Abstract
Aim: To evaluate the value of using perfluorocarbon liquid (PFCL) during vitrectomy in eyes with proliferative diabetic retinopathy (PDR).
Methods: The surgical records of eyes with PDR (291 eyes of 228 patients) that underwent vitrectomy in the vitreoretinal service of Osaka Medical College (April 1999 to October 2001) were reviewed. From these, 18 eyes of 15 patients had PFCL used during vitrectomy, and the preoperative and postoperative findings of these eyes were analysed.
Results: All of the 18 eyes had advanced PDR with tractional and/or rhegmatogenous retinal detachment. PFCL enabled easier flattening of the retinal folds and effective endophotocoagulation. In two cases, PFCL was used to flatten a bullous retinal detachment that developed when a tight vitreoretinal adhesion was loosened. In two other cases with combined traction/rhegmatogenous retinal detachment, PFCL was used to tamponade the detached retina which then allowed successful membrane dissection. Anatomical success was obtained in 16 of the 18 cases (mean follow up time 13.3 months) with visual acuity of 20/200 or better in nine eyes (50%).
Conclusions: PFCL is considered to be a useful adjunct during vitrectomy for the treatment of severe PDR.
Keywords: perfluorocarbon liquid, proliferative diabetic retinopathy
Perfluorocarbon liquid (PFCL) is colourless and odourless, and has a high density and low viscosity. The intraoperative use of PFCL in vitreoretinal surgery was introduced in 1987 by Chang for the treatment of giant retinal tears, retinal detachments with proliferative vitreoretinopathy (PVR), and traumatic retinal detachments.1–6 Recently, PFCL has also been used to reposition dislocated crystalline lenses and implanted intraocular lenses (IOLs).7–10 PFCL has also been used when a subretinal haemorrhage is removed during surgery for complicated age related macular degeneration.11,12
In our hospital, PFCL has been used during vitrectomy for advanced proliferative diabetic retinopathy (PDR) with tractional and/or rhegmatogenous retinal detachment. We have reviewed the surgical records and identified 18 eyes of 15 patients with severe PDR that had received PFCL during vitrectomy. We shall present representative cases and demonstrate the usefulness of PFCL during vitrectomy for advanced PDR.
PATIENTS AND METHODS
Patients were identified by searching the surgical records of the vitreoretinal service of department of ophthalmology, Osaka Medical College from April 1999 to October 2001. Vitrectomy was performed on 291 eyes of 228 diabetic patients by five vitreoretinal surgeons (YI, MM, MU, BS, TI). The preoperative information collected included age, sex, surgical eye, preoperative diagnosis (non-clearing vitreous haemorrhage, diabetic macular oedema, traction macular and/or extramacular detachment, combined traction/rhegmatogenous detachment, progressive fibrovascular proliferation), best corrected Snellen visual acuity, and lens status. Intraoperative data recorded included surgical procedures, areas of retinal detachment, iatrogenic breaks, use of PFCL, and adjunctive procedures. All surgical procedures were monitored and recorded by a 3CCD video camera system (Ikegami, Japan).
When the surgical records were reviewed for the use of PFCL (perfluorodecalin), we identified 18 eyes of 15 patients with PDR that had received PFCL. Only patients with follow up times longer than 6 months were analysed. All eyes showed macular tractional retinal detachment with incomplete posterior vitreous detachment, and two of these eyes also had a combined traction/rhegmatogenous retinal detachment (Table 1, patients 4, and 15). We reviewed the intraoperative surgical records and videos carefully, and then analysed when PFCL was used during vitreous surgery. All patients underwent pars plana vitrectomy, membrane peeling before or after the injection of PFCL, endophotocoagulation, fluid-gas exchange, and replacement of intraocular gas with 20% sulphur hexafluoride (14 eyes), or 14% perfluoropropane (three eyes) or silicone oil (one eye). Iatrogenic breaks were treated with photocoagulation or cryopexy. Simultaneous cataract surgery was performed on 10 eyes by phacoemulsification-aspiration through the pars plana.
