Abstract
Background: Amblyopia treatment is not standardised and differences between centres and countries have not been systematically investigated. This survey compares the different patterns of orthoptic treatment of amblyopia in the United Kingdom (UK) and three German speaking countries (GSC).
Methods: Questionnaires were sent to orthoptists in the UK and the GSC asking for their preferred choices of treatment of amblyopia between the ages of 6 months to 10 years.
Results: The following significant differences in management of amblyopia were found: (1) the number of hours of occlusion per week was higher in the GSC, p<0.0001, (2) orthoptists in the GSC treat amblyopia up to an older age. Orthoptists in the GSC and in the UK predicted similar treatment outcomes.
Conclusion: Orthoptists in the GSC usually treat patients more intensively and for longer, while the prediction of visual outcome does not differ significantly between countries. These results highlight the lack of standardisation in the treatment of the various types of amblyopia.
Keywords: amblyopia, strabismus, anisometropia, deprivation, questionnaires
Amblyopia affects 2–3% of the population and is defined as a reduction in vision, as a result of interruption of normal visual development during the sensitive period in childhood.1 It is generally accepted that occlusion of the non-amblyopic eye is the mainstay treatment of amblyopia.2,3 However, its efficacy is poorly quantified, as results are difficult to interpret in the absence of controlled trials.4
Treatment modalities, such as whether spectacles alone are efficient, the optimum duration and intensity of occlusion, part time or full time occlusion, or the efficacy of penalisation are unknown. The outcome of treatment depends on the type of amblyopia, initial visual acuity, compliance,5 and the age when treatment is started.6 Success rates of treatments have been reported between 30%1 to 92%.7
Occlusion treatment for amblyopia has been challenged recently by a report by the NHS Centre of Review and Dissemination.8 It suggests that preschool vision screening for amblyopia and its risk factors be discontinued because of lack of evidence of any demonstrable benefit. The report states that no study of the natural course of untreated amblyopia has been performed, that no studies have compared no treatment with treatment, and that most of the studies were methodologically flawed.
One of the authors (IG) has worked in several European countries (Austria, Germany, Switzerland, and the United Kingdom) and is aware of the variations in the management of amblyopia between German speaking countries (GSC) and the United Kingdom (UK). Firstly, the infrastructure of the ophthalmic units is different. Often in GSC a separate strabismus department manages amblyopia. In the UK, most departments have a well defined paediatric ophthalmology service where the orthoptists work closely with one or more consultants who have a special interest in paediatric ophthalmology and strabismus, but they are usually not a separate department. Secondly, she had the impression that amblyopia treatment was predominantly led by the orthoptists in the UK while the ophthalmologists were more involved in the GSC.
This study was set up to evaluate approaches of orthoptists towards the treatment of amblyopia and its outcomes in three GSC—namely, Germany, Switzerland, and Austria, compared to the United Kingdom.
METHODS
The questionnaire was sent in German by post to 64 orthoptists in GSC; 32 to Germany, 10 to Switzerland, and 22 to Austria. For the 60 questionnaires sent out within the UK, 45 were sent to orthoptic departments in England, 12 to Scotland, two to Northern Ireland, and one to Wales. The questionnaire in German was an exact translation of the original English questionnaire. All the departments with a chief orthoptist, listed in the Associations of Orthoptics for Germany, Switzerland and Austria were included in this study. Orthoptic departments listed in the British Orthoptic Society (BOS) Directory of Members were invited to complete the postal questionnaire. We attempted to match the departments in the UK by selecting those which have chief orthoptists, since these departments are more likely to set teaching standards.
Questionnaires were sent to hospital departments only. After 2 months, another invitation was sent out to centres that failed to respond, in an attempt to increase the response rate. One orthoptist per department, usually the head orthoptist, was asked to fill in the questionnaire. Orthoptists were asked about the number of orthoptists and to estimate the numbers of new amblyopic patients per week examined in their department.
