Abstract
Aim: To prospectively study the success rate and complications of viscocanalostomy, a non-penetrating glaucoma surgery.
Methods: Prospective non-randomised consecutive case series of 57 eyes (57 patients) with medically uncontrolled primary and secondary open angle glaucoma. Viscocanalostomy was performed on all participants with injection of viscoelastic in the surgically created ostia of Schlemm’s canal as well as in the scleral bed, the superficial scleral flap was loosely sutured. Intraocular pressure, visual acuity, and number of goniopunctures were measured.
Results: The mean follow up period was 34.1 months. The mean preoperative intraocular pressure (IOP) was 24.6 mm Hg; while the mean postoperative IOP was 5.6 mm Hg at day 1 and 13.9 mm Hg at 36 month. Patients who achieved IOP below 21 mm Hg with or without medication were 90% at 60 months, complete success rate (IOP<21 mm Hg without medication) was 60% at 60 months. 21 patients (37%) needed Nd:YAG goniopuncture postoperatively to control raised IOP, mean time for goniopuncture application was 9.4 months, mean pre-goniopuncture IOP was 20.4 mm Hg and mean postgoniopuncture IOP was 12.6 mm Hg (p <0.0001).
Conclusion: Viscocanalostomy appears to be a promising modification of filtering surgery.
Keywords: viscocanalostomy
Viscocanalostomy is a non-penetrating filtration procedure for the surgical treatment of medically uncontrolled open angle glaucoma. The more classic trabeculectomy, with or without antimetabolites, has a well documented complication rate.1–12 Viscocanalostomy was designed in an attempt to lower the risk of incidence of such complications, thus offering both surgeon and patient a safer, more convenient option.13,14
In this report, the experience gained with the procedure has been documented in a prospective, non-randomised study of 68 patients who were operated on between late 1994 and early 1996, and were followed for up to 60 months.
PATIENTS AND METHODS
Setting
The glaucoma unit, Ophthalmology Department, University of Lausanne, Canton of Vaud, Switzerland.
Case selection
Fifty seven eyes of 57 patients with medically uncontrolled primary and secondary open angle glaucoma having viscocanalostomy were consecutively enrolled in this study and followed up prospectively (Table 1). The study patients were enrolled consecutively, after the approval of the ethics committee of the University of Lausanne. Informed consent was obtained from all participants. Patients selected were all medically uncontrolled with maximal medical therapy. Uncontrolled glaucoma was defined as documented progression of glaucomatous visual field defects and glaucomatous optic nerve morphology under maximal tolerable medical treatment.
Table 1.
Patient data (57 patients (57 eyes))
| Demographics | |
| Age (years (SD)) | 71 (11.3) |
| Male/female | 27/30 |
| White/black | 57/0 |
| Preoperative IOP (mm Hg (SD)) | 24.6 (4.9) |
| Preoperative glaucoma medications (SD) | 2.7 (0.8) |
| Follow up (months (SD)) | 34.1 (12.6) |
| POAG | 40 |
| PEXG | 14 |
| PIGG | 3 |
POAG = primary open angle glaucoma; PEXG = pseudoexfoliation glaucoma; PIGG = pigmentary glaucoma.
Exclusion criteria were unwillingness to participate, known allergy to hyaluronic acid, advanced lens opacities, and previous eye surgery or laser trabeculoplasty less than 6 months before enrolment in this study.
Under this definition we have proposed the procedure to consecutive 68 patients, of which 11 where unwilling to participate in a medical trial, and 57 where included.
Data recorded preoperatively
On the day before surgery, patients underwent best corrected visual acuity assessment (Snellen chart at 5 metres), IOP was measured using a Haag-Streit (Bern, Switzerland) Goldmann applanation tonometer mounted on a slit lamp. Patients also underwent biomicroscopy, gonioscopy, visual field testing using the G1 programme of the octopus 101 (Interzeag AG, Schlieren, Switzerland), and fundus biomicroscopy.
Postoperative follow up
After surgery, all the previously mentioned examinations, except for visual field assessment, were conducted on the first and the seventh day as well as at 1, 3, 6, 9, 12, 18, 24, 30, 36, 48, 54, 60, and 66 months. Visual field examination was repeated every 6 months.