Table 1.
Clinical data of 18 eyes using PFCL for diabetic vitrectomy
| Visual acuity | ||||||||
| Case | Age (years) | Sex | Eye | Preoperative diagnosis | Pre | Post | Follow up (months) | Postoperative complication |
| 1 | 66 | F | LE | PVR+MTRD | 20/200 | NL | 18 | inoperable RD |
| 2 | 50 | M | LE | MTRD | HM | 20/400 | 16 | |
| 3 | 60 | F | RE | MTRD | 20/200 | 20/60 | 16 | |
| LE | VH+MTRD | LP | LP | 15 | RAO | |||
| 4 | 69 | M | LE | RRD/MTRD | HM | HM | 16 | |
| 5 | 28 | M | RE | VH+MTRD | CF | 20/20 | 16 | |
| 6 | 60 | F | RE | MTRD | LP | 20/800 | 15 | |
| 7 | 57 | M | RE | VH+MTRD | 20/400 | LP | 15 | |
| 8 | 34 | M | RE | MTRD | 20/400 | 20/200 | 14 | |
| 9 | 65 | F | RE | MTRD | HM | 20/200 | 14 | |
| LE | MTRD | HM | 20/200 | 13 | subretinal PFCL | |||
| 10 | 33 | M | RE | VH+MTRD | HM | HM | 12 | NVG |
| LE | MTRD | HM | NL | 12 | expulsive haemorrhage | |||
| 11 | 58 | M | LE | MTRD | 20/400 | 20/40 | 12 | |
| 12 | 61 | F | LE | MTRD | 20/30 | 20/40 | 11 | |
| 13 | 37 | M | RE | MTRD | CF | 20/30 | 10 | |
| 14 | 65 | M | LE | VH+MTRD | 20/100 | 20/200 | 9 | |
| 15 | 50 | F | RE | RRD/TRD | LP | CF | 6 | |
F = female; M, male; LE = left eye; RE = right eye; PVR, proliferative vitreoretinopathy; MTRD, macular tractional retinal detachment; VH = vitreous haemorrhage; RRD/TRD = combined traction/rhegnatogenous retinal detachment; HM = hand movement; CF = counting fingers; LP = light perception; RAO = retinal artery occlusion; NVG = neovascular glaucoma.
After discharge, the patients were followed in our outpatient clinic. At each follow up examination, the visual acuity, intraocular pressure, and the results of slit lamp and fundus examination were recorded. The final visual acuity and anatomical status were determined from the results of the most recent examination.
CASE REPORTS
Case 1 (patient 2)
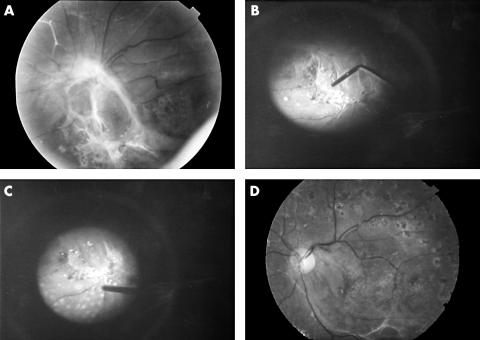
The patient was a 50 year old man who was diagnosed with PDR in both eyes. The left eye showed a longstanding tractional retinal detachment involving the macula (Fig 1A). Vitrectomy was performed and, after segmentation and delamination of the membranes, the tractional retinal detachment was flattened by a single bubble of PFCL (Fig 1B). Panretinal photocoagulation was then applied with a low energy (power 0.20 W, duration 0.2 seconds) under good visibility (Fig 1C). PFCL was then removed and replaced with 20% sulphur hexafluoride. The fundus photograph 13 months after the surgery showed reattachment of retina, and the visual acuity at this time was 20/400 (Fig 1D).
