Abstract
Aims: Patients with central serous chorioretinopathy were tested for psychosomatic symptoms and social support at the onset of their ailments; their personality profiles were also tested.
Methods: 24 consecutive outpatients at the department of ophthalmology, Freiburg University Hospital, Freiburg, Germany, presenting with central serous chorioretinopathy filled in the following standardised questionnaires: Symptom Checklist 90-R (SCL 90-R), Symptom List, Questionnaire on Social Support, and Sixteen Personality Factor Questionnaire.
Results: The sample (n=24) included 22 male patients with an average age of 44.1 years. Three quarters of the patients have children and live with their families; three quarters are white collar workers or self employed; one quarter are skilled blue collar workers. 12 patients were suffering from the ailment for the first time; 12 patients were undergoing a relapse. Mean visus of the affected eye was 0.8. The Symptom List yielded an inconspicuous total score for psychosomatic symptoms. In the SCL 90-R, nine out of 24 patients (37%) evinced elevated psychic stress. The total value of the questionnaire on social support showed good social support. In the Sixteen Personality Factor Questionnaire, the patients showed heightened emotional instability and insecurity as well as flexibility and spontaneity.
Conclusion: The sociodemographic data confirm that central serous chorioretinopathy is predominantly an ailment of middle aged, socially well integrated men. This study suggests elevated psychic stress a few weeks after the onset of the ailment. The personality factors in the patients with central serous chorioretinopathy found in this study have to be verified with other populations. These results did not clearly show that psychosocial factors have a definite role in the aetiology of central serous chorioretinopathy. In order to make any clear assertions about this matter, further longitudinal studies on the progression of psychosocial parameters with larger patient samples would be indispensable.
Keywords: central serous chorioretinopathy, psychosomatic aspects
Since the original description of central serous chorioretinopathy (CSC) by von Graefe in 1866,1 a variety of aetiological factors and pathophysiological mechanisms have been discussed.2 The aetiology of CSC remains unclear to this day.3 Psychosomatic aspects of the ailment were pointed out long ago.4 Harrington5 and Zeligs6 reported a relatively high incidence of CSC among American naval personnel during the second world war. It was suggested that anxiety and acute psychological trauma have a definite role in precipitating the ocular disorder.5–8 In subsequent studies, it was shown that a high proportion of those suffering from CSC are young men.5–10
In the 1970s, Werry and Arends11 described a neurotic personality structure in patients with CSC which could not, however, be confirmed by later studies.12,13 A further study associated CSC with type A behaviour.10 Contradictory evidence has also been gathered regarding the number of life events before the onset of CSC.12,14–16 In the largest study with 230 patients, Tittl et al17 found psychopharmacological medication use (anxiolytic and antidepressive medication among 13% of the patients), corticosteroid use, and hypertension as factors associated with CSC. The authors speculate that increased sympathetic nervous system stimulation created by psychological stress may induce CSC.17 However, in this study psychological symptoms of the patients were not directly explored. In other studies, larger numbers of psychological and physical symptoms as well as lower social support were found in patients with CSC.12,13,15 Altogether, investigations conducted until now on the subject of psychosomatic aspects of CSC have yielded inconsistent results.
In the present study, psychosomatic symptoms at the time of onset of the ailment as well as the personality profile of patients with CSC were investigated in order to improve the evidence regarding these psycho-ophthalmological questions.
METHODS
Patients
Between July 1999 and September 2001, all patients (n=31) at the department of ophthalmology, Freiburg University Hospital, Freiburg, Germany, presenting with the diagnosis of central serous chorioretinopathy were consecutively enrolled in the study. After a complete ophthalmological examination (Snellen visual acuity, slit lamp, funduscopy) the diagnosis was based on typical symptoms (visual decrease, metamorphopsia) and findings (serous retinal elevation) and was confirmed by fluorescence angiography (leaking point). The patients were asked at least within 6 weeks after the initial onset of the symptoms to complete standardised psychometric questionnaires; 24 out of 31 patients (77.4%) answered the questionnaires. The main reasons for non-participation were fear of disclosure of private issues and negative attitude towards research. Table 1 shows the comparison between the patients included and the refusers. Among the responding patients there were more patients with a relapse of the CSC and the responding patients were, on the average, 7 years older.
Table 1.