Complications have been defined as follows: hyphaema was considered present when erythrocytes were seen in the anterior chamber. Hypotony was defined as a postoperative IOP ≤4 mm Hg for more than 2 weeks. Anterior chamber depth was clinically assessed in comparison with the fellow eye. Anterior chamber was considered shallow when there was an irido-corneal touch in the periphery, and flat when there was a lens-corneal touch, as seen on biomicroscopy. Anterior chamber inflammation was considered to be present when leucocytes could be seen by biomicroscopy. Choroidal detachment was considered present when seen in the peripheral retina, using an indirect ophthalmoscope. In the postoperative follow up, cataract was either observed as a direct consequence of filtration surgery, and termed “surgery related cataract,” or appeared progressively and has therefore been called “cataract progression.” Surgery related cataract has been defined by a rapid decrease (over a period of 1 month) of visual acuity and mainly the development of cortical opacity, whereas cataract progression has been defined as slow progressive decrease in visual acuity of more than two lines (Snellen chart) owing to lens opacification, mainly nuclear sclerosis.
Surgical procedures
All surgeries were performed by one experienced surgeon (AM), using retrobulbar anaesthesia consisting of 2–4 ml of a solution of bupivacaine 0.75%, xylocaine 4%, and hyaluronidase 50 U.
Viscocanalostomy
A superior rectus muscle suture was placed. The conjunctiva and Tenon’s capsule were then opened in the upper fornix and the sclera exposed. Careful haemostasis using wet field cautery was performed. A one third scleral thickness limbus based scleral flap measuring 5 × 5 mm was dissected (Fig 1). This superficial scleral flap was further dissected 1 mm into clear cornea. A triangle or a rectangle of deep sclera was then dissected and removed (Fig 2), leaving a thin layer of deep sclera over the choroids, posteriorly. Anteriorly, the dissection was done reaching Schlemm’s canal, which was unroofed. Moreover, anteriorly, the excision of corneal stroma was done to the level of Descemet’s membrane (Fig 3). At this stage of the procedure, aqueous humour was seen to percolate through the remaining thin trabeculo-Descemet’s membrane (TDM). High viscosity hyaluronic acid was injected into the two surgically created ostia of Schlemm’s canal (Fig 4), aiming at dilating both the ostia and the canal and was also placed in the scleral bed. In classic viscocanalostomy described by Stegmann the superficial scleral flap has to be tightly sutured in order keep the viscoelastic substance in situ, and to force the aqueous percolating through the TDM into the two ostia. In our study the superficial scleral flap was secured with two loose single 10-0 Nylon sutures, and the knots buried. The rationale behind loosely closing the superficial flap will be discussed later. The conjunctiva and Tenon capsule were carefully closed with a running 8-0 Vicryl suture.
Figure 1.
Superficial scleral flap dissection.
Figure 2.
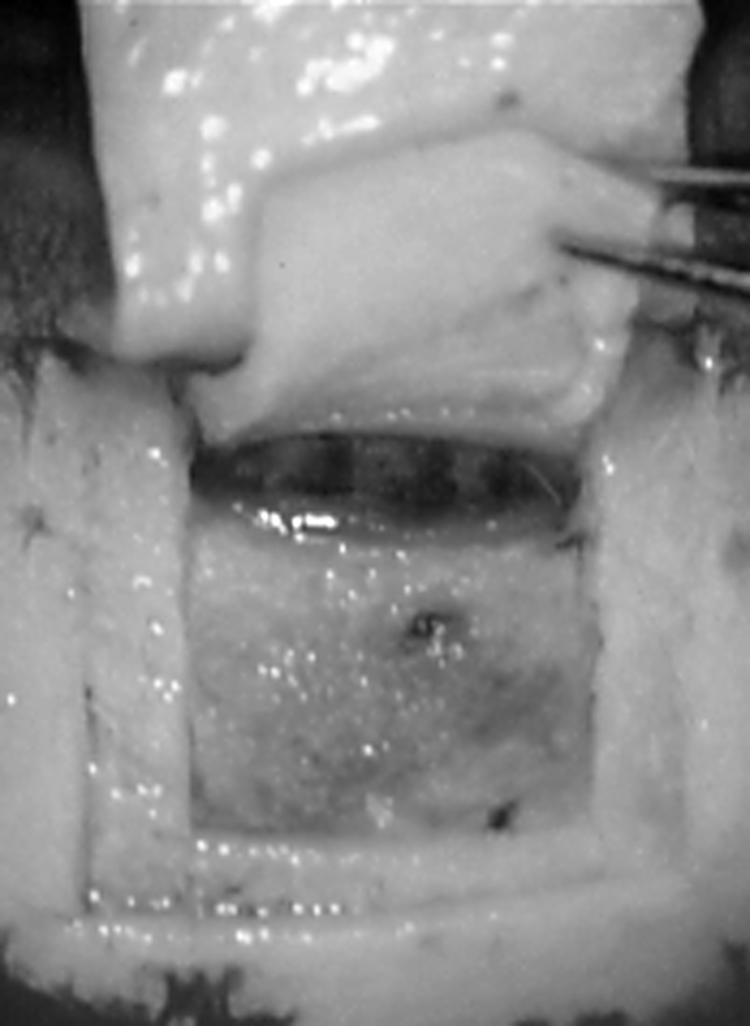
Deep scleral flap dissection.