Figure 1.
Fundus photographs and intraoperative findings of patient 2 (left eye). (A) Preoperative fundus. Longstanding tractional retinal detachment is present, and the macula is severely distorted inferonasally. (B) Appearance after PFCL was injected onto the detached and distorted macula as a single bubble. (C) Macula is flattened and endophotocoagulation was applied through the PFCL. (D) Postoperative fundus. Retina is reattached but the macular distortion remained.
Case 2 (patient 3)
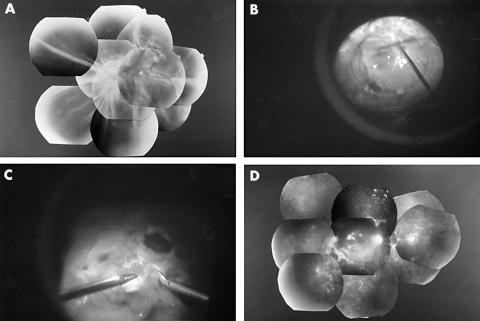
The patient was a 60 year old woman with PDR. Despite panretinal photocoagulation in all quadrants, the retinopathy progressed and dense vitreous haemorrhage appeared in both eyes. Vitrectomy was performed on both eyes. The right eye had a tractional retinal detachment involving the macula and PFCL was injected to flatten the retina. The visual acuity in the right eye recovered to 20/60 at 13 months postoperatively. For the left eye, the fundus was not visible because of a dense vitreous haemorrhage. Intraoperatively, the left eye had very strong vitreoretinal adhesions at the peripheral retina with tractional retinal detachment involving the macula. During the dissection of the proliferative membranes, multiple iatrogenic breaks developed. When the tight adhesions at the periphery were relieved, a bullous retinal detachment developed (Fig 2A). PFCL was gently injected onto the posterior retina to flatten the bullous detachment. Then, under good visibility, the peeling and shaving of the peripheral vitreous were completed (Fig 2B). The retina was reattached (Fig 2C); however the visual acuity remained at light perception as a result of a postoperative retinal artery occlusion.
Figure 2.
