Abstract
Aim: To investigate the relation between the clinical and electrophysiological abnormalities of patients undergoing visual evoked potential investigation for albinism.
Methods: 40 subjects with a probable or possible clinical diagnosis of albinism underwent pattern appearance and/or flash visual evoked potential (VEP) examination. The VEP findings are correlated with the clinical features of albinism determined by clinical examination and orthoptic assessment.
Results: The majority of patients with clinical evidence of albinism showed a contralateral predominance in the VEPs. There was close correlation between the clinical signs of albinism and the degree of contralateral VEP predominance. This manifested as an interhemispheric latency asymmetry to monocular pattern appearance stimulation but amplitude asymmetry to flash stimulation. The strongest correlation for pattern appearance interhemispheric latency difference was with foveal hypoplasia (rho = 0.58; p = 0.0003) followed by nystagmus (rho = 0.48; p = 0.0027) and iris transillumination (rho = 0.33; p = 0.039). The VEP abnormalities were of greater magnitude in those patients with most features of albinism. Several patients with apparently mild disorders of ocular pigmentation had small but significantly abnormal VEP latency asymmetries.
Conclusion: There is a strong association between the magnitude of the interhemispheric latency asymmetry of the pattern appearance VEP, and of amplitude asymmetry of the flash VEP, with the clinical signs of albinism. The data are consistent with a spectrum of abnormalities in albinism involving both clinical expression and electrophysiological misrouting, which is wider than previously recognised.
Keywords: albinism, visual evoked potentials, visual development, nystagmus, binocular vision
Albinism is a heterogeneous, genetically determined disorder of melanin synthesis in which either the eyes (ocular albinism), or the eyes, skin, and hair may be affected (oculocutaneous albinism).1–4 The different mutations are thought to act through a common pathway involving reduced melanin synthesis in the eye during development to produce the ocular abnormalities found.3,4 Ocular signs include foveal hypoplasia, fundal hypopigmentation, iris transillumination, nystagmus, reduced visual acuity, reduced or absent stereopsis, squint, and refractive errors. In addition, there is a characteristic anomaly of chiasmal decussation such that the majority of fibres from each eye cross to the contralateral hemisphere.5 This can be demonstrated by visual evoked potential (VEP) examination where albino patients have a contralateral predominance in the responses to monocular stimulation.6–20 If the clinical diagnosis is in doubt, VEP examination is the diagnostic investigation of choice and may provide conclusive evidence. Previous studies have examined the sensitivity and specificity of electrophysiological testing in albino subjects.11,12,17,21,22 Studies of pattern appearance VEPs have concentrated on the asymmetry of the amplitude of the VEP.9,11,12,15,18–20 However, our experience suggested that the abnormalities of the response to pattern appearance stimulation also involve latency.
The clinical diagnosis of albinism is not difficult when most of the clinical signs are present. However, there is considerable variability in the clinical signs present in individual patients; indeed, significant VEP abnormalities have been described in children having only iris transillumination and mildly reduced visual acuity.23 The present study examines the data from a series of patients referred for electrophysiological investigation of possible albinism, rather than a group with established diagnoses. The first aim of the study has been to determine the clinical features of albinism which correlate most closely with electrophysiological abnormalities and which particular electrophysiological parameters best correlate with the clinical features. The second aim has been to determine the nature and magnitude of the VEP abnormalities, if any, which are present in patients with only mild pigmentary abnormalities, who would not normally have been diagnosed as albino on clinical grounds.
Preliminary accounts of some of these findings have been presented.24,25
PATIENTS AND METHODS
Pattern appearance VEPs were recorded from 40 subjects with a probable or possible clinical diagnosis of albinism or a strong family history. Clinical signs of albinism were recorded after full orthoptic examination, biomicroscopy, and fundal examination. A scoring system was used in which a score of one each was given for the presence of foveal hypoplasia, iris transillumination, fundal hypopigmentation or nystagmus (a possible total score of 4). Thus, a patient with an albino score of 4 has more features of albinism than one with a lower score. The majority of the patients were examined by one of the authors (SD); in some patients the clinical data were ascertained from the case notes.
Pattern appearance VEPs were recorded using black and white checkerboard stimulation with 98% contrast and a mean luminance level of 80 cd/m2. The stimulus was presented for 152 ms at a frequency of 1.2 Hz. At the viewing distance of 1.0 metre, the field size was 20° by 16°, with a check size of 1.1°. Five electrodes were positioned 3–5 cm apart (depending on the subject’s head size) across the occiput in a row 2 cm above the inion. These were referred to a mid-frontal reference electrode at Fz. Electrode impedance was <5 kohms. Low and high bandpass filter settings were 1 Hz and 100 Hz with an analysis time of 250 ms. Patients wore their full spectacle correction throughout.