Figure 3.
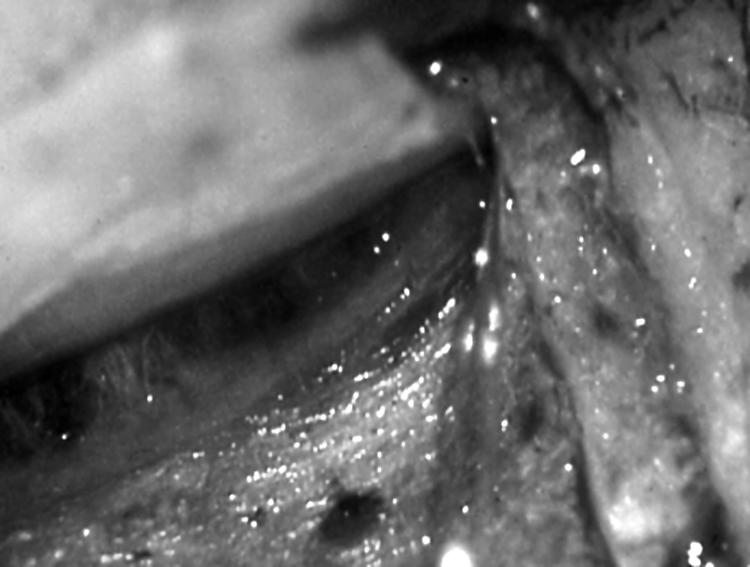
Trabeculo-Descemet’s membrane.
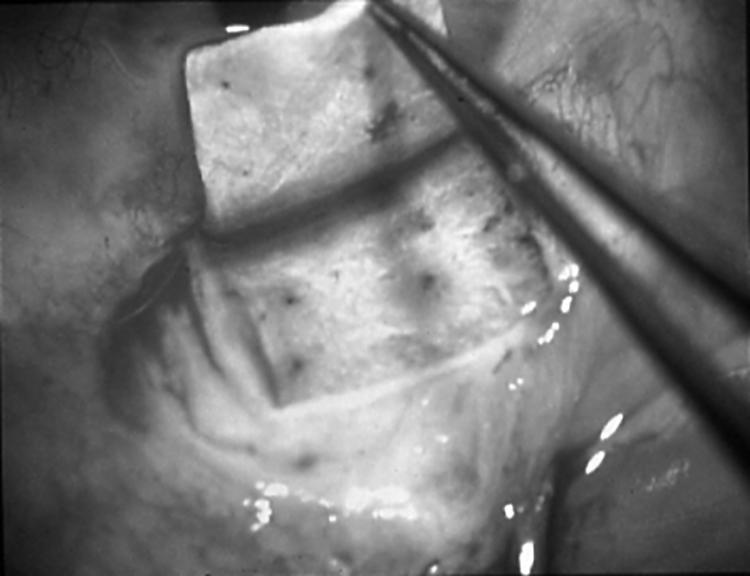
Figure 4.