Fundus photographs and intraoperative findings of the left eye of patient 3. The preoperative fundus was not visible because of dense vitreous haemorrhage. After removing the vitreous haemorrhage, tractional retinal detachment involving the macula was seen. (A) After relieving the tight adhesions at the periphery, a bullous retinal detachment can be seen. Then, PFCL was injected to stabilise the detached retina. (B) Thereafter, continued peeling and shaving the peripheral vitreous was performed. (C) Postoperative fundus. Retina is reattached; however, the visual acuity remained at light perception because a retinal artery occlusion occurred 2 months postoperatively.
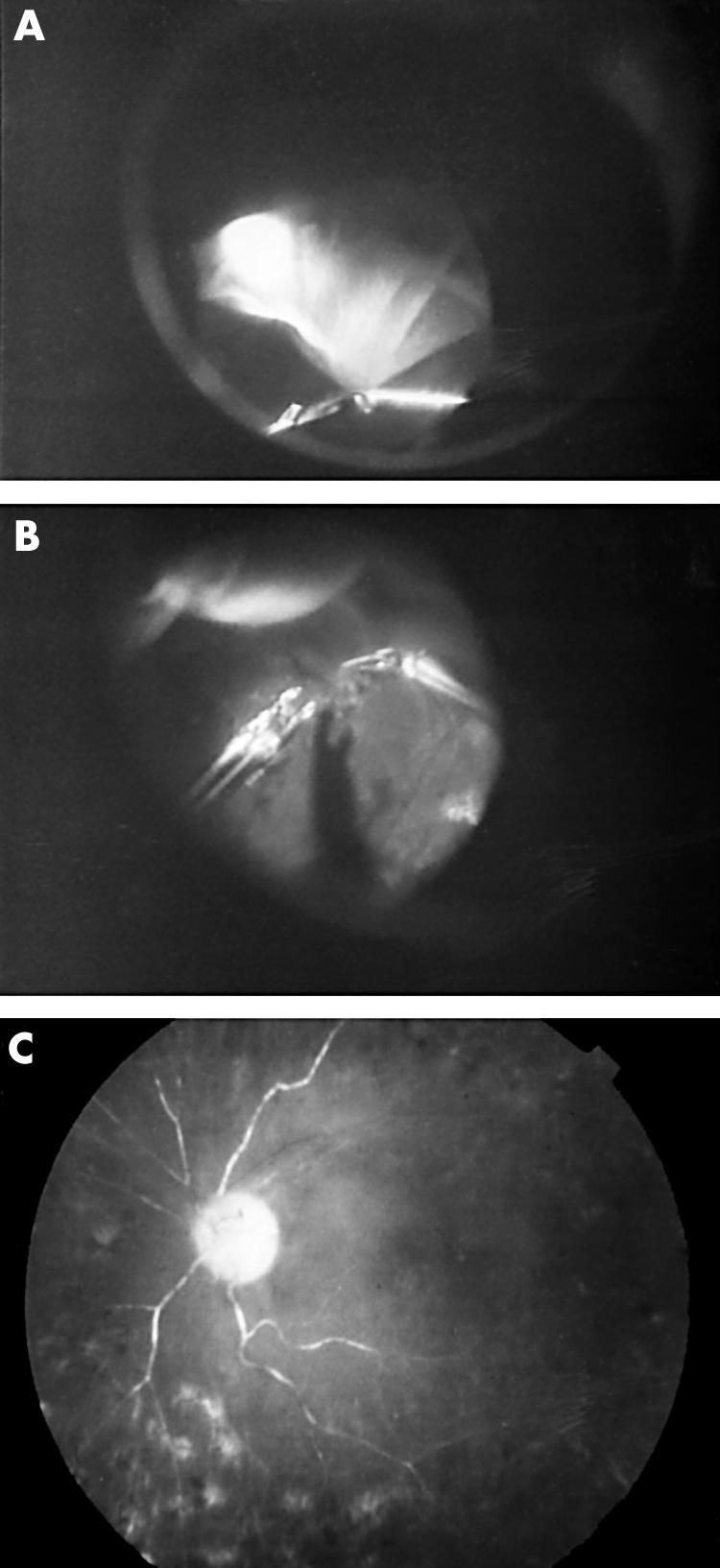
Case 3 (patient 15)
The patient was a 50 year old woman with a combined traction/rhegmatogenous retinal detachment in the right eye (Fig 3A). Proliferative membranes were recognised on the funnel-shaped retina by ophthalmoscopy. Vitrectomy was performed after lensectomy, then PFCL was injected into the centre of the funnel to flatten the detached retina (Fig 3B). The PFCL was injected gently and carefully so as none migrated beneath the retina through the large retinal break. We dissected the proliferative membranes using a bimanual technique with good visibility through the PFCL (Fig 3C). Endophotocoagulation, PFCL removal, and fluid-gas exchange were performed, and then the intraocular gas was replaced with 14% perfluoropropane.
Figure 3.
Fundus photographs and intraoperative findings of the left eye of patient 15. (A) Preoperative fundus. Combined traction/rhegmatogenous retinal detachment can be seen. (B) Intraoperative findings. PFCL was injected into the centre of the funnel to flatten the detached retina. (C) The fibrovascular membranes on the stabilised retina were dissected under good visibility. (D) Postoperative fundus. Retina is reattached with a visual acuity of finger counting.
Six months after the initial surgery, the retina was reattached with a visual acuity of finger counting (Fig 3D).