The latency and amplitude of the major positive peak were measured. The interhemispheric latency asymmetry was calculated by subtraction of the longer latency measured for each hemisphere such that right eye response difference was the longest right hemisphere latency minus the longest left hemisphere latency and vice versa. A positive score thus represents a relative delay in the response over the ipsilateral hemisphere. Clinical features for each patient were correlated both with the greater monocular latency asymmetry and also the mean of the latency asymmetry for the two eyes. The latencies measured at the two electrode positions over each hemisphere did not systematically differ, and an alternative analysis using the mean of the two latency values for each hemisphere gave comparable results. The asymmetry of the amplitude of the response was calculated for stimulation of each eye by dividing the mean of the amplitudes recorded at the two ipsilateral electrodes by the mean at the two contralateral electrodes. The clinical features for each patient were correlated with amplitude in a similar manner to that used for latency, with both the greater monocular amplitude ratio asymmetry and a mean value for the two eyes being assessed.
Flash VEPs were recorded using the same electrode array. Flash VEPs were recorded to a 2 Hz stimulus of intensity 17 cd/s/m2 using a Grass photic stimulator positioned approximately 25 cm from the subject’s eyes (<25 cm if younger subjects showed limited compliance). All evoked potentials in the patient group were assessed in relation to an extensive normal control series recorded as part of the study using the same protocol.
In addition to conventional measures of latency and amplitude, the pattern appearance VEP asymmetry was further assessed using an amplitude asymmetry index (AAI) as previously suggested by Apkarian.18 This measure is derived from the amplitudes determined at a single latency for each eye over each hemisphere based on the latency of the maximum amplitude of the major positive response in the contralateral hemisphere for the particular patient. Apkarian found a significant asymmetry index to be greater than 0.7.18
The correlations between the clinical and electrophysiological features were calculated using the Spearman rank correlation with correction for tied values.
The study followed the tenets of the Declaration of Helsinki and was approved by the ethics committee of Moorfields Eye Hospital.
RESULTS
The pattern appearance and flash VEP parameters for normal control subjects are summarised in Table 1. In particular, note that no normal subject showed a monocular pattern appearance VEP latency difference between hemispheres of more than 3 ms. A flash VEP was considered abnormal if there was an interhemispheric latency asymmetry of greater than 6 ms or an amplitude asymmetry greater than 50% (ipsilateral amplitude less than half of the contralateral amplitude).
Table 1.
Pattern appearance and flash VEP parameters for normal control subjects
| Latency difference (ms) Mean (2 SD) (range) | Amplitude ratio Mean (2 SD) (range) | ||||||
| Stimulus | Number of subjects | Right eye | Left eye | Mean | Right eye | Left eye | Mean |
| Pattern appearance | 27 | −0.04 (1.86) (−2 to +3) | 0.07 (2.05) (−2 to +2.5) | 0.02 (1.86) (−0.5 to +2) | 1.10 (0.50) (0.71 to 1.77) | 1.01 (0.42) (0.63 to 1.59) | 1.06 (0.23) (0.91 to 1.37) |
| Flash | 11 | −0.09 (2.44) (−2.0 to +2.0) | −0.73 (2.54) (−4.0 to 0) | −0.41 (1.47) (−1.5 to +1.0) | 1.1 (0.52) (0.73 to 1.30) | 1.1 (0.59) (0.81 to 1.63) | 1.1 (0.15) (0.96 to 1.19) |
The 26 male and 14 female albino subjects studied had a mean age of 10.6 years (range 2–38 years). The clinical and electrophysiological data for all 40 patients are shown in Table 2. Seventeen of the patients with squint had a manifest esotropia; five had an exotropia. A number of the patients had intermittent squints, with a degree of stereopsis when their eyes were aligned.
Table 2.