The questionnaire was designed to evaluate practice variations in the management of amblyopia. Clinical scenarios described patients with strabismic, anisometropic, and deprivation amblyopia.
For strabismic and anisometropic amblyopia identical questions were asked for patients at ages 6 months and 2, 4, 6, 8, and 10 years. They were further divided into mild (two lines decrease in visual acuity of the amblyopic eye) and severe (visual acuity of 6/60) strabismic amblyopia and mild and severe anisometropic amblyopia. Orthoptists were asked to state their preferred first choice of treatment, with the options (a) spectacles only, (b) spectacles and occlusion, (c) spectacles and atropine, or (d) none of the above. If occlusion therapy was preferred, the preference for part time or full time occlusion and the intensity of treatment was requested; this was converted to hours per week. Those who chose more than one option were omitted. The orthoptists were also asked to estimate the percentage of patients in whom they predicted the visual acuity in the amblyopic eye would improve by at least two lines using their preferred treatment. The age for discontinuation of treatment if visual acuity failed to improve was requested. This question was included in an attempt to establish an accepted sensitive period of visual development and not to imply that treatment was discontinued at a particular age.
In addition, the orthoptists were asked for their preferred approach to deprivation amblyopia in a 3 week old infant with unilateral cataract and the treatment of postoperative aphakia with contact lenses and occlusion (Table 1).
Table 1.
Treatment of a unilateral dense cataract in a 3 week old infant and subsequent correction of postoperative aphakia
| Correction of aphakia | GSC (n) | UK (n) |
| Secondary IOL in contact lens intolerance | 53% (38) | 54% (22) |
| Mean age for secondary IOL | 3.1 years (27) | 2.8 years (6) |
| Mean age when treatment is stopped when VA = 6/12 | 8.7 years (33) | 5.9 years (28) |
| Mean age when treatment is stopped when VA = 6/60 | 7.4 years (33) | 6.1 years (25) |
Further questions included whether the orthoptists used atropine at all and whether in non-compliant patients hospital admission would be considered. The orthoptists were asked which people were involved in the decision making process for amblyopia treatment and strabismus surgery and to judge the severity of psychological problems of the patients and their families caused by occlusion therapy. The questionnaire was validated by eight orthoptists in our department and the feedback received was used to reformulate some questions.
In the statistical analysis, continuous measurements were modelled using linear regression and the models were compared using analysis of variance. Proportions were modelled using logistic regression and the models compared by likelihood ratio tests. Within models individual coefficients were compared using Wald statistics based on robust standard errors that adjust for the correlation between multiple responses by the same orthoptist.
RESULTS
Forty two out of 64 questionnaires that were sent to orthoptists in the GSC were returned, a response rate of 66%. A total of 40 questionnaires were available for analysis. Two questionnaires were omitted because they were completed by ophthalmologists. From the UK, 41 out of 60 questionnaires were returned, a 68% response rate.
The average number of full time equivalent orthoptists in each department was 3.5 in the GSC and 6.0 in the UK. The average number of new amblyopic patients seen per department in a month was 4.9 in the GSC and 13.0 in the UK. The number of new patients per orthoptist per month was 7.3 in the GSC and 11.6 in the UK, p = 0.08.
First choice of treatment
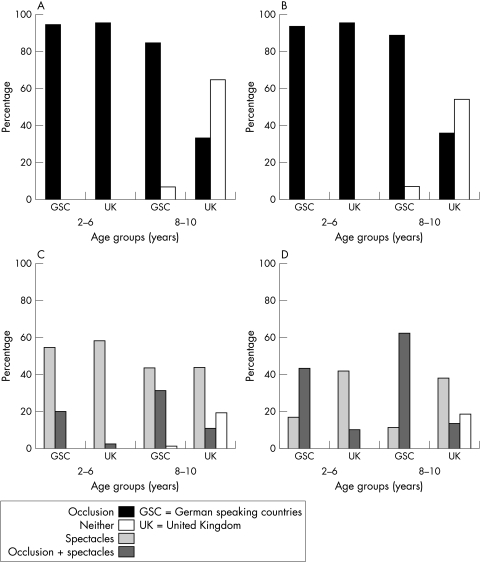
In both regions results for the first choice of treatment were similar for ages 2, 4, and 6 years and 8 and 10 years, and so the data for these age groups were combined. These two groups have therefore been labelled as ages 2–6 and ages 8–10. In both the GSC and the UK, more than 90% of orthoptists preferred occlusion only as their first choice in treating mild (Fig 1A) and severe (Fig 1B) strabismic amblyopia for children aged 2–6 years. For the older age group, occlusion remained the first choice of treatment for mild and severe strabismic amblyopia in the GSC, but this preference was not mirrored in the UK, (p<0.0001), where more than 50% chose no treatment.