Comparison between responders and non-responders within the 31 CSC patients
| Variable | Responder (n) | Non-responder (n) |
| Total | 24 | 7 |
| Age (mean/SD)* | 44.1 (7.2) years | 37 (5.7) years |
| Sex/male | 22/92% | 6/86% |
| Time between first manifestation and investigation (mean (SD)) | 6 (2.7) weeks | 6.7 (2.2) weeks |
| Relapse | 12/50% | 2/28.6% |
*Significant age difference in the t test (t=2.39; df=29; p=0.023).
As only standardised questionnaire instruments were employed, we used the available norm and comparative sample values instead of a control group.
The study was approved by the ethics review committee of Freiburg University. Informed consent was given by all subjects.
Psychometric instruments
Symptom Checklist (SCL 90-R)18,19
This is a questionnaire established in international research and clinical practice to ascertain psychic stress in a variety of symptomatic areas within the past 7 days. The questionnaire contains 90 items on a five degree Likert scale combining nine scales and a global severity index (GSI) as a measurement for total psychic stress. The instrument was normed using a standardising sample of 1006 normal people (mean age 34 years); the transformation into T values takes the demographic variables sex and degree of education into account. For the evaluation of the SCL-90-R, the threshold values for elevated psychic stress were established in the individual scales in accordance with the relevant norm samples (T values >60).
The Symptom List20
The Symptom List is a questionnaire used to establish the quantity of momentary subjective impairment due to non-specific physical symptoms not clearly the result of somatic diagnoses. The questionnaire is available in two parallel forms, B-L and B-L′, with 24 items each, to be crossed on a four level scale. Out of these 24 items, the total score is calculated as a measurement for the degree of impairment. The present study employed both parallel forms, so that high reliability of the results of the questionnaires may be assumed. Norming of the test values was performed on the basis of a norm sample of 1761 people representative for Germany with regard to age and sex.
The Sixteen Personality Factor Questionnaire (16 PF)21
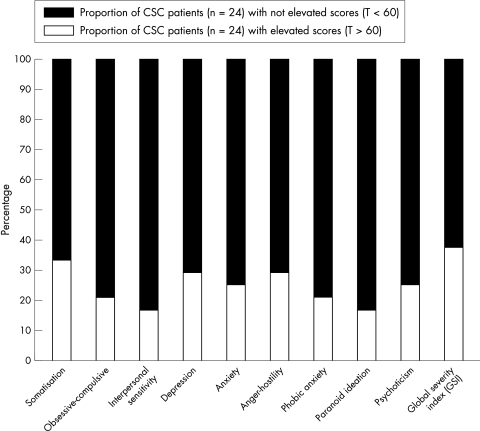
The Sixteen Personality Factor Questionnaire is an objective test for multidimensional personality diagnosis in adults. The original English version22 was translated into German, and validated in the German version.21 The test consists of 192 items on a three-level scale, comprising 16 primary personality dimensions. Norming of the test values was performed on the basis of a norm sample of 3250 people representative for Germany with regard to age and sex. For greater clarity, the raw values of the test are transformed into Sten values of a standard scale running from 1 to 10, with a mean value of 5.5 and a standard deviation of 2 (see Fig 2).
Figure 2.
Personality traits of the patients according to the PF 16 (mean transformed into Sten values).
Questionnaire on Social Support (F-Sozu, K-22)23
The questionnaire establishes, in abbreviated form with a total of 22 items on a five level Likert scale, the total degree of individual perception of social support and social integration. Comparative values from 14 samples in which the questionnaire was employed, are available. For the present study, a norm sample of a representative population with regard to age (n=864) was used.
Documentation of sociodemographic data
Sociodemographic data were recorded in a questionnaire routinely used in the department of psychosomatic and psychotherapeutic medicine, Freiburg University Hospital, establishing—apart from sociodemographic data such as age, sex, life situation, education, and working activity—information on sick leave and number of consultations with doctors.
Statistical analyses
Statistical analyses were carried out using the program spss 10.0 for Windows. Descriptive statistics were calculated for sociodemographic data, clinical data, and all psychometric tests. To establish group differences at the interval scale level, the t test for independent samples was employed. To calculate differences at nominal level, the χ2 test was used. All statistical tests were two sided and a level of p<0.05 was considered statistically significant.
RESULTS
Sociodemographic and clinical data
The sociodemographic data of the patient population are shown in Table 2.
Table 2.
