Abstract
Background: It has been reported that exposure to artificial lighting at night during the first 2 years of life was very strongly associated with subsequent myopia development.
Methods: The strength of this association was tested in a UK sample for the first time. The study population comprised 122 university students.
Results: Myopia occurred with approximately equal frequency in those who slept with and without light exposure at night. In contrast, two largely genetic factors, parental myopia and race, were both significantly associated with myopia development, as has been found previously.
Conclusion: This study provides further support for the view that night-time light exposure during infancy is not a major risk factor for myopia development in most population groups. In a subset of this cohort for which spectacle prescriptions were available for both parents (49 trios), the heritability of ocular refraction was estimated to be 0.31.
Keywords: myopia, genetics, ambient lighting
Both genetic and environmental factors are implicated in the aetiology of myopia.1 Historically, near work activity—for example, reading, has been considered the most important environmental risk factor,2 although two comprehensive genetic studies have recently suggested that additive genetic factors are responsible for over 80% of the variation in refractive error in European populations,3,4 leaving only a minor component that could be due to environmental factors to which people are variably exposed. However, Quinn and co-workers5 have reported an association between night-time light exposure during the first 2 years of childhood and subsequent myopia development (in a US population group attending a university paediatric ophthalmology outpatient clinic) the magnitude of which was so strong that it would be expected to dominate genetic factors in the aetiology of myopia. Interestingly, the disruption of normal diurnal lighting rhythms is known to alter refractive development in chickens6–9 resulting in eyes with flatter corneas, shallower anterior chambers, and deeper vitreous chambers (with this latter effect possibly being an emmetropisation response to the anterior segment changes). However, these chick studies would predict that continuous light exposure would predispose to hyperopia rather than myopia, and Smith et al10 have recently found that in rhesus monkeys continuous light exposure does not induce the dramatic changes in refractive development seen in chicks. In addition, three studies (two in the United States, one in Singapore and China) have failed to replicate the findings of Quinn et al in human populations.11–13 We tested the strength of the association between night-time lighting and myopia development in a UK sample for the first time.
METHODS
Subjects aged between 18–40 inclusive were recruited from the Cardiff University student population, via advertisements describing the study. Criteria for exclusion were a history of keratoconus, connective tissue disease, cataract, or refractive surgery. Subjects underwent cycloplegic autorefraction on the right eye. Their parents were sent a questionnaire inquiring whether the subject had slept in darkness, with a night light, or with the room light on, before the age of 2 years, using the questions of Quinn et al.5 Parents were asked about their own use of spectacles or contact lenses using the “indirect method” questions of Walline and co-workers,14 and where possible, the spectacle prescription of each parent was obtained from their optometrist (when these were worn). In cases where the prescription was not available, the classification of parents as myopic or non-myopic was determined from their questionnaire responses as described by Walline et al.14 Myopia was defined as a mean spherical equivalent of ≤−0.50 D, as described by Quinn et al.5 All data were analysed for right eyes only, as ocular refraction is known to be highly correlated between fellow eyes of the same subject.4
In all, 122 subjects participated in the study (mean age 21.6 years, range 19–36 years, 71% female, 66% white, 34% Asian). No subject had to be excluded. Parental refractive status (myopic versus non-myopic) could be determined from questionnaires for both parents of 81 subjects and for at least one parent of a further 29 subjects. Refractive details were obtained for both parents of 49 subjects and for at least one parent of a further 31 subjects. Ethical approval for this project was obtained from the local research ethics committee and all subjects and their parents provided informed consent. Fisher’s exact test and the χ2 test were used for the statistical evaluation of 2 × 2 and 3 × 2 contingency tables, respectively. Heritability was calculated from the regression of offspring values for mean sphere on “mid-parent” values.15
RESULTS
In this UK sample there was no significant association between night-time light exposure and myopia (Table 1A; χ2, p=0.21). This remained the case when subjects in the “night lights” and “room lights” groups were pooled, and the data were analysed in the form of a simplified 2 × 2 contingency table—specifically, the presence/absence of myopia in subjects who had/had not received light exposure at night during infancy (Table 1B; Fisher’s, p=0.12). (Since the χ2 test sometimes performs poorly when cells contain values <5 the latter test is likely to be more reliable than the former.) When the data collected by Quinn et al5 were re-analysed in this simplified 2 × 2 table manner it retained its high statistical significance (p<0.0001). The current study had 95% power to detect an effect of similar magnitude.16
Table 1.