Figure 1.
First choice treatment of mild (A) and severe (B) strabismic and mild (C) and severe (D) anisometropic amblyopia.
In mild anisometropic amblyopia (Fig 1C), both GSC and UK orthoptists preferred using spectacles only as their first choice treatment in all age groups. However, in severe anisometropic amblyopia (Fig 1D), orthoptists in the GSC preferred using spectacles plus occlusion as their first choice treatment, significantly more than their UK counterparts who preferred spectacles only as their first choice (p<0.001).
Another large difference was in the orthoptists’ approach to older age children with mild and severe anisometropic amblyopia. A significantly higher proportion of UK orthoptists chose no treatment (p = 0.003) for this age group while most orthoptists from GSC attempted treatment (Fig 1C and D).
Atropine penalisation was used as a first choice by only 3% of orthoptists for mild and severe strabismic amblyopia in GSC and was not reported at all from the UK. For mild anisometropic amblyopia it was reported from GSC by 6.7% and from the UK by 0.8% and for severe anisometropic amblyopia in the GSC by 5.4% and in the UK not at all.
Part-time versus full time occlusion
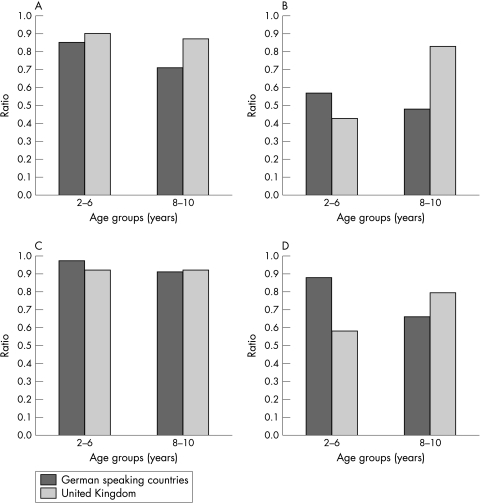
In both regions results for the first choice of treatment were similar for ages 2, 4, and 6 years and 8 and 10 years, and so the data for these age groups were combined together. These two groups have therefore been labelled as ages 2–6 and ages 8–10. Part time occlusion was preferred to full time by orthoptists in both the UK and GSC for mild strabismic amblyopia in both age groups (Fig 2A). In severe strabismic amblyopia (Fig 2B) there was a significant difference for the older age group with more GSC orthoptists preferring full time occlusion as compared to those in the UK (p = 0.03). Part time was preferred to full time occlusion by orthoptists in both the UK and GSC for mild anisometropic amblyopia (Fig 2C) in all age groups. For severe anisometropic amblyopia, there was a significant difference in the younger age group, with UK orthoptists preferring full time occlusion (p = 0.004).
Figure 2.
Preferred type of occlusion in mild (A) and severe (B) strabismic and mild (C) and severe (D) anisometropic amblyopia. The data are presented as a ratio of those who prefer part time occlusion to the number of responders.
