Sarcoidosis is an immune mediated disease that may affect any organ. Scleral involvement has rarely been described with sarcoidosis.1–3 We report on a patient with unilateral nodular anterior scleritis who was found to suffer from sarcoidosis. Here, the clinical and histopathological features are described.
Case Report
A 53 year old white woman had persistent moderate tenderness in her left eye that lasted for several weeks. Visual acuity was 20/20 in both eyes. The slit lamp appearance of the right eye was unremarkable. A scleral nodule in the inferior nasal quadrant was found in the left eye (Fig 1), and a moderate tenderness was determined in this area. The intraocular pressures were within normal ranges. On ophthalmoscopy, the posterior segment of both eyes was normal. The ultrasound images did not indicate posterior scleritis.
Figure 1.
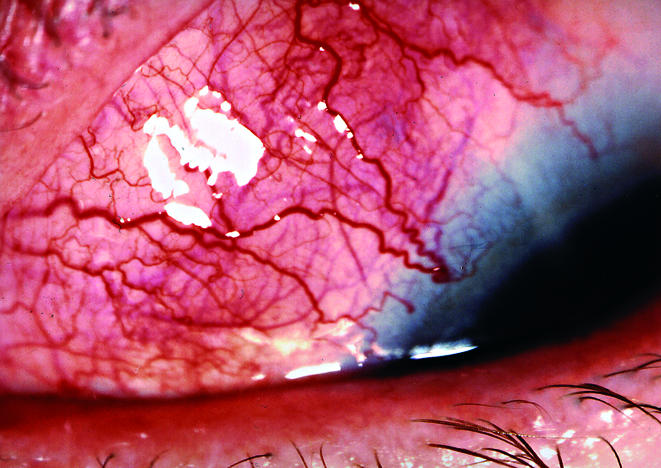
Scleral nodule of the left eye with tenderness in a patient with sarcoidosis.
The medical history was remarkable for an episode of hepatitis A 20 years ago, and the patient suffered from exercise dependent dyspnoea, night sweats, and repeated headaches.
An extensive examination for associated systemic diseases was performed, including serological tests for syphilis, CRP, ESR, ANCA, RF, CIC, ANA, and PPD tests: all were within normal ranges and consultant examinations by the internal medicine, rheumatology, neurology, and ENT departments were performed. The chest x ray examination revealed a bilateral hilar lymphadenopathy and basal interstitial pulmonary infiltration typical of sarcoidosis stage 2. In the body plethysmography, a mild restriction and a moderately reduced diffusion capacity was determined. The bronchoalveolar lavage revealed an increased proportion of CD3+ T cells and an increased CD4/CD8 ratio, consistent with active pulmonary sarcoidosis. The level of angiotensin converting enzyme was 51.3 U/l (normal, 8–52) in the high normal range. The magnetic resonance images revealed an increased enhancement and thickening of the inferior nasal part of the sclera of the left eye.
A biopsy was taken from the scleral nodule under peribulbar anaesthesia. Histopathological studies on the paraffin embedded tissue that was performed by the pathologists revealed a perivascular lymphocytic cell infiltration, with non-caseating granuloma-like cell accumulation (Fig 2). Some histiocytes and very few giant cells were found. The scleral tissue was oedematous and the vessels were dilated, but necrosis, vasculitis or malignant cell configurations were absent. Additionally, Ziehl-Neelson and Gonori's silver methaminamine stains excluded the possibility of causative infections.
Figure 2.
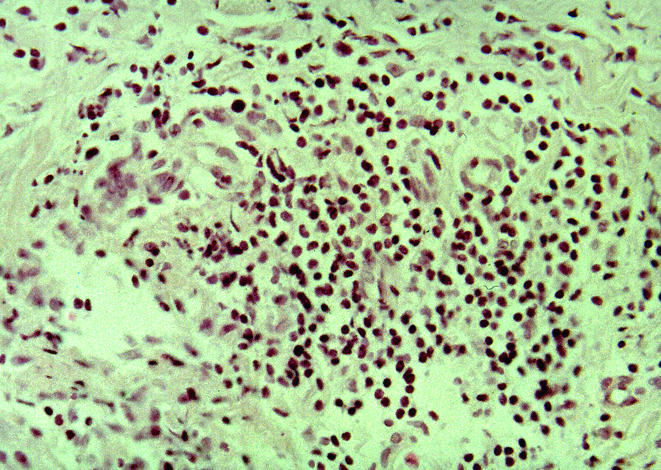
Histopathology of a scleral nodule in a patient with sarcoidosis. The scleral tissue with oedema and vessel dilatation, perivascular lymphocytic cell infiltration with non-caseating granuloma-like cell accumulation, some histiocytes and giant cells. Haematoxylin and eosin staining, magnification, ×200.
Treatment with oral prednisone with an initial dosage of 1 mg/kg was performed. The corticosteroid dosage was tapered within 6 weeks, and was maintained at 20 mg. Under this regimen, the pain and the scleral nodule resolved immediately, and the ACE level fell to 24 U/l (normal).
Comment
Scleral involvement has been previously reported in a few patients with sarcoidosis. In a series of 537 patients with histologically proved sarcoidosis,3 scleral plaques anterior to the equator have been found in four cases, and this was seen in the acute stage of disease and in association with erythema nodosum and bihilar lymphadenopathy. In another series by Jabs and Johns,2 within a group of 183 patients with chronic sarcoidosis, scleral involvement was detected in one patient. However, the clinical course and histopathological appearances have not been described previously. Posterior scleritis has been seen only rarely with sarcoidosis.1
In our patient, the sparse systemic symptoms made the diagnosis difficult and, therefore, scleral biopsy was done in order to rule out infections or malignancies and to disclose the histopathological evidence for sarcoidosis. Although a classic non-caseating granuloma has not been found in our patient, a granuloma-like perivascular cell infiltration was seen, consisting primarily of lymphocytes, some histiocytes, and very few giant cells, which are typical for sarcoidosis. To the best of our knowledge, this is the first histopathological description of a sarcoid lesion in the sclera. The mainstay of treatment for sarcoidosis is corticosteroids, and the scleritis responded in our patient.
Acknowledgments
The authors thank Professor Dr Annette Fisseler-Eckhof, Department of Pathology, Zentralklinik Emil von Behring in Berlin and Professor Dr Christian Witting, Department of Pathology, Clemens Hospital, Muenster for the histopathological evaluation of the tissue specimens.
References
- 1.Dodds EM, Lowder CY, Barnhorst DA, et al. Posterior scleritis with annular ciliochoroidal detachment. Am J Ophthalmol 1995;120:677–9. [DOI] [PubMed] [Google Scholar]
- 2.Jabs DA, Johns CJ. Ocular involvement in chronic sarcoidosis. Am J Ophthalmol 1986;102:297–301. [DOI] [PubMed] [Google Scholar]
- 3.James DG, Neville E, Langley DA. Ocular sarcoidosis. Trans Ophthalmol Soc UK 1976;96:133–9. [PubMed] [Google Scholar]