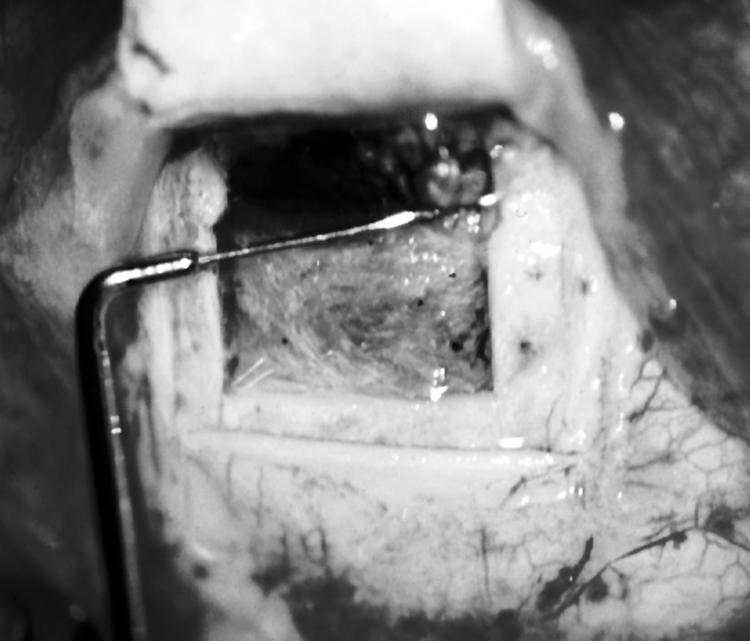
Injection of viscoelastic in the surgically created ostia of Schlemm’s canal.
Postoperatively, patients were treated with topical 0.1% dexamethasone, 0.35% neomycin and 6000 U/ml polymyxin (Maxitrol) three times daily for 2 weeks, and then with topical fluoromethonole three times a day for 3–6 months.
When a perforation of the thin TDM occurred during the corneal stroma dissection, the surgery could be converted into a standard trabeculectomy, with a rectangular resection of the trabeculum, followed by a basal iridectomy. In our series we had no perforations.
Surgery was considered a complete success when IOP was ≤21 mm Hg without glaucoma medication and a qualified success when IOP was ≤21 mm Hg with or without glaucoma medication. It was considered a failure when IOP was >21 mm Hg with or without glaucoma medication, or when an eye required further glaucoma drainage surgery, developed phthisis bulbi or lost light perception. Three measures of the IOP were performed to determine the mean IOP; when this mean was >21 mm Hg, the operation was considered a failure.
When the filtering bleb at any postoperative visit was encysted or showed signs of fibrosis, subconjunctival injections of 5 mg of 5-fluorouracil (5-FU) were administered in the lower quadrant, opposite the viscocanalostomy site. The subconjunctival injections consisted of 0.1 ml of a 50 mg/ml solution of 5-FU (250 mg/5 ml, Roche, Basel, Switzerland). Subconjunctival 5-FU injections were repeated up to seven times, when necessary.
Goniopuncture with the Nd:YAG laser (Microruptor II, Lasag AG, Thun, Switzerland) was performed when the filtration through the TDM was suspected to be insufficient, either because of a shallow filtration bleb or elevated IOP. The laser treatment was performed using a Lasag-15 gonioscopy contact lens (CGA1). Goniopuncture was performed using the free running Q-switch mode with energy ranging from 2–4 mJ. Two to eight shots were aimed at the TDM. The goal of the laser treatment was to create a small hole in the TDM, which is technically similar to posterior capsulotomy after cataract surgery. Goniopuncture allows direct passage of aqueous humour from the anterior chamber to the filtration bleb transforming the non-perforating filtering surgery into a perforating filtering surgery. After laser treatment, patients were treated with topical prednisolone acetate (Predforte) three times a day for 3 days. Laser goniopuncture was considered a success when final IOP was <18 mm Hg, or when the decrease in IOP was >5 mm Hg with initial pressure of ≤23 mm Hg.