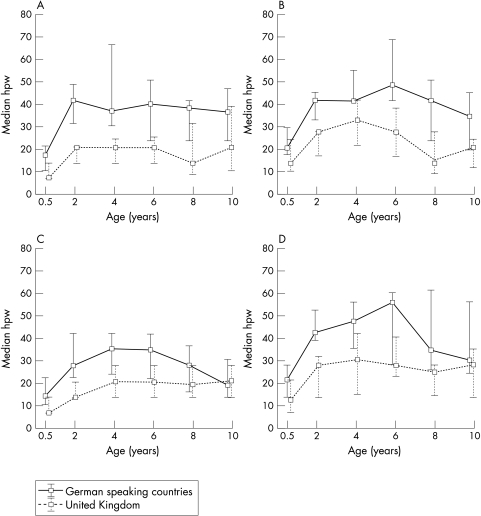
Intensity of treatment
The median number of hours per week of part time occlusion reported in the GSC was significantly higher than in the UK (p<0.0001) for all groups. Figure 3 shows that more intense patching is preferred through all age ranges and types of amblyopia in the GSC. The most striking difference was in mild strabismic amblyopia, where orthoptists in GSC reported occlusion almost twice as many hours per week than those in the UK (Fig 3A).
Figure 3.
Median, first, and third quartile of the intensity of part time occlusion (median hours per week, hpw) in mild (A) and severe (B) strabismic and mild (C) and severe (D) anisometropic amblyopia.
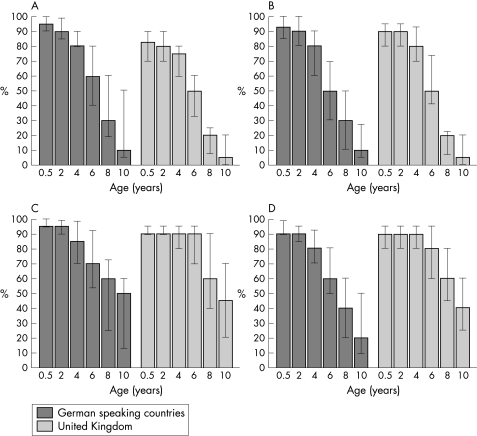
Predicted treatment outcome
Orthoptists in the GSC and in the UK gave very similar estimates of the percentage of children improving their visual acuity to be at least two lines in the amblyopic eye at the end of the preferred choice of treatment (Fig 4). The responses from the GSC and UK orthoptists for anisometropic amblyopia (Fig 4C and D) were more optimistic than for strabismic amblyopia in the older age groups (Fig 4A and B).
Figure 4.
Median, first, and third quartile of the predicted treatment outcome (by at least two lines of improvement) in mild (A) and severe (B) strabismic and mild (C) and severe (D) anisometropic amblyopia
Discontinuation of treatment
UK orthoptists reported that they would discontinue occlusion if treatment failed at a younger age than orthoptists from GSC.
Mild strabismic; UK, mean 6.8 (SD 1.0) years compared to GSC, mean 10.0 (SD 2.4) years, severe strabismic; UK mean 6.5 (SD 1.1) years compared to GSC, mean 8.9 (SD 2.7) years (p<0.001).
Mild anisometropic; UK, mean 8.4 (SD 2.3) years compared to GSC mean 10.1 (SD 2.2) years, severe anisometropic; UK mean 8.4 (SD 2.1) years compared to GSC, mean 9.5 (SD 2.8) years (p = 0.02).
Deprivation amblyopia
Following unilateral congenital cataract surgery, 93% (n = 40) in the GSC and 90% (n = 31) in the UK favoured using contact lenses and occlusion therapy rather than contact lenses alone; 86% (n = 37) in the GSC and 87% (n = 30) in the UK would prefer to prescribe contact lenses for near, p = 1.00. 95% (n = 39) in the GSC and 86% (n = 28) in the UK preferred part time occlusion for deprivation amblyopia, p = 0.39. The mean intensity of part time occlusion prescribed was 22 hours per week (n = 20) in GSC and 28 (n = 20) in the UK, p = 0.26. In contact lens intolerance, spectacles were preferred in 95% (n = 40) in GSC and 71% (n = 28) in UK, p = 0.01. The estimated likelihood of secondary lens implantation was 53% (n = 38) in the GSC and 54% (n = 22) in the UK, p = 1.00. Orthoptists in both the GSC and the UK thought the appropriate age for correcting an aphakic child with bifocal spectacles (p = 0.001) and for lens implantation (p = 0.75) was 3 years. Orthoptists in the UK favoured stopping treatment for deprivation amblyopia at a younger age.
