Coxsackievirus is a kind of enterovirus, which may cause respiratory and gastrointestinal symptoms, erythema, meningoencephalitis, myocarditis, pericarditis, and myositis. Although Coxsackievirus B4 is apparently a rare cause of chorioretinitis, Coxsackievirus infection and concurrent posterior segment inflammation have been disclosed in a few cases. However, iridocyclitis, scattered haemorrhagic dots, and occlusive retinal vasculitis have not previously reported as being features of Coxsackievirus B4 infectious ocular disease.
Case report
A 34 year old man was referred to our hospital with a 2 week history of inferior visual field defect and visual loss in his right eye. His left eye was asymptomatic. A few days before the onset of visual manifestations, the patient noted a prodrome of viral infection, consisting of severe headache and high grade fever of 38.0–39.2°C, joint pain, and general malaise. There was no significant medical or family history. At the initial ophthalmic examination, his best corrected visual acuities were 10/20 in the right eye and 25/20 in the left eye, and intraocular pressure was normal in both eyes. Slit lamp examination showed moderate cellular infiltration in the anterior chamber in both eyes. Humphrey central visual field testing demonstrated relative scotoma inferior to fixation in the right eye. Goldmann peripheral visual field testing was within normal limits in both eyes. Ophthalmoscopic examination disclosed subretinal exudates with haemorrhage in the parafovea and the mid-periphery of bilateral eyes (Fig 1). Moreover, scattered haemorrhagic dots and blots were observed along retinal vessels. The optic discs appeared normal. Fluorescein angiography demonstrated occlusive retinal vasculitis characterised by blocked fluorescence and mild dye leakage from the retinal vessels corresponding to the lesions detected clinically, and irregular choroidal background fluorescence (Fig 2). Laboratory examination findings were normal except a white blood cell count of 10 500 ×106/l, GOT of 76 IU/l, GPT of 209 IU/l, gamma-GTP of 88 IU/l, and LDH of 771 IU/l. Serological tests, however, revealed a slight elevation of serum antibody to Coxsackievirus B4, at a titre of 1:8 (neutralisation test).
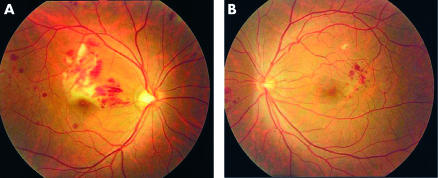
Figure 1.
Photographs of right eye (A) and left eye (B) at the initial ophthalmic examination. Subretinal exudates with haemorrhage around the macula and near the disc, and scattered haemorrhagic blots are evident.
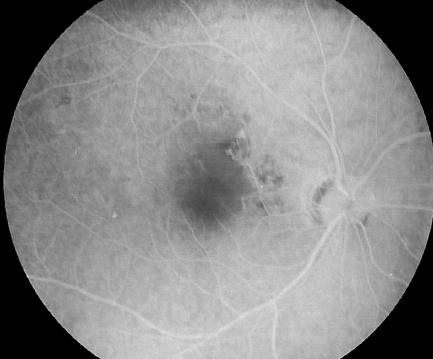
Figure 2.
Fluorescein angiograms of the right eye. Note blocked fluorescence and slight dye leakage from the retinal vessels around the macula, and irregular choroidal background fluorescence.
The patient's general condition improved gradually without specific medication. Cellular infiltration in the anterior chamber gradually disappeared. The retinal exudative lesions reduced in size, and haemorrhage tended to decrease. Eight months after the initial ophthalmic examination, bilateral exudative lesions had improved and were replaced by scars, and most of the retinal haemorrhagic lesions had disappeared. Visual acuity was restored to 25/20 in the right eye and 30/20 in the left eye. However, relative paracentral scotoma persisted in his right eye. Antibody titre to Coxsakievirus B4 had increased, demonstrating a 16-fold rise between the acute (1:8) and convalescent sera (1:128). Retrospectively, we diagnosed the ocular lesions in this patient as uveoretinitis induced by Coxsackievirus B4 infection.
Comment
Viruses are one of the most common causes of infections involving the posterior segment of the eye. Such infections may be congenital or acquired, and may affect primarily the retina or the choroid. Retinitis and choroiditis caused by viruses such as measles, influenza, Epstein-Barr virus, and Rift Valley fever virus typically occur on an acquired basis, subsequent to an acute viral systemic illness. Coxsakievirus associated chorioretinitis is thought to elicit the same clinical course as in other viral chorioretinitis. Coxsackievirus infection and concurrent posterior segment inflammation have been reported in a few cases, in which clinical signs and antibody titres suggested that Coxsackievirus was the responsible agent.1–4 Among them, two cases of chorioretinits associated with Coxsackievirus B4 infection were reported.1,3 One was a paediatric case, and the ophthalmoscopic manifestation was described as scattered white lesions in mid-periphery of the retina.1 The other was an adult case, with chorioretinitis similar to the multiple evanescent white dot syndrome.3 However, the clinical features observed in our patient consisted of iridocyclitis, scattered haemorrhagic dots, and occlusive retinal vasculitis were apparently different from the two earlier reports.
Coxsackievirus infection is apparently a rare cause of uveoretinitis but, nevertheless, should be considered in the appropriate clinical setting, since it is possible that overt clinical manifestations and complications may occur depending on the severity and the location of the uveoretinal lesions.
References
- 1.Hirakata K, Oshima T, Azuma N. Chorioretinitis induced by coxsackievirus B4 infection. Am J Ophthalmol 1990;109:225–7. [DOI] [PubMed] [Google Scholar]
- 2.Forster W, Bialasiewicz AA, Busse H. Coxsackievirus B3-associated panuveitis. Br J Ophthalmol 1993;77:182–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kadrmas EF, Buzney SM. Coxsackievirus B4 as a cause of adult chorioretinitis. Am J Ophthalmol 1999;127:347–9. [DOI] [PubMed] [Google Scholar]
- 4.Haamann P, Kessel L, Larsen M. Monofocal outer retinitis associated with hand, foot, and mouth disease caused by coxsackievirus. Am J Ophthalmol 2000;129:552–3. [DOI] [PubMed] [Google Scholar]