Sociodemographic description of the patient population (n=24)
| Number of patients | ||
| Variable | Patient sample | No (%) |
| Age (years) | 24 | |
| Mean | 44.1 | |
| Median | 45.5 | |
| SD | 7.2 | |
| Range | 31–55 | |
| Sex | Male | 22 (92) |
| Life situation | Married/living with a partner | 18 (75) |
| Living alone | 6 (25) | |
| Children | Without children | 4 (17) |
| 1–3 children | 20 (83) | |
| Education | Elementary school | 7 (29) |
| Vocational school | 5 (21) | |
| High school/college | 12 (50) | |
| Working activity | Workers | 4 (17) |
| White collar workers/officials | 12 (50) | |
| Self employed | 6 (25) | |
| Others | 2 (8) | |
| Sick leave during the | None | 14 (58) |
| past year | Less than 3 months | 9 (38) |
| 3–6 months | 1 (4) | |
| Retirement | – | |
| Number of consultations during the past 2 years | 1–5 | 7 (29) |
| 6–10 | 10 (42) | |
| 11–20 | 7 (29) |
Twelve of 24 patients were suffering from an initial occurrence and 12 of 24 patients from a relapse of CSC. Mean visus of the affected eye was 0.8 (calculated from logMAR values, range 0.3–1, n=24). Twenty of 24 patients indicated metamorphopsia as a symptom. On average, initial symptoms of the CSC started 6 weeks (range 1–12 weeks) before the time when the data were gathered. None of the patients was regularly taking medication—particularly no corticosteroids or psychotropic medication.
Psychosomatic symptoms
The Symptom List showed a mean total score of 13.1 (SD 10.7; n=24). The patients with CSC thus showed values comparable to those of the norm sample (n=1761; mean 14.3; SD 10.8; t=0.54; df=1,783; p=0.588). The symptoms indicated were heartburn, pains in the neck and shoulders, worrying, inner tension, and lack of energy.
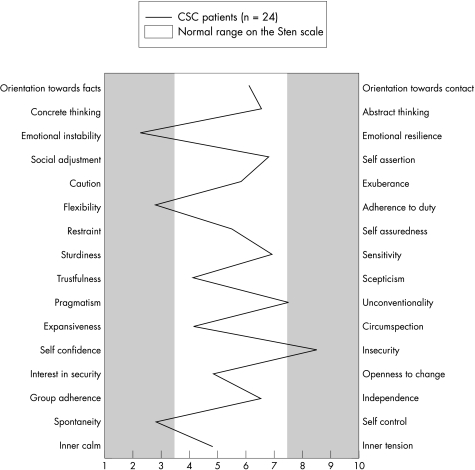
In the Symptom Checklist 90-R, nine out of 24 patients (37%) showed elevated psychic stress (GSI, T>60) (Fig 1). Most of the stress occurred on the somatisation (n=8; 33%), depression (n=7; 29%), and anger-hostility (n=7; 29%) scales (Fig 1).
Figure 1.
Proportion of the patients in the sample with elevated psychic symptoms according to the scales of the SCL 90-R and the Global Severity Index (GSI) (T>60).
Personality traits and social support
Establishing personality factors with the Sixteen Personality Factor Questionnaire (16 PF), the patients with central serous chorioretinopathy, compared with adults in a representative German population sample (n=3250), were shown to be more emotionally unstable and insecure, but also more flexible and spontaneous (Fig 2).
The mean total score (score range 1–5) of the Questionnaire on Social Support of the CSC patients (mean value 4.4; SD 0.4; n=24) was significantly higher than the mean value of the norm sample (n=864; mean 3.93; SD 0.71; t=3.23; df=886; p=0.0013).
DISCUSSION
The sociodemographic data of our sample confirm that CSC is mainly an ailment of socially well integrated middle aged men. By comparison with the nationwide average,24 a high proportion of the patients are either married or living in a steady relationship, they have a higher degree of education, and are working as white collar workers or officials. The patients had taken little or no sick leave and had not consulted physicians with conspicuous frequency in the course of the previous 2 years.
One third of the patients in our study showed elevated psychic stress. This indication referred to the previous 7 days—that is, several weeks after the onset of symptoms of CSC. It must therefore remain unclear to what extent, with some of the patients, heightened psychic stress was a result of the eye ailment, or existed previous to the outbreak of the illness and might be a causal factor. As the patients included are older than the original patient sample, the correlation between age and psychological stress was investigated. Only a weak statistic correlation (r=0.071) was shown, so that the psychological stress measured would not seem to be a function of age difference. Neither were any statistically significant differences shown in the results of any psychometric tests between patients with recurrent disease and patients with an initial attack of CSC.
