
- 3.Levy C, Doz F, Quintana E, et al. The role of chemotherapy alone or in combination with hyperthermia in the primary treatment of intraocular retinoblastoma: preliminary results in 30 patients treated at Institut Curie. Br J Ophthalmol 1998;82:1154–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greenwald MJ, Strauss LC. Treatment of intraocular retinoblastoma with carboplatin and etoposide chemotherapy. Ophthalmology 1996;103:1989–97. [DOI] [PubMed] [Google Scholar]
- 5.Kingston J, Hungerford JL, Madreperla SA et al. Results of combined chemotherapy and radiotherapy for advanced intraocular retinoblastoma. Arch Ophthalmol 1996;114:1339–43. [DOI] [PubMed] [Google Scholar]
- 6.Nenadov Beck M, Balmer A, Dessing C, et al. First-line chemotherapy with local treatment can prevent external beam irradiation and enucleation in low stage intraocular retinoblastoma. J Clin Oncol 2000;18:2881–7. [DOI] [PubMed] [Google Scholar]
- 7.Gallie BL, Budning A, DeBoer G, et al. Chemotherapy with focal therapy can cure intraocular retinoblastoma without radiotherapy. Arch Ophthalmol 1996;114:1321–8. [DOI] [PubMed] [Google Scholar]
- 8.Meresse V, Vassal G, Michon J et al. Combined continuous infusion etoposide with high-dose cyclophosphamide for refractory neuroblastoma: a phase II study from the Société Française d’Oncologie Pédiatrique. J Clin Oncol 1993;11:630–7. [DOI] [PubMed] [Google Scholar]
- 9.Khelfaoui F, Validire P, Auperin A, et al. Histopathological risk factors in retinoblastoma: a retrospective study on 172 patients treated in a single institution. Cancer 1996;77:1206–13. [PubMed] [Google Scholar]
- 10.Pratt CB, Crom DB, Howarth C. The use of chemotherapy for extraocular retinoblastoma. Med Pediatr Oncol 1985;13:330–5. [DOI] [PubMed] [Google Scholar]
- 11.Namouni F, Doz F, Tanguy ML, et al. High dose chemotherapy with carboplatin, etoposide and cyclophosphamide followed by hematopoietic stem cell rescue in patients with high risk retinoblastoma: a SFOP and SFGM study. Eur J Cancer 1997;33:2368–75. [DOI] [PubMed] [Google Scholar]
- 12.Chantada G, Fandino A, Manzitti J et al. Late diagnosis of retinoblastoma in a developing country. Arch Dis Child 1999;80:171–4. [DOI] [PMC free article] [PubMed] [Google Scholar]