RESULTS
We studied 18 eyes of 15 patients ranging in age from 28 to 69 years (mean 52.9 years) with a follow up time of 6–18 months (mean 13.3 months). The surgical results and other clinical characteristics including preoperative diagnosis and final visual acuity are listed in Table 1. Primary vitrectomy was performed on 16 eyes and the other two eyes had had previous vitreous surgery (patients 1 and 4). Retinal reattachment was obtained in 16 of 18 eyes, and a final visual acuity of better than 20/200 was obtained in nine of the 18 eyes.
Postoperative complications included a retinal artery occlusion (patient 3, left eye) and neovascular glaucoma (patient 10, right eye). One eye had an expulsive haemorrhage during the removal of postoperative vitreous haemorrhage by fluid-gas exchange (patient 10, left eye) which resulted in a failed outcome. We were unable to reattach the retina in patient 1 who had an anterior proliferative vitreoretinopathy and retinal shortening after a previous failed vitrectomy for PDR. We also had a patient who retained a droplet of PFCL beneath the retina (patient 9, left eye). During the 13 months of follow up, the subretinal PFCL did not appear to be toxic for the retina and the patient maintained a visual acuity of 20/200.
During the PFCL injection, retinal flattening was obtained in all 18 cases. The anterior meniscus of the PFCL could be clearly observed in all cases because its index of refraction was slightly different from that of saline. Endophotocoagulation was then performed easily through the PFCL with relatively low energy under good visual observation.
In two cases (patient 3, left eye; and patient 8, right eye), a bullous retinal detachment occurred after relieving the tight vitreoretinal adhesions at the peripheral retina. PFCL was then injected to flatten the bullous detachment, and surgery was continued with shaving and dissection of the vitreous and membranes.
We also had two cases of combined traction/rhegmatogenous retinal detachment, which were successfully treated with vitrectomy in conjunction with PFCL injection. In both cases, PFCL flattened the retina before membrane peeling. We were then able to observe and remove the proliferative membranes existing on the attached retina under good visibility.
DISCUSSION
PFCL is optically clear and its index of refraction is slightly different from saline which permits good visibility for the intraoperative application of laser photocoagulation to attach the retina. In addition, PFCL has a boiling point higher than that of water and does not absorb the wavelengths used for panretinal photocoagulation. These properties allow photocoagulation through the PFCL without risk of intraocular vaporisation.13 In our cases, we applied panretinal photocoagulation through the PFCL bubble with relatively low energy as the retina was stabilised by the posterior tamponade force of the heavy liquid. This technique was especially useful when the retina was shrunk and detached by proliferative membranes. In addition, PFCL can flatten the shrunken macula intraoperatively in patients with tractional macular detachment.
Application of PFCL during vitreous surgery for PDR has been reported by several authors,14,15 and the surgical results were acceptable although the follow up time was relatively short.15 According to our surgical records, PFCL was used in the most difficult and complicated cases among our PDR patients. All 18 eyes showed macular tractional detachment, two had combined rhegmatogenous retinal detachment, and one had PVR due to a previous failed vitrectomy for PDR. The anatomical success rate was 89% (16 of 18 eyes), and a visual improvement was found in 10 eyes (55%). In previous studies, macular reattachment was achieved in 66% to 88% of eyes with tractional macular detachment, and visual acuity of 5/200 or better was attained in 59% to 71%.16–23 The Diabetic Retinopathy Vitrectomy Study reported that in eyes with severe fibrovascular proliferation and visual acuity better than 10/200, vitrectomy resulted in a final visual acuity of 20/40 or better in 44% of cases at 4 year follow up.24,25 Although the mean follow up time was 13.3 months in our cases, our surgical results including the anatomical success rate and postoperative visual acuity were comparable with the results of other investigators. The success rate was especially good considering that our 18 cases were the most complicated among the 291 consecutive eyes in our department.
The postoperative complications included neovascular glaucoma (one eye), expulsive haemorrhage (one eye), retinal artery occlusion (one eye), and subretinal migration of PFCL (one eye). The migration of PFCL into the subretinal space has been reported to occur with a frequency of 0.9%.26 At the 13 month follow up examination, this patient (patient 9) had a visual acuity of 20/200, and the droplet of PFCL appeared not to cause any visible damages to the retina. Careful injection of PFCL in a single bubble would probably prevent this complication.