Clinical and electrophysiological data for all patients
| Case number | Age (years) | Snellen acuity right eye | Snellen acuity left eye | Stereoacuity (sec of arc) | Foveal hypoplasia | Fundal hypopigmentation | Iris transillumination | Nystagmus | Manifest squint | Cutaneous albinism | Abnormal flash VEP | Right eye latency difference (ms) | Left eye latency difference (ms) | Mean latency difference (ms) | Amplitude asymmetry index |
| 1 | 6 | 6/6 | 6/6 | 120 | − | − | − | − | No | No | No | 0 | 1 | 1 | 0.0 |
| 2 | 5 | 6/24 | 6/6 | 120 | − | − | − | − | No | No | – | 4 | 2 | 3 | 0.1 |
| 3 | 8 | 6/5 | 6/5 | – | − | + | − | − | No | No | No | −7 | −2 | −4 | 0.2 |
| 4 | 5 | 6/6 | 6/6 | 110 | − | + | − | − | No | No | No | 13 | −13 | 0 | 0.4 |
| 5 | 5 | 6/9 | 6/9 | 210 | − | − | − | + | No | No | No | 14 | −2 | 6 | 0.0 |
| 6 | 9 | 6/6 | 6/9 | 6000 | − | − | − | + | Yes | No | No | 43 | 9 | 26 | 0.8 |
| 7 | 11 | 6/36 | 6/18 | Nil | − | − | − | + | No | No | No | 45 | 36 | 41 | 0.5 |
| 8 | 22 | 6/18 | 1/36 | – | − | + | + | − | – | No | No | 0 | −3 | −2 | 0.4 |
| 9 | 6 | 6/12 | 6/12 | 110 | − | + | + | + | No | No | No | 6 | −7 | −1 | −0.2 |
| 10 | 4 | 6/18 | 6/12 | 550 | − | + | + | + | No | No | Yes | −9 | 14 | 2 | 1.0 |
| 11 | 9 | 6/36 | 6/36 | 6000 | + | − | − | + | Yes | Yes | Yes | 60 | 59 | 59 | 1.5 |
| 12 | 15 | 6/6 | 6/6 | Nil | + | + | − | − | Yes | Yes | Yes | 6 | 7 | 7 | 0.5 |
| 13 | 4 | 6/24 | 6/24 | Nil | + | + | + | − | Yes | No | No | 18 | −7 | 6 | 0.6 |
| 14 | 6 | 6/12 | 6/9 | 6000 | + | + | + | − | Yes | Yes | No | −6 | 7 | 1 | 0.4 |
| 15 | 4 | 6/12 | 6/12 | 120 | + | + | + | − | No | No | No | 3 | 16 | 10 | 0.2 |
| 16 | 8 | 6/9 | 6/9 | 110 | + | + | + | − | No | No | No | 36 | 25 | 30 | 1.5 |
| 17 | 7 | 6/18 | 6/12 | 240 | + | + | + | − | Yes | Yes | No | 14 | 29 | 22 | 1.1 |
| 18 | 12 | 6/12 | 6/12 | 6000 | + | + | + | − | Yes | No | Yes | 35 | 46 | 41 | 1.0 |
| 19 | 14 | 6/12 | 6/18 | 6000 | + | + | + | − | Yes | No | Yes | 60 | 57 | 58 | 1.1 |
| 20 | 6 | 6/36 | 6/36 | Nil | + | + | − | + | Yes | Yes | Yes | 46 | 18 | 32 | 0.9 |
| 21 | 10 | 6/24 | 6/18 | 6000 | + | + | − | + | No | No | No | 9 | 8 | 8 | 1.1 |
| 22 | 10 | 6/9 | 6/12 | Nil | + | + | + | + | No | Yes | No | 13 | 22 | 17 | 0.5 |
| 23 | 6 | 6/24 | 6/24 | Nil | + | + | + | + | Yes | No | Yes | 19 | 49 | 34 | 0.6 |
| 24 | 13 | 6/24 | 6/24 | Nil | + | + | + | + | Yes | No | Yes | 35 | 31 | 33 | 1.1 |
| 25 | 18 | 3/60 | 3/60 | Nil | + | + | + | + | – | Yes | No | 61 | 60 | 60 | 1.6 |
| 26 | 7 | 6/12 | 6/12 | 6000 | + | + | + | + | Yes | No | Yes | 37 | 28 | 33 | 1.3 |
| 27 | 10 | 6/12 | 6/12 | Nil | + | + | + | + | Yes | Yes | Yes | 39 | 5 | 22 | 1.7 |
| 28 | 17 | 2/60 | 4/60 | Nil | + | + | + | + | No | No | Yes | 52 | 54 | 53 | 1.6 |
| 29 | 30 | 6/36 | 6/36 | 6000 | + | + | + | + | No | No | No | 54 | 50 | 52 | 1.3 |
| 30 | 4 | 6/60 | 6/60 | Nil | + | + | + | + | Yes | Yes | No | 57 | 2 | 29 | 1.0 |
| 31 | 4 | 6/12 | 6/18 | 6000 | + | + | + | + | Yes | Yes | Yes | 33 | 43 | 38 | 1.6 |
| 32 | 7 | 6/9 | 6/12 | 6000 | + | + | + | + | Yes | No | No | 33 | 56 | 44 | 1.0 |
| 33 | 16 | 6/18 | 6/18 | – | + | + | + | + | No | No | No | 63 | 59 | 61 | 1.2 |
