Phenylephrine 10% leads to a faster and more pronounced mydriasis but cardiovascular effects like hypertension and arrhythmias have been reported. In a young healthy adult the upper limit of safety for intravenous administration of phenylephrine is 1.5 mg1 and Kumar et al2 had found phenylephrine plasma levels after administration of topical 10% viscous solution to their patients to be 1.842–11.526 ng/ml after 20 minutes while topical 2.5% aqueous solution produced plasma levels of 0–1.720 ng/ml after 20 minutes. They concluded that the mean pressure tended to be higher with the 10% viscous solution.
Chin et al,3 in their study on 89 patients, concluded that significant hypertensive effects can arise after topical phenylephrine; however, no significant difference between the two groups (2.5% v 10%) was shown. Symons et al4 reported no significant change in the mean systolic and diastolic blood pressure in 126 patients receiving 10% phenylephrine. Malhotra et al5 in their study on 54 cases showed no difference in systemic cardiovascular effects of either the 2.5% or the 10% concentration.
Methods
We carried out a prospective randomised and double masked study on 53 patients undergoing phacoemulsification under topical anaesthesia (Amethocaine 0.1% and Marcaine 0.75%) and no exclusion of cases with hypertension, heart failure, or diabetes was made. All patients received one drop of each of tropicamide 1%, cyclopentolate 1%, and Voltarol 0.1%. Phenylephrine drops, either 2.5% or 10%, were administered in three doses starting half hour before surgery at 5 minute intervals. All patients had their blood pressure measured before dilatation and in the anaesthetic room preoperatively then postoperatively.
Results
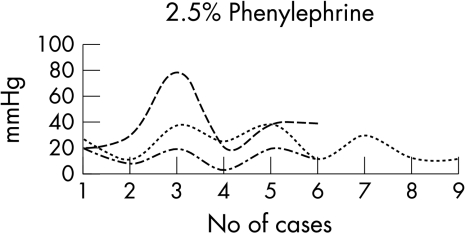
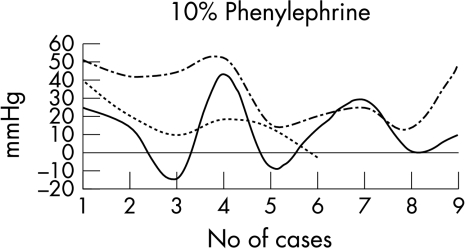
The study included 49 cases aged 52–91, 24 cases were known to have cardiovascular problems and seven were also diabetic. Comparison of the blood pressure changes before dilatation and in the anaesthetic room preoperatively in the 2.5% group (Fig 1 showed a mean rise in systolic BP of 22 mm Hg (p=0.003) in the normotensive group. In the hypertensive group all patients recorded statistically significant rises in systolic and diastolic BP (respectively p=0.010, p=0.009). In the 10% group (Fig 2, 10 patients in the normotensive group showed a mean rise in systolic BP of 34.4 mm Hg (p=0.001) and 10.5 mm Hg in diastolic BP (p=0.077). In the hypertensive group six patients recorded a rise in systolic BP with a mean of 22.8 mm Hg (p=0.015) and a diastolic rise with a mean of 16.8 mm Hg (p=0.033) (Table 1) (Figs 3 and 4).
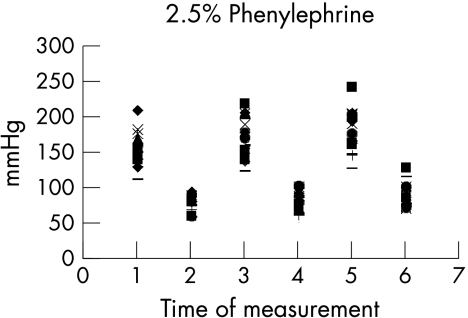
Figure 1.
Blood pressure (mm Hg) with phenylephrine 2.5%. Numbers 1 and 2 = systolic and diastolic reading preanaesthetic; 3 and 4 = systolic and diastolic reading in the anaesthetic room; 5 and 6 = systolic and diastolic reading in recovery.
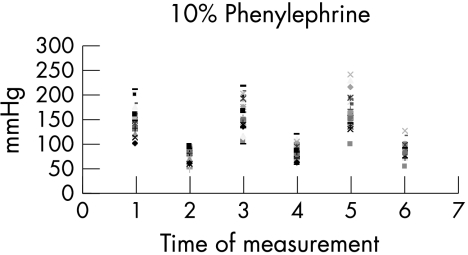
Figure 2.
Blood pressure (mm Hg) with phenylephrine 10%. Numbers 1 and 2 = systolic and diastolic reading preanaesthetic; 3 and 4 = systolic and diastolic reading in the anaesthetic room; 5 and 6 = systolic and diastolic reading in recovery.
Table 1.
t Test 2.5% and 10% (normotesives and hypertensives)
| Mean | SD | Significance* | |
| Normotensive/sys | −12.44 | 19.08 | 0.86 |
| Normotensive/diast | 2.88 | 16.64 | 0.61 |
| Hypertensive/sys | 14.16 | 28.36 | 0.27 |
| Hypertensive/diast | −4.16 | 14.00 | 0.49 |
Two tailed t test, comparing the 2.5% group and 10% group both hypertensive and normotensive patients.
*p=0.05.
Figure 3.
Blood pressure (mm Hg) with phenylephrine 2.5% The mean changes to systolic and diastolic BP.
Figure 4.
Blood pressure (mm Hg) with phenylephrine 10% The mean changes to systolic and diastolic BP.
Comment
Our study showed that patients in both groups of phenylephrine doses experienced a rise in systolic blood pressure which was statistically significant; the mean of which is higher in the 10% group. The maximal systolic blood pressure rise is around 10–20 minutes after administration, which corresponds to the time of maximal plasma levels of phenylephrine as demonstrated by other authors,5 but the paired t test failed to show any significance between the results of the groups of either concentration. Postoperative results showed some elevations in systolic and diastolic BP but weren't statistically significant. Using Altman's normogram the study was limited in its power. Although the aim of this study was not designed to investigate the effect of anxiety on systemic blood pressure, this element should be taken into consideration since it is known to elevate the systolic blood pressure. We have also used topical anaesthesia so that adrenaline 1:200 000, which is always included in local anaesthesia, is excluded which might cause elevation of the blood pressure although the concentration is too low for any significant systemic effect.
We therefore recommend the routine use of the 2.5% phenylephrine in ophthalmic surgery and only use 10% solution for cases where the lower concentration may not be as effective.
References
- 1.Fraunfelder FT, Scafidi AF. Possible adverse effects from topical ocular 10% phenylephrine. Am J Ophthalmol 1978;85:447–53. [DOI] [PubMed] [Google Scholar]
- 2.Kumar V, Schoenwald RD, Chien DS, et al. Systemic absorption and cardiovascular effets of phenylephrine eye drops. Am J Ophthalmol 1985;99:180–4. [DOI] [PubMed] [Google Scholar]
- 3.Chin KW, Law NM, Chin MK. Phenylephrine drops in ophthalmic surgery: a clinical study on cardiovascular effects. Med J Malaysia 1994;49:158–63. [PubMed] [Google Scholar]
- 4.Symons RCA, Walland MJ, Kaufman DV. Letter to the editor. Eye 1997;11:946–7. [DOI] [PubMed] [Google Scholar]
- 5.Malhotra R, Banerjee G, Brampton W, et al. Comparison of the cardiovascular effects of 2.5% phenylephrine and 10% phenylephrine during ophthalmic surgery. Eye 1998;12:973–5. [DOI] [PubMed] [Google Scholar]