A combined traction/rhegmatogenous retinal detachment in PDR is known to be difficult to manage particularly when dissecting the fibrovascular membranes on the detached retina. The use of PFCL to stabilise the detached retina was important for the successful removal of the fibrovascular membranes on the very thin retina under good visibility. In agreement with previous investigators, the postoperative visual acuity was poor in our combined cases, possibly because of severe ischaemic changes in retina.
In summary, we used PFCL during vitrectomy on 18 eyes with severe PDR and obtained satisfactory anatomical and functional results. We conclude that PFCL is a useful adjunct during vitrectomy for severe PDR, especially to flatten shrunken retinas and to perform endophotocoagulation of relatively low energy. PFCL was also useful in flattening bullous retinal detachments that appeared when relieving tight vitreoretinal adhesion, and also to stabilise a retinal detachment before membrane peeling in eyes with combined traction/rhegmatogenous retinal detachment. Longer follow up periods and additional studies with a larger number of patients will be necessary to confirm the surgical usefulness and safety of PFCL in eyes with severe PDR.
Acknowledgments
Presented in part at annual meeting of the American Academy of Ophthalmology, New Orleans, LA, USA, 2001.
The authors have no proprietary interest in any of the materials used in this study.
REFERENCES
- 1.Chang S. Low viscosity liquid fluorochemical in vitreous surgery. Am J Ophthalmol 1987;103:38–43. [DOI] [PubMed] [Google Scholar]
- 2.Chang S, Lincoff H, Zimmerman NJ, et al. Giant retinal tears: surgical techniques and results using perfluorocarbon liquid. Arch Ophthalmol 1989;107:761–6. [DOI] [PubMed] [Google Scholar]
- 3.Chang S, Ozmert E, Zimmerman NJ. Intraoperative perfluorocarbon liquid in the management of proliferative retinopathy. Am J Ophthalmol 1988;106:668–74. [DOI] [PubMed] [Google Scholar]
- 4.Chang S, Reppucci V, Zimmerman NJ. Perfluorocarbon liquid in the management of traumatic retinal detachment. Ophthalmology 1989;96:785–92. [DOI] [PubMed] [Google Scholar]
- 5.Glaser AM, Carter J, Kuppermann BD. Perfluoro-n-octane in the treatment of giant retinal tears with proliferative vitreoretinopathy. Ophthalmology 1991;98:1613–21. [DOI] [PubMed] [Google Scholar]
- 6.Lee KL, Alturki WA, Peyman GA, et al. Management of retinal detachment associated with choroidal coloboma using perfluoroperhydrophenanthrene (Vitreon). Ophthalmic Surg 1992;23:553–4. [PubMed] [Google Scholar]
- 7.Lui K, Peyman GA, Chen M, et al. Use of high-density vitreous substitutes in the removal of posteriorly dislocated lenses or intraocular lenses. Ophthalmic Surg 1991;22:503–7. [PubMed] [Google Scholar]
- 8.Shapiro MJ, Resnick KI, Kim SH, et al. Management of dislocated crystallin lens with a perfluorocarbon liquid. Am J Ophthalmol 1991;112:401–5. [DOI] [PubMed] [Google Scholar]
- 9.Rowson NJ, Bascon AS, Rosen PH. Perfluorocarbon heavy liquids in the management of posterior dislocation of the lens nucleus during phacoemulsification. Br J Ophthalmol 1992;76:169–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fanous MM, Friedman SM. Ciliary sulcus fixation of a dislocated posterior chamber intraocular lens using liquid perfluorophenanthrene. Ophthalmic Surg 1992;23:551–2. [PubMed] [Google Scholar]