| 34 | 2 | 6/60 | 6/60 | Nil | + | + | + | + | Yes | No | Yes | 47 | −19 | 14 | 0.9 |
| 35 | 11 | 6/36 | 6/24 | 6000 | + | + | + | + | Yes | Yes | Yes | 24 | 14 | 19 | 1.7 |
| 36 | 13 | 6/36 | 6/36 | Nil | + | + | + | + | Yes | No | Yes | 37 | 42 | 40 | 1.7 |
| 37 | 38 | 6/36 | 6/36 | Nil | + | + | + | + | Yes | Yes | No | 63 | 64 | 63 | 0.9 |
| 38 | 5 | 6/12 | 6/12 | Nil | + | + | + | + | Yes | No | Yes | 39 | 27 | 33 | 1.0 |
| 39 | 19 | 6/36 | 6/36 | – | + | + | + | + | No | No | No | 73 | 84 | 78 | 1.1 |
| 40 | 4 | 6/18 | 6/36 | Nil | + | + | + | + | Yes | No | Yes | 66 | 45 | 55 | 1.0 |
Fourteen patients had cutaneous signs of albinism to clinical examination (Table 2). There were no significant differences in either pattern appearance interhemispheric latency difference or AAI between those with and without cutaneous signs for the whole group (unpaired t test; latency difference, p = 0.56; AAI, p = 0.08) or for subjects with albino scores of 3 or 4 (latency difference, p = 0.28; AAI, p = 0.65). This confirms previous observations7,26; all patients have thus been analysed as a single group.
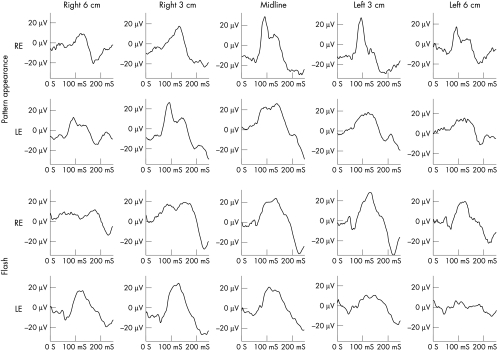
The typical pattern appearance and flash VEP abnormalities, demonstrating the intracranial misrouting, are illustrated in Figure 1 (case 26). The monocular responses from each eye show markedly abnormal distribution with contralateral predominance shown by increased latency and/or reduced amplitude of the response in the ipsilateral hemisphere. Note in the pattern appearance response that the latency of the major component in the ipsilateral hemisphere is considerably longer than that in the contralateral hemisphere.
Figure 1.
Five channel pattern appearance and flash VEPs from case 26 showing the contralateral predominance typical of albinism. All electrodes are referred to Fz. Note the markedly shorter latency of the prominent positive component in the contralateral hemisphere traces of the pattern appearance VEP and the greatly reduced amplitude of the ipsilateral response in the first 150 ms of the flash VEPs.
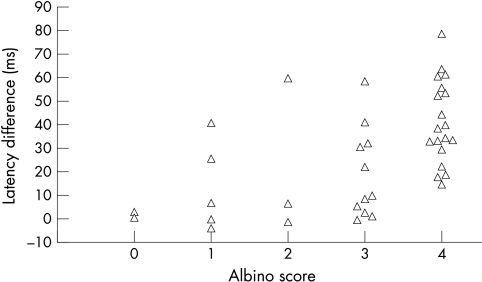
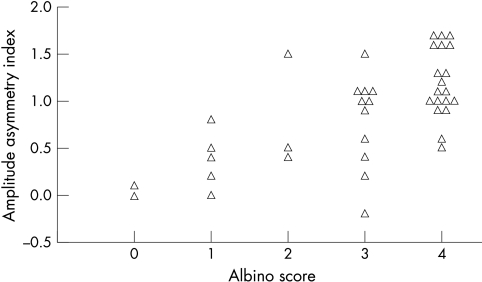
The relation between the mean interhemispheric VEP latency difference and the clinical albino scores is shown for all subjects in Figure 2. There is a significant increase in the magnitude of the interhemispheric difference with increasing albino score (linear regression; r2 = 0.27, p <0.001). The AAI shows a similar increase (Fig 3; linear regression; r2 = 0.42, p <0.001). The statistical correlations between parameters of the pattern appearance VEP and the individual clinical features of albinism are shown in Table 3. The strongest association with pattern appearance latency difference, and also for AAI, is with foveal hypoplasia, followed by nystagmus and iris transillumination. The latency difference also correlates strongly with reduced visual acuity and reduced stereopsis. The peak amplitude ratio showed no significant correlation with the overall albino score or with any of the individual clinical features.
Figure 2.