Other aspects
The majority of orthoptists would use atropine sometimes for amblyopia therapy, 60% in the GSC and 87% in the UK. For those who were non-compliant with the treatment of strabismic amblyopia, hospital admission was considered more frequently in the UK, 83% (n = 40) compared to 63% (n = 40) in the GSC (p = 0.05).
A negative psychological effect of occlusion therapy was estimated to be infrequent in both the GSC and the UK, p = 1.00, as shown in Table 2.
Table 2.
Psychological effects of amblyopia treatment and who decides on the mode of occlusion therapy and surgical treatment in managing amblyopia
| Negative psychological effect | Always | Mostly | Sometimes | Rarely | Never |
| GSC (n=39) | 0% | 3% | 33% | 64% | 0% |
| UK (n=40) | 3% | 3% | 50% | 45% | 0% |
| Decision on mode of treatment | Orthoptists | Ophthalmologists | Both | ||
| GSC (n=40) | 65% | 10% | 25% | ||
| UK (n=40) | 100% | 0% | 0% | ||
| Decision on surgical treatment | Orthoptists | Ophthalmologists | Both | ||
| GSC (n=40) | 3% | 60% | 38% | ||
| UK (n=40) | 15% | 48% | 38% | ||
The mode of treatment for amblyopia was decided by orthoptists only in the UK whereas ophthalmologists were frequently involved in GSC, p<0.001. Orthoptists were slightly more involved in the decision on the surgical treatment for strabismus in the UK compared to the GSC, but this was insignificant, p = 0.14 (see table 2).
DISCUSSION
This study highlights international differences in treatment approaches. GSC orthoptists prefer more intensive occlusion regimens, although this does not correlate with a better predicted outcome. Amblyopia management is teamwork of which the orthoptist is only one component. With this questionnaire, we surveyed only one component of the team; however, it does give us an overall impression in the differences in management of amblyopia. UK orthoptists preferred spectacles without occlusion in the treatment of severe anisometropic amblyopia as their first choice of treatment, and they discontinued treatment earlier than in the GSC. Most of the responses for mild anisometropia chose spectacles only as their first choice treatment. The questionnaire was limited as we did not establish whether this group of orthoptists proceeded to occlusion therapy and when they would do so. The size of the study does not allow us to evaluate trends within subregions.
In general, occlusion therapy is widely accepted as the first choice treatment of both strabismic and anisometropic amblyopia.2,3 This is reflected in the responses throughout the regions included in this study. Orthoptists in the GSC prefer treating severe anisometropic amblyopia with spectacles combined with occlusion while UK orthoptists prefer the less aggressive approach of observing the visual improvement from correcting the refractive error before introducing occlusion. There is little research in the literature to suggest the optimal approach. A pilot study of eight subjects by Moseley et al9 found that significant visual improvement was achieved for those who received spectacle correction, while further gains in visual improvement were not sustained during occlusion.
The lack of standardisation in the management of amblyopia applies also to the intensity of treatment regimes. In Leicestershire, Hiscox et al10 found the average amount of occlusion prescribed to be 1.5 hours daily ranging between 10 minutes and 8 hours daily. Cleary11 looked at occlusion therapy in 73 patients in the Glasgow area and reported a mean daily dosage of 3.7 hours. Although the intensity of occlusion regimes varies between units within the UK, the inter-regional differences are even greater with GSC orthoptists prescribing significantly more.
In the literature, some practitioners are reported to favour full time occlusion3 while others just a few minutes’ occlusion each day.12 Our study shows a preference for part time occlusion.