RESULTS
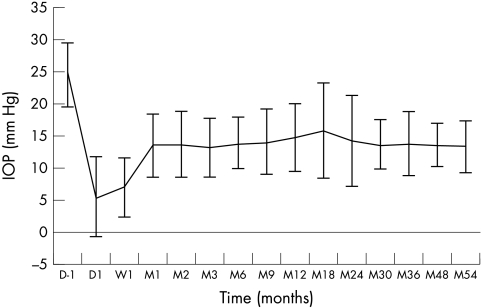
Mean follow up period was 34.1 (SD 11) months. The mean preoperative IOP was 24.6 (SD 4) mm Hg. The mean IOP at the first postoperative day was 5.6 (SD 6) mm Hg. The IOP at 3 months was reduced by 46.1% (13 (SD 3) mm Hg versus 24 mm Hg), and at 48 months IOP was reduced by 44.6% (13 (SD 4) mm Hg versus 24.4 mm Hg) thus showing stability of IOP postoperatively (Fig 5).
Figure 5.
Intraocular pressure before and after viscocanalostomy. Vertical error bars represent ±1 SD.
Complete success rate, defined as IOP lower than 21 mm Hg without medication, was 60% (34/57 patients) at 60 months (Fig 6). Qualified success rate, patients who achieved IOP below 21 mm Hg with and without medication, was 90% (51/57 patients) at 60 months. Patients with an IOP lower than 21 mm Hg with medication were 30% at 60 months. The mean number of medications per patient was reduced from 2.7 (SD 0.76) to 0.94 (SD 0.72) after viscocanalostomy.
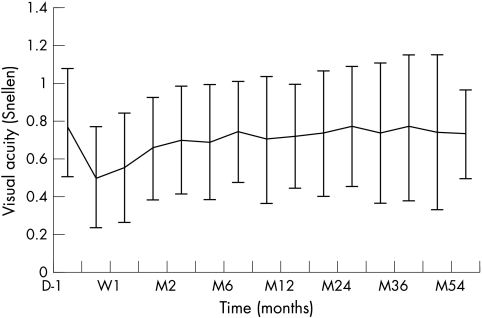
Figure 6.
Evolution of the mean visual acuity after viscocanalostomy. Vertical error bars represent ±1 SD.
Patients were further divided into group A (<21 mm Hg without treatment) and group B (<21 mm Hg with treatment).
Group A was further subdivided into three categories: IOP between 19 and 21 mm Hg two patients (3.5%); IOP between 16 and 18 mm Hg eight patients (14%); and 15 mm Hg or less 24 patients (71% of group A, and 42% of the whole series).
Group B was subdivided in the same fashion to IOP between 19 and 21 mm Hg, three patients (17%), IOP between 16 and 18 mm Hg five patients (29%); and IOP 15 mm Hg or less nine patients (53%).
Of the 57 eyes on which viscocanalostomy was performed, six failed to achieve complete or qualified success criteria and were considered failures. Four patients had primary open angle glaucoma and two suffered from pseudoexfoliative glaucoma. Mean preoperative IOP was 27 mm Hg, mean time to failure was 24 months. At 24 months the mean IOP was 27 mm Hg. One patient developed neovascular glaucoma and his pressure was not controlled, a glaucoma drainage device was needed to control IOP below 21 mm Hg. Another patient developed central retinal artery occlusion and his visual acuity dropped to perception of light, while four other patients were thought to have excessive fibrosis and they were reoperated (two deep sclerectomy with collagen implant, and two trabeculectomies with mitomycin C).
Best corrected visual acuity (BCVA) dropped on the first postoperative day from a mean of 0.79 (SD 0.28) preoperatively, to a mean of 0.50 (SD 0.26). Visual acuity returned to preoperative levels 1 week after surgery and remained stable over the next 5.5 years achieving a mean BCVA of 0.77 (SD 0.31) at 24 months and 0.76 (SD 0.38) at 36 months (Fig 6).
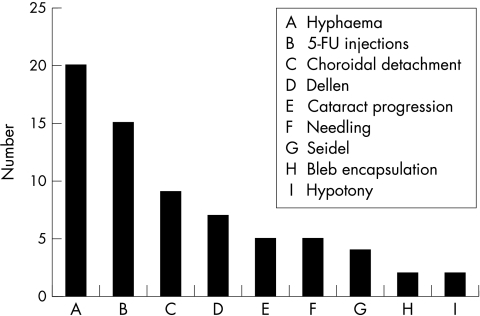
There were no significant operative complications recorded in this series. Postoperative complications that occurred are given in Figure 7. No shallow or flat anterior chamber, no bleb related endophthalmitis, and no surgery induced cataract were observed. However, five patients (8.7%) showed a progression of pre-existing senile cataract. Bleb fibrosis and encapsulation were treated with 5-FU subconjunctival injections. Injections of 5-FU were performed on 15 patients who underwent viscocanalostomy. The mean number of injections was 2.1 (SD 1.4) and the mean time between operation and 5-FU injection was 1.6 (SD 1.4) months.