Graph showing the relation of the mean interhemispheric latency difference to the albino score.
Figure 3.
Graph showing the relation of the amplitude asymmetry index to the albino score.
Table 3.
Correlation of clinical features of albinism with pattern appearance VEP parameters
| Mean latency difference | Greatest monocular latency difference | Amplitude asymmetry index | Greatest monocular peak amplitude ratio | |||||
| rho | p | rho | p | rho | p | rho | p | |
| Albino score | 0.58 | 0.0003 | 0.61 | 0.0002 | 0.63 | <0.0001 | −0.06 | 0.7288 |
| Foveal hypoplasia | 0.58 | 0.0003 | 0.56 | 0.0005 | 0.63 | <0.0001 | −0.07 | 0.6846 |
| Iris transillumination | 0.33 | 0.0393 | 0.35 | 0.0270 | 0.43 | 0.0075 | 0.10 | 0.5246 |
| Nystagmus | 0.48 | 0.0027 | 0.53 | 0.0009 | 0.43 | 0.0080 | −0.03 | 0.8398 |
| Fundal hypopigmentation | 0.09 | 0.5570 | 0.13 | 0.4154 | 0.33 | 0.0383 | 0.12 | 0.4373 |
| Left Snellen acuity | −0.58 | 0.0003 | −0.67 | <0.0001 | −0.49 | 0.0021 | 0.20 | 0.2026 |
| Right Snellen acuity | −0.47 | 0.0037 | −0.52 | 0.0012 | −0.43 | 0.0075 | 0.21 | 0.1876 |
| Stereopsis | 0.47 | 0.0055 | 0.52 | 0.0020 | 0.27 | 0.1120 | 0.04 | 0.8271 |
There were significant correlations between the amplitude asymmetry of the flash VEP and both foveal hypoplasia and overall albino score when the whole group of patients was analysed, but little correlation with latency (Table 4). (Note that greater amplitude asymmetry gives a smaller amplitude ratio and so a negative value for rho). However, when the flash VEP analysis was restricted to patients aged 7 years or less there were strong correlations between the amplitude asymmetry of the flash response and all the clinical parameters (Table 5). There were no significant correlations between the interhemispheric flash VEP latency difference and clinical measures in this young group (Table 5).
Table 4.
Correlation of clinical features of albinism with flash VEP parameters for all ages
| Latency difference | Amplitude ratio | |||
| rho | p | rho | p | |
| Albino score | 0.01 | 0.9335 | −0.41 | 0.0118 |
| Foveal hypoplasia | −0.12 | 0.4430 | −0.54 | 0.0010 |
| Iris transillumination | 0.09 | 0.5954 | −0.30 | 0.0667 |
| Nystagmus | −0.07 | 0.6589 | −0.23 | 0.1483 |
| Fundal hypopigmentation | 0.06 | 0.7052 | −0.23 | 0.1656 |
| Left Snellen acuity | 0.27 | 0.0963 | 0.25 | 0.1192 |
| Right Snellen acuity | 0.34 | 0.0372 | 0.19 | 0.2307 |
| Stereopsis | −0.14 | 0.4096 | −0.32 | 0.0659 |
Table 5.
Correlation of clinical features of albinism with flash VEP parameters for patients aged 7 years or under
| Latency difference | Amplitude ratio | |||
| rho | p | rho | p | |
| Albino score | 0.05 | 0.8519 | −0.72 | 0.0030 |
| Foveal hypoplasia | 0.10 | 0.6929 | −0.54 | 0.0266 |
| Iris transillumination | 0.03 | 0.9153 | −0.54 | 0.0257 |
| Nystagmus | 0.03 | 0.8881 | −0.48 | 0.0491 |
| Fundal hypopigmentation | 0.10 | 0.6729 | −0.55 | 0.0246 |
| Left Snellen acuity | 0.09 | 0.7166 | 0.57 | 0.0183 |
| Right Snellen acuity | 0.16 | 0.5174 | 0.48 | 0.0491 |
| Stereopsis | 0.02 | 0.9401 | −0.50 | 0.0385 |
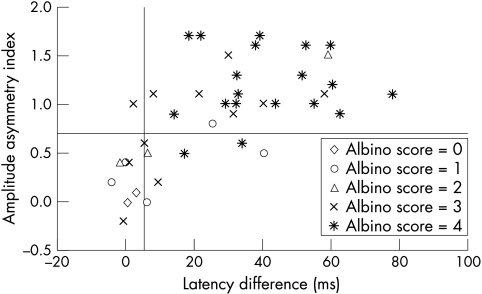
The relation between the pattern appearance latency difference and the AAI for each patient is plotted in Figure 4. There is a strong correlation between the two electrophysiological measures (r = 0.64; p <0.0001); most patients with albino scores of 3 or 4 were abnormal on both measures. However, three patients had an abnormal interhemispheric latency difference, but an AAI within normal limits. Two of these had albino scores of 4 (cases 22 and 23), with one (case 22) showing cutaneous features of albinism. They were aged 10 and 6. The third patient not correctly identified as albino by the AAI method was aged 4, had an albino score of 3, and showed a clear latency difference on stimulation only of one eye (case 15).