There are studies that have shown success in treating amblyopia with atropine penalisation.13–15 Our survey shows that despite this, atropine is not the preferred first choice treatment for either strabismic or anisometropic amblyopia. Only 3% respondents from the GSC and none from the UK used atropine as their first choice treatment for strabismic amblyopia. However, our study shows 60% of orthoptists from the GSC and 80% from the UK would consider atropine penalisation as a second line approach.
The predicted treatment outcome in our survey is similar between GSC and the UK. If these predictions are realistic it may be possible that orthoptists in the GSC are over-treating. As these predicted outcomes are only the orthoptists’ beliefs, a study comparing the effective treatment outcomes in the different countries would be very informative. Orthoptists in both the GSC and the UK thought that a better outcome is obtainable with earlier treatment. Very few orthoptists in the GSC and the UK found occlusion therapy to have a negative psychological effect in this study. Since occlusion therapy is a large part of orthoptists’ professional activity, they may have a vested interest in this answer and this may have produced a bias in their response.
Two large pooled data sets by Woodruff et al5 and Flynn et al6 highlight a large variation in treatment outcomes. The two pooled data sets have been compared16—showing that a final visual acuity of 6/12 or better was achieved in 59.9%5 and 73.7%.6 They both found the depth of amblyopia at presentation to be the main determinant of visual outcome.
The effectiveness of occlusion is poorly established, partly as a result of difficulty in determining compliance. Compliance with patching may be poor17 and it is possible that patients in different countries and cultures do not comply in the same way with occlusion therapy. This might result in a similar real time of occlusion despite differences in prescription. Measurement of compliance with a dose occlusion monitor18,19 in different countries would be interesting and might reveal a dose-effect relation of occlusion therapy.
Unilateral congenital cataracts are uncommon and can represent a challenge. They are a potent cause of deprivation amblyopia and have to be addressed with urgency.20 Postoperative care is also crucial for visual development. In the literature visual acuity outcome after unilateral surgery for congenital cataract varies between 20/60 and 20/115.21 Our questionnaire highlighted that orthoptists in the UK and the GSC had very similar approaches to the postoperative treatment of early cataract surgery regarding the use of contact lenses and occlusion therapy. The main difference found was the duration of treatment.
This questionnaire highlights differences in the management of amblyopia within Europe. This could be due to the different orthoptic training programmes that advocate different attitudes towards amblyopia treatment. The textbooks, which are different in the two countries,22,23 do not clearly define treatment regimes. There may be cultural differences between countries—for example, towards compliance and acceptability towards patching. In view of this, there is a great need for the management of amblyopia to be more evidence based in orthoptics.
The most striking difference in our survey was that the treatment was in most aspects more intensive in the GSC than in the UK. On the other hand the anticipated outcomes were not different. Our findings show a lack of uniformity in the approach towards amblyopia treatment. Further studies to investigate the optimal approach for different amblyopia types, dose effectiveness, compliance, and necessary duration may allow the establishment of more uniform and effective occlusion treatment plans.
Acknowledgments
The authors thank all orthoptists who completed questionnaires that made this study possible.
REFERENCES
- 1.Flynn JT, Cassady JC. Current trends in amblyopia therapy. Ophthalmology 1978;85:428–50. [DOI] [PubMed] [Google Scholar]
- 2.Olson RJ, Scott WE. A practical approach to occlusion therapy for amblyopia. Sem Ophthalmol 1997;12:161–5. [Google Scholar]
- 3.Von Noorden GK. In: Binocular vision and ocular motility: theory and management of strabismus. 5th ed. St Louis: CV Mosby, 1996:512–20.
- 4.Mosely MJ, Fielder AR. Occlusion therapy for childhood amblyopia: current concepts in treatment evaluation. In: Vital-Durand F, Atkinson J, Braddick OJ, eds. Infant vision. Oxford: Oxford University Press, 1996:383–99.