Figure 7.
Postoperative complications.
Goniopuncture with ND:YAG laser was performed on 21 patients (37%). The mean time between viscocanalostomy and laser was 9.4 (SD 9) months, the mean IOP before goniopuncture was 20.4 (SD 6), and the mean IOP after goniopuncture was 12.6 (SD 6). This difference was statistically significant (p <0.0001).
DISCUSSION
Classic glaucoma teachings consider surgery to be a last resort for the treatment for primary open angle glaucoma, after the failure of topical therapy and argon laser trabeculoplasty (ALT) in controlling IOP.15
Recent data from the Advanced Glaucoma Intervention Study (AGIS)16 has cast doubt over this classic approach. The AGIS revealed a race related response to ALT, which argues for trabeculectomy before ALT in white people. Such data clearly are at odds with the classic approach of surgery as last resort intervention.
Most surgeons prefer to delay surgery because of the potential vision threatening complications of classic trabeculectomy, with or without antimetabolites. Complications include hypotony, hyphaema, flat anterior chamber, choroidal effusion or haemorrhage, surgery induced cataract, and bleb failure.1–12
In spite of the tendency to delay surgery, it remains a very effective way of lowering IOP. Bylsma15 hypothesises that if the safety margin of glaucoma surgery could be increased significantly without sacrificing efficacy, surgical intervention for glaucoma might be considered earlier.
In an attempt to avoid the numerous postoperative complications of trabeculectomy, some authors17 proposed a tight closure of the scleral flap with secondary suture lysis using argon laser. More recently, for the same reason, several techniques of non-perforating filtration surgery have been described. Zimmerman et al18,19 reported positive results of non-penetrating trabeculectomy in phakic and aphakic patients. Arenas20 developed a technique called ab externo trabeculectomy, and reported a success rate of 88%. Other authors who used the ab externo technique reported control of IOP in 85.8% to 90% of patients.21–23 Stegmann13,14 was the first to describe viscocanalostomy, in which the scleral space was filled with a viscoelastic substance, and reported complete success of 82.7% and qualified success in 89.0% of patients at 35 months of follow up.
The major advantage of viscocanalostomy is that it precludes the sudden hypotony that occurs following trabeculectomy by creating progressive filtration of aqueous humour from the anterior chamber to the subconjunctival space, thus avoiding sudden decompression of the eye ball. In an experimental model, Vaudaux and Mermoud24 studied the aqueous dynamics through the remaining thin TDM, and found that the outflow resistance was low but sufficient enough to avoid the immediate postoperative complications often seen after trabeculectomy.
Stegmann14 published his results of performing viscocanalostomy on black African patients suffering from open angle glaucoma. This prospective study was performed on 214 patients who were poorly controlled by medical therapy. Stegmann reported an IOP of 22 mm Hg or less in 82.7% of eyes without medical therapy (complete success rate). His qualified success rate was 89.0%. With a mean follow up of 35 months, this study clearly shows that IOP could, and is, controlled satisfactorily with viscocanalostomy, a non-penetrating glaucoma surgery.
In a similar study Carrassa et al25 performed viscocanalostomy on 33 patients and achieved a complete success rate of 86.2 %. In spite a much shorter mean follow up (3.0 months SD 2.6), Carrassa’s results were comparable to Stegmann’s.
In another prospective study by Carrassa,26 he compared two groups of randomised patients, one group had trabeculectomy and the other viscocanalostomy. Each group included 25 patients of comparative male/female ratio and mean age. He concluded that although viscocanalostomy has a less significant rate of complications, in terms of incidence and gravity, trabeculectomy achieved lower mean IOP.