Figure 4.
Graph showing the relation of the mean interhemispheric latency difference to the amplitude asymmetry index for all patients segregated by albino score.
Table 2 presents the patients in approximately increasing order of strength of evidence for a diagnosis of albinism. Cases 1–4 showed no clinical evidence of albinism, apart from fundal pallor in one, and had normal electrophysiology with the exception of case 4 who showed a similar latency difference in one hemisphere to stimulation of either eye, not indicative of albino misrouting. Cases 16–40 were albino by both clinical and electrophysiological criteria. Cases 5–15 showed variable evidence of albinism by clinical criteria, although most had reduced visual acuity and stereoacuity and so were not simply albinoid.27 Two cases in this intermediate group had marked bilateral latency differences (cases 7 and 11) and a third case had marked latency difference from one eye and a small difference from the other eye (case 6). The electrophysiological abnormality in a further six of these patients was either a small, but clearly abnormal, bilateral latency difference (case 12) or an abnormal interhemispheric latency asymmetry to stimulation of one eye only (cases 5, 10, 13, 14, and 15). Of these six, cases 10 and 12 had abnormal flash VEPs in keeping with albino misrouting; case 12 had foveal hypoplasia with pale skin, hair and fundus, bilateral visual acuities of 6/6, and a small esotropia; case 14 had marked iris transillumination, foveal hypoplasia and fair hair, with visual acuities of 6/12 in the right eye, and 6/9 in the left, a small near esotropia, and gross stereopsis. There were three patients in this intermediate group with an abnormal AAI (cases 6, 10, and 11).
Case 13, who had foveal hypoplasia, iris transillumination, and a pale fundus, had a “negative” ERG on full field ERG testing consistent with a diagnosis of Åland Island disease, in which congenital stationary night blindness occurs in addition to pigmentary abnormalities similar to those seen in albinism28 and in which crossed asymmetry of the flash VEP has been described.29
DISCUSSION
Some of the cohort of patients described had been referred for electrophysiological testing because of a clinical suspicion or a family history of albinism; others were clinically thought to have albinism and were referred for confirmatory electrophysiology. Thus, although not strictly a population study, these patients form a representative clinical cross section of patients with disorders of ocular pigmentation ranging from the very mild to typically albino. The data show a close correlation between the presence and magnitude of a pattern appearance VEP latency difference between hemispheres and the clinical features of albinism. Foveal hypoplasia gave the highest correlation of the individual clinical features, and there were strong correlations with iris transillumination, nystagmus, reduced visual acuity, and reduced stereoacuity. The findings further confirm the value of VEP latency measurements in the diagnosis of albinism; latency measurement was more sensitive than an amplitude asymmetry index (AAI), which would have failed to identify three patients as albino.
It is well recognised that the sensitivity of the flash VEP to detect albinism declines with age19,30; this was manifest in weak correlations between flash VEP parameters and clinical features when patient age was not taken into account. However, when patients aged 7 or less were analysed separately, there were strong correlations between all the clinical features and interhemispheric flash amplitude asymmetry but, in contrast with the findings with pattern appearance stimulation, no correlations with interhemispheric latency difference.
In most patients with strong clinical evidence of albinism the electrophysiology serves to confirm the clinical diagnosis. However, it is of particular value to the clinician for patients in whom the clinical signs are less definite. For example, the abnormal intracranial misrouting of albinism was established by evoked potential examination in seven patients who lacked typical features of albinism, three having no iris transillumination and four lacking nystagmus.
The patients in this study showed a gradation of clinical abnormality, which correlated with the magnitude of the VEP asymmetry, demonstrating a relation between the severity of the pigmentary abnormality and the degree of chiasmal misrouting in human albinos. This establishes the misrouting in human albinism to be a spectrum of abnormality rather than an “all or none” change. A similar relation has been demonstrated by anatomical methods in animal studies.31,32 Most patients with clinically obvious albinism had large latency differences, but a number of patients had a mild ocular pigmentary disorder with reduced visual acuity and stereoacuity and smaller latency abnormalities. However, these were still well outside the normal range of interhemispheric latency difference. These patients resemble a group of 18 children studied by Sjödell et al,23 who were selected on the basis of reduced visual acuity and iris transillumination. Eight of those were found to have typical albino VEP asymmetries to flash stimulation while a further four were described as having small, atypical asymmetries.