Franke et al,15 in a study of 20 CSC patients, used a short form of the SCL 90-R to compare a sample of 20 patients suffering from ocular histoplasmosis with a control group comprising 40 healthy people. They also reported heightened mean psychological stress in patients with CSC compared with the comparative sample of patients with ocular histoplasmosis and the healthy control group, which hardly deviated from each other. It must be admitted, however, that the time of performance of the study of Franke et al was outside the period of illness.
While Tittl et al17 reported use of psychopharmacological medication and corticosteroids with significantly greater frequency than in a comparison group of patients with other ocular findings, this involved only 13% of the patients with CSC. In our sample, none of the patients was taking comparable medication.
Compared with the results of Conrad et al13 in the Symptom List20 (n=35; mean total score 18.5; SD 11.1), the patients in our study showed fewer non-specific physical symptoms (t=1.86; df=57; p=0.067), and may be considered inconspicuous in this regard. Conrad et al, in their study of 35 CSC patients, elicited a very significantly higher symptom level, compared with a control group of 21 patients with traumatic eye diseases. By comparison with this control group, the CSC patients in our study also had a higher mean rating on the Symptom List; this difference, however, was not statistically significant (t=1.186, df=43, p=0.242).
High social support was found, corresponding well with our patients’ sociodemographic characteristics. In their study using the same questionnaire, Franke et al15 found a significantly lower mean social support value (n=20; mean 3.8; SD 0.7; t=3.56; df=42; p=0.0009) than in our study. Franke et al also found low social support of CSC patients compared both with patients suffering from ocular histoplasmosis and healthy control persons,15 while our patients’ mean values for social support did not differ from these comparative samples. Here, too, it must be mentioned that the measurement of Franke et al did not take place during the acute stage of the ailment, so that these results are not directly comparable with those of our study.
Emotional instability, insecurity, and nervousness have—compared both with healthy norm populations and patients with other eye ailments—previously been described as personality traits of patients with CSC.11–13 This was also shown by the patients in our sample, who, however, were particularly spontaneous and flexible as well. These results may permit the hypothesis that these are personalities in whom openness and spontaneity on the one hand and insecurity on the other hand can give rise to inner conflicts. Such an interpretation can of course only be considered as a hypothesis which must be tested with a larger sample of patients. Owing to the small case number in our investigation, it can by no means be considered to be generally valid—as it unfortunately and erroneously was in Werry and Arends’s study of 31 patients.11
Altogether, the problem remains that investigations of CSC with a prospective study design, such as our own study, only attain small case numbers because the ailment is so rare.11–13 All the studies with larger samples between 50 and 350 patients were conducted as retrospective investigations, leading to considerable methodological difficulties in establishing modification sensitive psycho-ophthalmological parameters.15–17,25
The significance of the psychosomatic aspects of CSC, in the light of the results of our own study and those reported in previous literature, remains inconsistent. It therefore does not seem to be scientifically substantiated that psychosocial factors have a dominant role in the etiology of CSC.
Taken strictly, the testing of the hypothesis that previous cumulative psychological stress over a period of months and the resultant raised levels of endogenous stress hormones decisively influence the onset of CSC would require a measurement of modification sensitive psychological parameters before the outbreak of the ailment. Recruiting such samples, however, presents a basic methodological problem. In any event, the development of the conspicuous psychological stress measured in one third of the patients in our study should be investigated across time. This would require longitudinal studies permitting statements regarding the course of the physical and psychological symptoms, establishing possible connections between personality traits and the course of central serous chorioretinopathy. It would therefore seem important to evaluate the degree to which these parameters are altered in patients with other types of eye diseases.