Number of subjects with myopia as a function of night-time light exposure during first 2 years of life
| A | Darkness | Night light | Room light |
| Subject not myopic | 22 | 20 | 2 |
| Subject myopic | 51 | 23 | 4 |
| B | Darkness at night | Light exposure at night |
| In (B) the data from the night light and room light groups are pooled. Note that while not statistically significant, myopia was more common in subjects who slept in darkness during infancy. | ||
| Subject not myopic | 22 | 22 |
| Subject myopic | 51 | 27 |
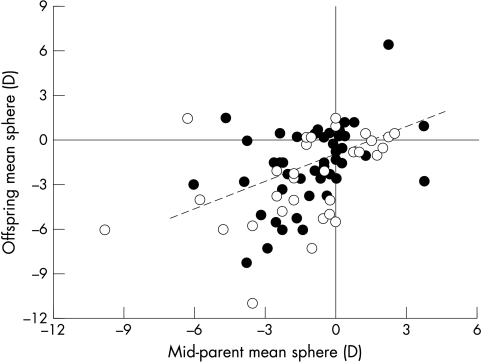
Myopia was equally prevalent between the two sexes (Table 2A; Fisher’s, p=1.0), but was more common in Asians (Table 2B; Fisher’s, p=0.005) and in those with at least one myopic parent (Table 3; Fisher’s, p=0.02). There was a significant correlation between the refractive error of subjects and their parents (Fig 1; p<0.0001). This relation provided a heritability estimate15 for ocular refraction of 0.31 (95% confidence interval 0.14 to 0.50) for the 49 families for which data were available for both parents.
Table 2.
Number of subjects with myopia as a function of their sex (A) and ethnicity (B)
| A | Male | Female |
| Subject not myopic | 13 | 31 |
| Subject myopic | 22 | 56 |
| B | White | Asian |
| Subject not myopic | 36 | 8 |
| Subject myopic | 44 | 34 |
Table 3.
Number of subjects with myopia as a function of parental myopia
| A | Neither parent myopic | Either parent myopic |
| Subject not myopic | 20 | 15 |
| Subject myopic | 17 | 39 |
Figure 1.
Correlation in ocular refraction between parents and offspring. All data are from right eyes only. Mid-parent values are the average mean spherical equivalent for both parents (solid symbols; n=49), or the value for a single parent when a prescription was available for only one parent (open symbols; n=31). Spearman correlation coefficient r = 0.482 (n=80; p<0.0001). The broken line shows the linear regression (b=0.31) for the 49 families for which data were available for both parents.
DISCUSSION
In this UK sample there was no evidence of an association between night lights and myopia. A similar conclusion was drawn from studies in the United States by Gwiazda et al11 and Zadnik et al.12 However, in subjects from Singapore and China, Saw and co-workers13 did find a weak association between night lights and myopia that almost reached statistical significance, and in a very recent study, Loman et al17 found a significant association between myopia and the number of hours of complete darkness to which young adults were currently exposed at night.
The population studied here had a higher prevalence of myopia (64%) and a lower prevalence of hyperopia than the general population (see distribution of offspring mean spheres in Fig 1) suggesting a source of ascertainment bias. As has been noted previously,11 given that the subjects studied by Quinn et al1 were aged between 2–16 years, they showed a similar high prevalence of myopia (with 30% of subjects myopic). Although a myopia prevalence of 64% is typical of university students,17 our study was also likely to have been affected by response bias, with more myopes choosing to participate than non-myopes. Such selection and response biases have the potential to either inflate or mask the effect being investigated.18,19 By selecting subjects attending a university paediatric ophthalmology clinic, the population studied by Quinn et al5 is likely to have suffered from a different source of selection bias, but possibly a similar response bias.
In contrast with the lack of an effect from night lights, this study once again confirms the higher prevalence of myopia in Asians compared to Europeans, and the influence of parental myopia in determining the refractive errors of their children.1 However, the heritability estimate obtained here (0.31) is much lower than that obtained in two careful twin studies that were carried out recently3,4 both of which used considerably more subjects than were included in the present investigation (n=506 and 114 twin pairs, respectively). We speculate that several factors might have contributed to this difference. Firstly, our heritability has wide confidence intervals and thus could be a considerable underestimate (and while the linear regression residuals for the calculation do not show a significant deviation from normality, the sample is too small to provide a robust test of this). Secondly, our subjects had a more varied ethnicity, and a higher proportion of high myopes, compared to those examined in the two twin studies. Thirdly, our heritability estimate is subject to a source of bias, since emmetropic parents would be less likely to wear spectacles, and thus would have been excluded from our analysis. Finally, because twin studies make the assumption that “common environment” effects are independent of zygosity, they tend to overestimate heritability in comparison with population studies.20
In conclusion, our results suggest that night-time light exposure played a lesser part than genetic factors in the myopia development of this UK student population.