Three patients had nystagmus alone, with no evidence of hypopigmentation (cases 5, 6, and 7). One had VEPs typical of albinism with a pronounced latency difference on stimulation of either eye; one had a large latency difference to stimulation of one eye and a small difference to stimulation of the other; the third showed a small but significant latency difference from one eye only. Similar patients have been previously described by some authors,33 but other electrophysiological studies of patients with nystagmus, but no associated pigmentary abnormality, do not describe similar abnormalities.18,34 Some patients with apparent congenital nystagmus may have subclinical albinism35 and our observations are thus of particular clinical relevance.
Five of the six patients with a marked interocular difference in latency asymmetry were children between 2 and 6 years of age (cases 5, 10, 15, 30, and 34). The pattern appearance response may fail to be diagnostic in young children with albinism and this may reflect immaturity of the central visual pathways. These five young children were all thought clinically to be albino and longitudinal study will be of interest.
To conclude, the ocular pigmentary changes seen in this study present a spectrum of abnormality and this is paralleled by, and correlated with, a variable degree of electrophysiological abnormality. In addition to patients with clinically obvious albinism, there are a considerable number of patients with mild pigmentary abnormalities who show VEP evidence of intracranial misrouting. The identification of such patients is important as they may be at risk of having more seriously affected children.
Acknowledgments
We are grateful to Miss GW Adams, Mr AT Moore, and Mr J Lee for permission to report data from patients under their care and to Ms C Bunce for statistical advice.
Proprietary interests: None.
Grant support: Special Trustees, Moorfields Eye Hospital.
REFERENCES
- 1.Carden SM, Boissy RE, Schoettker PJ, et al. Albinism: modern molecular diagnosis. Br J Ophthalmol 1998;82:189–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Biswas S, Lloyd IC. Oculocutaneous albinism. Arch Dis Child 1999;80:565–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oetting WS. Albinism. Curr Opin Pediatr 1999;11:565–71. [DOI] [PubMed] [Google Scholar]
- 4.Oetting WS, King RA. Molecular basis of albinism: mutations and polymorphisms of pigmentation genes associated with albinism. Hum Mutat 1999;13:99–115. [DOI] [PubMed] [Google Scholar]
- 5.Guillery RW. Why do albinos and other hypopigmented mutants lack normal binocular vision, and what else is abnormal in their central visual pathways? Eye 1996;10:217–21. [DOI] [PubMed] [Google Scholar]
- 6.Creel D, Witkop Jr CJ, King RA. Asymmetric visually evoked potentials in human albinos: evidence for visual system anomalies. Invest Ophthalmol 1974;13:430–40. [PubMed] [Google Scholar]
- 7.Creel D, O’Donnell Jr FE, Witkop Jr CJ. Visual system anomalies in human ocular albinos. Science 1978;201:931–3. [DOI] [PubMed] [Google Scholar]
- 8.Coleman J, Sydnor C, Wolbarsht M, et al. Abnormal visual pathways in human albinos studied with visual evoked potentials. Exp Neurol 1979;65:667–79. [DOI] [PubMed] [Google Scholar]
- 9.Creel D. Luminance-onset, pattern-onset and pattern-reversal evoked potentials in human albinos demonstrating visual system anomalies. J Biomed Eng 1979;1:100–4. [DOI] [PubMed] [Google Scholar]
- 10.Carroll WM, Jay BS, McDonald WI, et al. Pattern evoked potentials in human albinism. J Neurol Sci 1980;48:265–86. [DOI] [PubMed] [Google Scholar]
- 11.Creel D, Spekreijse H, Reits D. Evoked potentials in albinos: efficacy of pattern stimuli in detecting misrouted optic fibers. Electroenceph Clin Neurophysiol 1981;52:595–603. [DOI] [PubMed] [Google Scholar]
- 12.Apkarian P, Reits D, Spekreijse H, et al. A decisive electrophysiological test for human albinism. Electroenceph Clin Neurophysiol 1983;55:513–31. [DOI] [PubMed] [Google Scholar]
- 13.Boylan C and Harding GF. Investigation of visual pathway abnormalities in human albinos. Ophthalmic Physiol Opt 1983;3:273–85. [PubMed] [Google Scholar]