- 11.Kamei M, Tano Y, Maeno T, et al. Surgical removal of submacular hemorrhage using tissue plasminogen activator and perfluorocarbon liquid. Am J Ophthalmol 1996;121:267–75. [DOI] [PubMed] [Google Scholar]
- 12.Desai UR, Peyman GA, Chen CJ, et al. Use of perfluorophenanthrene in the management of suprachoroidal hemorrhage. Ophthalmology 1992;99:1542–7. [DOI] [PubMed] [Google Scholar]
- 13.Bourke RD, Simpson RN, Cooling RJ, et al. The stability of perfluoro-n-octane during vitreoretinal procedures. Arch Ophthalmol 1996;114:537–44. [DOI] [PubMed] [Google Scholar]
- 14.Itoh R, Ikeda T, Sawa H, et al. The use of perfluorocarbon liquids in diabetic vitrectomy. Ophthalmic Surg Lasers 1999;30:672–5. [PubMed] [Google Scholar]
- 15.Maturi RK, Merrill PT, Lomeo MD, et al. Perfluoro-N-octane (PFO) in the repair of complicated retinal detachment due to severe proliferative diabetic retinopathy. Ophthalmic Surg Lasers 1999;30:715–20. [PubMed] [Google Scholar]
- 16.Rice TA, Michels RG, Rice EF. Vitrectomy for diabetic traction retinal detachment involving the macula. Am J Ophthalmol 1983;95:22–33. [DOI] [PubMed] [Google Scholar]
- 17.Han DP, Murphy ML, Mieler WF. A modified en bloc excision technique during vitrectomy for diabetic traction retinal detachment. Results and complications. Ophthalmology 1994;101:803–8. [DOI] [PubMed] [Google Scholar]
- 18.Williams DF, Williams GA, Hartz A, et al. Results of vitrectomy for diabetic traction retinal detachment using the en bloc excision technique. Ophthalmology 1989;96:752–8. [DOI] [PubMed] [Google Scholar]
- 19.Tolentino FI, Freeman HM, Tolentino FL. Closed vitrectomy in the management of diabetic traction retinal detachment. Ophthalmology 1980;87:1078–89. [DOI] [PubMed] [Google Scholar]
- 20.Aaberg TM. Pars plana vitrectomy for diabetic traction retinal detachment. Ophthalmology 1981;88:639–42. [DOI] [PubMed] [Google Scholar]
- 21.Barrie T, Feretis E, Leaver P, et al. Closed microsurgery for diabetic traction macular detachment. Br J Ophthalmol 1982;66:754–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thompson JT, de Bustros S, Michels RG, et al. Results and prognostic factors in vitrectomy for diabetic traction retinal detachment of the macula. Arch Ophthalmol 1987;105:497–502. [DOI] [PubMed] [Google Scholar]
- 23.Thompson JT, de Bustros S, Michels RG, et al. Results and prognostic factors in vitrectomy for diabetic traction-rhegmatogenous retinal detachment. Arch Ophthalmol 1987;105:503–7. [DOI] [PubMed] [Google Scholar]
- 24.Diabetic Retinopathy Vitrectomy Study Research Group. Early vitrectomy for severe proliferative diabetic retinopathy in eyes with useful vision: results of a randomized trial, Diabetic Retinopathy Vitrectomy Study Report 3. Ophthalmology 1988;95:1307–20. [DOI] [PubMed] [Google Scholar]
- 25.Diabetic Retinopathy Vitrectomy Study Research Group. Early vitrectomy for severe proliferative diabetic retinopathy in eyes with useful vision: results of a randomized trial, Diabetic Retinopathy Vitrectomy Study Report 4. Ophthalmology 1988;95:1321–34. [DOI] [PubMed] [Google Scholar]
- 26.De Queiroz JM, Blanks JC, Ozler SA, et al. Subretinal perfluorocarbon liquids: an experimental study. Retina 1992;12 (3 suppl):33–9. [PubMed] [Google Scholar]