REFERENCES
- 1.Graefe A von. Über zentrale rezidivierende Retinitis. V Graefes Arch Ophthal 1866;12:211. [Google Scholar]
- 2.Trichtel F. Zur Ätiologie der Retinopathia centralis serosa. Wiener Med Wochenschrift 1980;15/16:533–8. [PubMed] [Google Scholar]
- 3.Marmor MF. On the cause of serous detachments and acute serous chorioretinopathy. Br J Ophthalmol 1997;81:812–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Niklewski G. Psychosomatische Erkrankungen des Auges. Eine Übersicht Zschr psychosom Med 1982;28:300–31. [PubMed] [Google Scholar]
- 5.Harrington DO. Psychosomatic interrelationship in ophthalmology. Am J Ophthalmol 1948;31:1241–51. [DOI] [PubMed] [Google Scholar]
- 6.Zeligs MA. Central angiospastic retinopathy. A psychosomatic study of its occurrence in military personel. Psychosom Med 1947;9:110–17. [PubMed] [Google Scholar]
- 7.Schlaegel TF. Psychosomatics: the second face of ophthalmology. Int Ophthalmol Clin 1968,8:409–85. [PubMed] [Google Scholar]
- 8.Hartmann ME. La retinopathie centrale angiospastique. Bull Soc Ophtalmol Fr 1952:110–20. [PubMed]
- 9.Lipowski ZJ, Kiriakos RZ. Psychosomatic aspects of central serous retinopathy: a review and case report. Psychosomatics 1971;12:398–401. [DOI] [PubMed] [Google Scholar]
- 10.Yanuzzi LA. Type-A behavior and central serous chorioretinopathy. Retina 1987,7:111–30. [DOI] [PubMed] [Google Scholar]
- 11.Werry H, Arends C. Untersuchung zur Objektivierung von Persönlichkeitsmerkmalen bei Patienten mit Retinopathia centralis serosa. Klin Monatsbl Augenheilkd 1978;172:363–70. [PubMed] [Google Scholar]
- 12.Bahrke U, Krause A, Walliser U, et al. Retinopathia centralis serosa—Magengeschwür der Augenheilkunde? Psychother Psychosom Med Psychol 2000;50:464–9. [DOI] [PubMed] [Google Scholar]
- 13.Conrad R, Bodeewes I, Schilling G, et al. Chorioretinopathia centralis serosa und psychische Belastung. Ophthalmologe 2000;97:527–31. [DOI] [PubMed] [Google Scholar]
- 14.Bennett G. Central serous retinopathy. Br J Ophthalmol 1955;39:605–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Franke GH, Esser J, Stäcker K-H, et al. Die gefilterte Normalität: Psychologische Ursachen und Folgen von spezifischen Netzhauterkrankungen. Psychother Psychosom med Psychol 1996;46:159–68. [PubMed] [Google Scholar]
- 16.Franke GH, Esser J, Stäcker K-H, et al. Über den Zusammenhang zwischen Krankheitsprogredienz und Stressverarbeitung bei Patienten mit Retinopathia centralis serosa. Psychother Psychosom med Psychol 1998;48:215–22. [PubMed] [Google Scholar]
- 17.Tittl MK, Spaide RF, Wong D, et al. Systemic findings associated with central serous chorioretinopathy. Am J Ophthalmol 1999;128:63–8. [DOI] [PubMed] [Google Scholar]
- 18.Derogatis LR. Symptom Checklist-90-R (SCL-90-R), scoring and procedures manual-I for the revised version. Johns Hopkins School of Medicine Goldbeck, 1977.
- 19.Franke, G. SCL-90-R. Die Symptom Checklist von Derogatis. German Version. Weinheim: Beltz-Test, 1995.
- 20.Zerssen D v. The Symptom List—Die Beschwerden-Liste. Fragebogen und Manual. München: Beltz-Test, 1975
- 21.Schneewind KA, Schröder G, Cattell RB. The Sixteen Personality Factor Questionnaire (16 PF). Test manual. 2nd ed. Bern, Stuttgart, Toronto: Verlag Hans Huber, 1985
- 22.Cattell RB, Eber HW, Tatsuoka MM. Handbook for the Sixteen Personality Factor Questionnaire (16 PF). Champaign: Institute for Personality and Ability Testing (IPAT), 1970.
- 23.Sommer G, Fydrich T. Questionnaire on social support (F-Sozu). Diagnostik, Konzepte. Tübingen: Dt Gesellschaft für Verhaltenstherapie, 1989.
- 24.German Statistical Office, informations of the year 2002, www.destatis.de/themen/d/thm_bevoelk.htm
- 25.Gäckle HC, Lang GE, Fressler KA, et al. Chorioretinopathia centralis serosa. Der Ophthalmologe 1998;95:529–53. [DOI] [PubMed] [Google Scholar]