- 14.van Dorp DB, van Haeringen NJ, Delleman JW, et al. Albinism: phenotype or genotype? Doc Ophthalmol 1983;56:183–94. [DOI] [PubMed] [Google Scholar]
- 15.Apkarian P, Reits D, Spekreijse H. Component specificity in albino VEP asymmetry: maturation of the visual pathway anomaly. Exp Brain Res 1984;53:285–94. [DOI] [PubMed] [Google Scholar]
- 16.Boylan C, Clement RA, Harding GF. Lateralization of the flash visual-evoked cortical potential in human albinos. Invest Ophthalmol Vis Sci 1984;25:1448–50. [PubMed] [Google Scholar]
- 17.Russell-Eggitt I, Kriss A, Taylor D. Albinism in childhood. Br J Ophthalmol 1990;74:136–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Apkarian P, Shallo-Hoffmann J. VEP projections in congenital nystagmus; VEP asymmetry in albinism: a comparison study. Invest Ophthalmol Vis Sci 1991;32:2653–61. [PubMed] [Google Scholar]
- 19.Kriss A, Russell-Eggitt I, Harris CM, et al. Aspects of albinism. Ophthal Paediatr Genet 1992;13:89–100. [DOI] [PubMed] [Google Scholar]
- 20.Bouzas EA, Caruso RC, Drews-Bankiewicz MA, et al. Evoked potential analysis of visual pathways in human albinism. Ophthalmology 1994;101:309–14. [DOI] [PubMed] [Google Scholar]
- 21.Kriss A, Russell-Eggitt I, Taylor D. Childhood albinism. Visual electrophysiological features. Ophthal Paediatr Genet 1990;11:185–92. [DOI] [PubMed] [Google Scholar]
- 22.Soong F, Levin A, Westall C. Comparison of techniques for detecting visual evoked potential asymmetry in albinism. J AAPOS 2000;4:302–10. [DOI] [PubMed] [Google Scholar]
- 23.Sjodell L, Sjostrom A and Abrahamsson M. Transillumination of iris and subnormal visual acuity–ocular albinism? Br J Ophthalmol 1996;80:617–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dorey S, Neveu M, Burton L, et al. The clinical features of albinism and their correlation with visual evoked potentials (ARVO abstract). Invest Ophthalmol Vis Sci 1999;40:821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dorey S, Neveu M, Burton L, et al. The correlation between visual evoked potential abnormalities and the clinical features of albinism. In: Proceedings of the 25th Meeting of the European Strabismological Association. Lisse: Aoleus Press, 1999:171–5.
- 26.Creel DJ, Summers CG, King RA. Visual anomalies associated with albinism. Ophthal Paediatr Genet 1990;11:193–200. [DOI] [PubMed] [Google Scholar]
- 27.Kinnear PE, Jay B, Witkop Jr CJ. Albinism. Surv Ophthalmol 1985;30:75–101. [DOI] [PubMed] [Google Scholar]
- 28.Weleber RG, Pillers DA, Powell BR, et al. Aland Island eye disease (Forsius-Eriksson syndrome) associated with contiguous deletion syndrome at Xp21. Similarity to incomplete congenital stationary night blindness. Arch Ophthalmol 1989;107:1170–9. [DOI] [PubMed] [Google Scholar]
- 29.Tremblay F, De Becker I, Cheung C, et al. Visual evoked potentials with crossed asymmetry in incomplete congenital stationary night blindness. Invest Ophthalmol Vis Sci 1996;37:1783–92. [PubMed] [Google Scholar]
- 30.Apkarian P. Methodology of testing for albinism with visual evoked cortical potentials. In: Heckenlively JR, Arden GB, Eds. Principles and practice of clinical electrophysiology of vision. St Louis: Mosby Year Book, 1991:425–34.
- 31.Sanderson K, Guillery R, Shackleford R. Congenitally abnormal visual pathways in mink (Mustela vision) with reduced retinal pigment. J Comp Neurol 1974;154:225–48. [DOI] [PubMed] [Google Scholar]
- 32.La Vail J, Nixon R, Sidman R. Genetic control of retinal ganglion cell projections. J Comp Neurol 1978;182:399–422. [DOI] [PubMed] [Google Scholar]
- 33.Meienberg O, Hemphill G, Rosenberg M, et al. Visually evoked response asymmetries in a family with congenital nystagmus:possible evidence of abnormal visual projections. Arch Neurol 1980;37:697–8. [DOI] [PubMed] [Google Scholar]
- 34.Guo SQ, Reinecke RD, Fendick M, et al. Visual pathway abnormalities in albinism and infantile nystagmus: VECPs and stereoacuity measurements. J Pediatr Ophthalmol Strabismus 1989;26:97–104. [DOI] [PubMed] [Google Scholar]
- 35.Simon J, Kandel G, Krohel G, et al. Albinotic characteristics in congenital nystagmus. Am J Ophthalmol 1984;97:320–7 [DOI] [PubMed] [Google Scholar]