In Stegmann’s description of viscocanalostomy, the superficial flap should be tightly closed, thus forcing the percolating aqueous through the two cut ends of Schlemm’s canal. Although we acknowledge that aqueous drainage through the surgically created ostia, may well be one of the methods of drainage, it is not the only one. Various studies (Kasakova and Mermoud, unpublished data) have examined aqueous humour resorption following non-penetrating glaucoma surgery, and they have concluded that aside from the Schlemm’s canal route, aqueous is resorbed through subconjunctival blebs, intrascleral blebs, and through the subchoroidal space. To tightly close the superficial flap would lower the chances of function for other routes.
Except for the first week after surgery, visual acuity was unaffected by viscocanalostomy. This phenomenon may be explained by the non-perforation of the eye, which avoids inflammation, use of mydriatics, and sudden hypotony. Furthermore, visual acuity remained stable because no surgery related cataracts developed after viscocanalostomy.
In our series, patients who developed fibrosis or an encysted bleb were treated with subconjunctival injections of 5-FU. The mean number of injections required per patient (2.9 (SD 1.9)), was much lower than in previous studies using 5-FU after trabeculectomies (7–21 injections).27 The majority of 5-FU injections were made during the first two postoperative months.
Goniopunctures with the Nd:YAG laser were performed in 33.8% of the patients (23 patients). Goniopuncture was performed shortly after viscocanalostomy if there was insufficient percolation of aqueous humour at the TDM probably because of the lack of surgical dissection. When goniopunctures were required at a later time (more than 9 months after initial surgery), low filtration was probably the result of fibrosis of the TDM,28 since goniopuncture resulted in increased filtration of aqueous humour and decreased IOP. The success rate of Nd:YAG laser goniopuncture was satisfactory, with an immediate reduction in mean IOP of 39.5 % (from 21.3 (SD 6.15) to 13.1 (SD 6.5) mm Hg). By opening the TDM; however, goniopuncture transformed a non-perforating filtration procedure into a perforating one. Although the potential risk of late bleb related endophthalmitis may be increased after goniopuncture, no such case occurred during the study.28
The early postoperative complications included the presence of subtle hyphaema in 20 of our cases. The very small amount of blood in the anterior chamber can be explained by a probable blood reflux from the scleral bed through the anterior trabeculum, or by undetected microperforations.28
In conclusion, viscocanalostomy appears to be a promising non-perforating filtration procedure. In our experience, the success rate after 5 years of follow up was satisfactory for all types of primary and secondary open angle glaucoma studied. The immediate postoperative complication rate was low, and visual acuity was almost unaffected.
REFERENCES
- 1.Watson PG, Jakeman C, Ozturk M, et al. The complications of trabeculectomy (a 20-year follow-up). Eye 1990;4:425–38. [DOI] [PubMed] [Google Scholar]
- 2.Kao SF, Lichter PR, Musch DC. Anterior chamber depth following filtration surgery. Ophthalmic Surg 1989;20:332–6. [PubMed] [Google Scholar]
- 3.Stewart WC, Shields MB. Management of anterior chamber depth after trabeculectomy. Am J Ophthalmol 1988;106:41–4 [DOI] [PubMed] [Google Scholar]
- 4.Brubaker RF, Pederson JE. Ciliochoroidal detachment. Surv Ophthalmol 1983;27:281–9. [DOI] [PubMed] [Google Scholar]
- 5.Gressel MG, Parrish RK II, Heuer DK. Delayed nonexpulsive suprachoroidal hemorrhage. Arch Ophthalmol 1984;102:1757–60. [DOI] [PubMed] [Google Scholar]