- 5.Woodruff G, Hiscox F, Thompson JR, et al. Factors affecting the outcome of children treated for amblyopia. Eye 1994;8:627–31. [DOI] [PubMed] [Google Scholar]
- 6.Flynn JT, Schiffman J, Feuer W, et al. The therapy of amblyopia: an analysis of the results of amblyopia therapy utilizing the pooled data of published studies. Trans Am Ophthalmol Soc 1998;96:431–53. [PMC free article] [PubMed] [Google Scholar]
- 7.Scott WE, Dickey CF. Stability of visual acuity in amblyopic patients after visual maturity. Graefes Arch Clin Exp Ophthalmol 1988;226:154–7. [DOI] [PubMed] [Google Scholar]
- 8.Snowdown SK, Stewart-Brown SL. Pre-school screening: results of a systematic review. York: NHS Centre for Review and Dissemination. 1997. (CDR report 9.)
- 9.Moseley MJ, Fielder AR, Irwin M, et al. Effectiveness of occlusion therapy in ametropic amblyopia: a pilot study. Br J Ophthalmol 1997;81:956–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hiscox F, Strong N, Thompson JR, et al. Occlusion for amblyopia: a comprehensive survey of outcome. Eye 1992;6:300–4. [DOI] [PubMed] [Google Scholar]
- 11.Cleary M. Efficacy of occlusion for strabismic amblyopia: can an optimal duration be identified? Br J Ophthalmol 2000;84:572–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watson PG, Sanac AS, Pickering MS. A comparison of various methods of treatment of amblyopia: a block study. Trans Ophthalmol Soc UK 1985;104:319–28. [PubMed] [Google Scholar]
- 13.Foley-Nolan A, McCann A, O’Keefe M. Atropine penalisation versus occlusion as the primary treatment for amblyopia. Br J Ophthalmol 1997;81:54–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simons K, Gotzler K, Vitale S. Penalization versus part-time occlusion and binocular outcome in treatment of strabismic amblyopia. Ophthalmology 1997;104:2156–60. [DOI] [PubMed] [Google Scholar]
- 15.Simons K, Stein L, Sener E, et al. Full-time atropine, intermittent atropine, and optical penalization and binocular outcome in treatment of strabismic amblyopia. Ophthalmology 1997;104:2143–55. [DOI] [PubMed] [Google Scholar]
- 16.Flynn JT, Woodruff G, Thompson JR, et al. The therapy of amblyopia: an analysis comparing the results of amblyopia therapy utilizing two pooled data sets. Trans Am Ophthalmol Soc 1999;97:373–95. [PMC free article] [PubMed] [Google Scholar]
- 17.Wright EC. Non-compliance—or how many aunts has Matilda? Lancet 1993;342:909–13. [DOI] [PubMed] [Google Scholar]
- 18.Fielder AR, Irwin M, Auld R et al. Compliance in amblyopia therapy: objective monitoring of occlusion. Br J Ophthalmol 1995;79:585–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simonsz HJ, Polling JR, Voorn R, et al. Electronic monitoring of treatment compliance in patching amblyopia. Strabismus 1999;7:113–23. [DOI] [PubMed] [Google Scholar]
- 20.Birch EE, Stager D, Leffler J, et al. Early treatment of congenital unilateral cataract minimizes unequal competition. Invest Ophthalmol Vis Sci 1998;39:1560–6. [PubMed] [Google Scholar]
- 21.Catalano RA, Simon JW, Jenkins PL, et al. Preferential looking as a guide for amblyopia therapy in monocular infantile cataracts. J Pediatr Ophthalmol Strabismus 1987;24:56–63. [DOI] [PubMed] [Google Scholar]
- 22.Mein J. In: Diagnosis and management of ocular motility disorders. 2nd ed. Oxford: Blackwell Scientific, 1991.
- 23.Haase W. Amblyopie. In: Kaufmann H, ed. Strabismus. Stuttgart: Ferdinand Enke Verlag, 1995.