Acknowledgments
We would like to thank the participating subjects, parents, and optometrists for their assistance. Many thanks also to Jane Farbrother and Ruth Stewart for their valuable criticisms and suggestions.
REFERENCES
- 1.Bear JC. Epidemiology and genetics of refractive anomalies. In: Grosvenor T, Flom MC, eds. Refractive anomalies: research and clinical applications. Stoneham, MA: Butterworth-Heinemann, 1991.
- 2.Goldschmidt E. On the etiology of myopia. Acta Ophthalmol 1968;(suppl):98. [PubMed]
- 3.Hammond CJ, Snieder H, Gilbert CE, et al. Genes and environment in refractive error: the twin eye study. Invest Ophthalmol Vis Sci 2001;42:1232–6. [PubMed] [Google Scholar]
- 4.Lyhne N, Sjolie AK, Kyvik KO, et al. The importance of genes and environment for ocular refraction and its determiners: a population based study among 20–45 year old twins. Br J Ophthalmol 2001;85:1470–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quinn GE, Shin CH, Maguire MG, et al. Myopia and ambient lighting at night. Nature 1999;399:113. [DOI] [PubMed] [Google Scholar]
- 6.Lauber JK, Kinnear A. Eye enlargement in birds induced by dim light. Can J Ophthalmol 1979;14:265–9. [PubMed] [Google Scholar]
- 7.Weiss S, Schaeffel F. Diurnal growth rhythms in the chicken eye: relation to myopia development and retinal dopamine levels. J Comp Physiol A 1993;172:263–70. [DOI] [PubMed] [Google Scholar]
- 8.Boelen MK, Cottriall CL. Nightlights affect diurnal cycling of dopamine release and the rate of emmetropisation. Invest Ophthalmol Vis Sci 2000;41:S134. [Google Scholar]
- 9.Li T, Howland HC. Modulation of constant light effects on the eye by ciliary ganglionectomy and optic nerve section. Vision Res 2000;40:2249–56. [DOI] [PubMed] [Google Scholar]
- 10.Smith EL, Bradley DV, Fernandes A, et al. Continuous ambient lighting and eye growth in primates. Invest Ophthalmol Vis Sci 2001;42:1146–52. [PubMed] [Google Scholar]
- 11.Gwiazda J, Ong E, Held R, et al. Myopia and ambient night-time lighting. Nature 2000;404:144. [DOI] [PubMed] [Google Scholar]
- 12.Zadnik K, Jones LA, Irvin BC, et al. Myopia and ambient night-time lighting. Nature 2000;404:143–4. [DOI] [PubMed] [Google Scholar]
- 13.Saw SM, Zhang MZ, Hong RZ, et al. Near-work activity, night-lights, and myopia in the Singapore-China study. Arch Ophthal 2002;120:620–7. [DOI] [PubMed] [Google Scholar]
- 14.Walline JJ, Zadnik K, Mutti DO. Validity of surveys reporting myopia, astigmatism, and presbyopia. Optom Vis Sci 1996;73:376–81. [DOI] [PubMed] [Google Scholar]
- 15.Falconer DS. Heritability. In: Introduction to quantitative genetics. Harlow, Essex: Longman, 1989:163–86.
- 16.Altman DG. Sample size in clinical trials, In: Practical statistics for medical research. Boca Raton: Chapman and Hall, 1991:455–60.
- 17.Loman J, Quinn GE, Kamoun L, et al. Darkness and near work: myopia and its progression in third-year law students. Ophthalmology 2002;109:1032–8. [DOI] [PubMed] [Google Scholar]
- 18.Appen RE, Mares-Perlman J. Are the sky and night lights falling? Arch Ophthalmol 2000;118:701–2. [DOI] [PubMed] [Google Scholar]
- 19.Fredrick DR. Myopia: was mother right about reading in the dark? Br J Ophthalmol 2001;85:509–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hopper JL. Why ‘common environment’ effects are so uncommon in the literature. In: Spector TD, Snieder H, MacGregor AJ, eds. Advances in twin and sib-pair analysis. London: Greenwich Medical Media, 2000:151–65.