- 6.Ruderman JM, Harbin TS Jr, Campbell DG. Postoperative suprachoroidal hemorrhage following filtration procedures. Arch Ophthalmol 1986;104:201–5. [DOI] [PubMed] [Google Scholar]
- 7.Freedman J, Gupta M, Bunke A. Endophthalmitis after trabeculectomy. Arch Ophthalmol 1978;96:1017–18. [DOI] [PubMed] [Google Scholar]
- 8.Zaidi AA. Trabeculectomy: a review and 4-year follow-up. Br J Ophthalmol 1980;64:436–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akafo SK, Goulstine DB, Rosenthal AR. Long-term post trabeculectomy intraocular pressures. Acta Ophthalmol (Copenh) 1992;70:312–6 [DOI] [PubMed] [Google Scholar]
- 10.Mills KB. Trabeculectomy: a retrospective long-term follow-up of 444 cases. Br J Ophthalmol 1981;65:790–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Molteno AC, Bosma NJ, Kittelson JM. Otago glaucoma surgery outcome study: long-term results of trabeculectomy–1976 to 1995. Ophthalmology 1999;106:1742–50. [DOI] [PubMed] [Google Scholar]
- 12.D’Ermo F, Bonomi L, Doro D. A critical analysis of the long-term results of trabeculectomy. Am J Ophthalmol 1979;88:829–35. [DOI] [PubMed] [Google Scholar]
- 13.Stegmann RC. Visco-canalostomy: a new surgical technique for open angle glaucoma. An Inst Barraquer, Spain 1995;25:229–32. [Google Scholar]
- 14.Stegmann R, Pienaar A, Miller D. Viscocanalostomy for open-angle glaucoma in black African patients. J Cataract Refract Surg 1999;25:316–22. [DOI] [PubMed] [Google Scholar]
- 15.Bylsma S. Nonpenetrating deep sclerectomy: collagen implant and viscocanalostomy procedures. Int Ophthalmol Clin 1999;30:103–19. [DOI] [PubMed] [Google Scholar]
- 16.AGIS authors. The Advanced Glaucoma Intervention Study (AGIS): 4. Comparison of treatment outcomes within race. Seven-year results. Ophthalmology 1998;105:1146–64. [DOI] [PubMed] [Google Scholar]
- 17.Savage JA, Condon GP, Lytle RA, et al. Laser suture lysis after trabeculectomy. Ophthalmology 1988;95:1631–8. [DOI] [PubMed] [Google Scholar]
- 18.Zimmerman TJ, Kooner KS, Ford VJ, et al. Effectiveness of nonpenetrating trabeculectomy in aphakic patients with glaucoma. Ophthalmic Surg 1984;15:44–50. [PubMed] [Google Scholar]
- 19.Zimmerman TJ, Kooner KS, Ford VJ, et al. Trabeculectomy vs non-penetrating trabeculectomy: a retrospective study of two procedures in phakic patients with glaucoma. Ophthalmic Surg 1984;15:734–40. [PubMed] [Google Scholar]
- 20.Arenas E. Trabeculectomy ab-externo. Highlights of Ophthalmology 1991;19:59–66. [Google Scholar]
- 21.Gierek A, Szymanski A. Results of deep sclerectomy for open-angle glaucoma. Folia Ophthalmol (Leipzig) 1987;12:227–9. [Google Scholar]
- 22.Tavano G, Chabin T, Barrut JM. Hémitrabéculectomie ab externo non invasive. Bull Soc Ophtalmol Fr 1993;93:749–50. [Google Scholar]
- 23.Tanihara H, Negi A, Akimoto M, et al. Surgical effects of trabeculotomy ab externo on adult eyes with primary open angle glaucoma and pseudoexfoliation syndrome. Arch Ophthalmol 1993;111:1653–61. [DOI] [PubMed] [Google Scholar]
- 24.Vaudaux J, Uffer S, Mermoud A. Aqueous dynamics after deep sclerectomy: In vitro study. Ophthalmic Practice 1998;16:204–9. [Google Scholar]
- 25.Carassa RG, Bettin P, Brancato R. Viscocanalostomy: a pilot study. Acta Ophthalmol Scand Suppl 1998;227:51–2. [DOI] [PubMed] [Google Scholar]
- 26.Carassa RG, Bettin P, Fiori M, et al. Viscocanalostomy: a pilot study. Eur J Ophthalmol 1998;8:57–61. [DOI] [PubMed] [Google Scholar]
- 27.The Fluorouracil Filtering Surgery Study Group. Fluorouracil filtering surgery study one-year follow-up. Am J Ophthalmol 1989;108:625–35. [DOI] [PubMed] [Google Scholar]
- 28.Lachkar Y, Hamard P. Non penetrating filtering surgery. Curr Opin Ophthalmol 2002;13:110–15. [DOI] [PubMed] [Google Scholar]