Abstract
Aims: To present transcaruncular medial orbitotomy as the preferred approach to manage frontoethmoid mucoceles.
Methods: 11 patients with frontoethmoid mucoceles received transcaruncular orbitotomy from 2000 to 2002 at the National Taiwan University Hospital. The incision was made through the caruncle to explore the medial wall periosteum. Then the periosteum was opened and extended to provide adequate surgical field exposure. Frontoethmoid mucoceles could be viewed and removed directly. A transnasal drainage tube was inserted before closure of the caruncle wound.
Results: The mean follow up period was 12 (SD 9.1) months (range 1–26). Both functional recovery and cosmetic outcome were excellent. There was no recurrence of mucoceles. One patient complained of diplopia, which subsided after 2 months.
Conclusion: Transcaruncular orbitotomy provides a wide exposure and a safe access to the medial orbital extraperiosteal space. Furthermore, there is less damage to skin and muscle layer and less manipulation of other ocular adnexal structures, such as medial canthal tendon and lacrimal sac. It can be an excellent approach for the management of frontoethmoid mucoceles.
Keywords: lynch incision, frontoethmoid mucoceles, oculoplastic flap surgery, transcaruncular approach
Paranasal sinus mucoceles are slowly expanding cystic lesions with pseudostratified ciliated columnar epithelium. They are caused by obstruction of the normal sinus ostea and entrapment of the secretory epithelium, which continues to secrete mucus, filling the normal aerated space and exerting pressure on the surrounding bony structures.1 This leads to effacement of the normal septae, expansion of the sinus, thinning of the bony wall, and ultimately extension through the wall into the adjacent orbit, nasopharynx, or cranial cavity. The cysts are usually filled with clear to slightly yellowish thick mucoid secretions.
Most mucoceles arise from the frontal or ethmoid sinuses or both. They occur at any age in both sexes. However, the majority of them are seen between the fourth and seventh decades. Frontoethmoid mucoceles cause outward and downward displacement of the globe, and are often associated with fullness in the superonasal and medial canthal region with a palpable mass. The expanding mass lesion may result in proptosis, eye motility disturbance, diplopia, visual loss, orbital pain, or headache.2
Management of mucoceles includes complete removal of the cystic lining, re-establishment of normal drainage, or obliteration of the sinus by mucosal stripping and packing with bone or fat. This is usually the domain of the otorhinolaryngologist, but the ophthalmological expertise may be necessary for management of the orbital portion.
There are several surgical approaches to frontoethmoid sinus. The most commonly used approach by the oculoplastic surgeon is that of Lynch.3 Here, we describe another technique, the transcaruncular approach, which affords a rapid entry to the medial orbit and less damage to the adnexal structures, and achieves superior cosmetic results.4–7
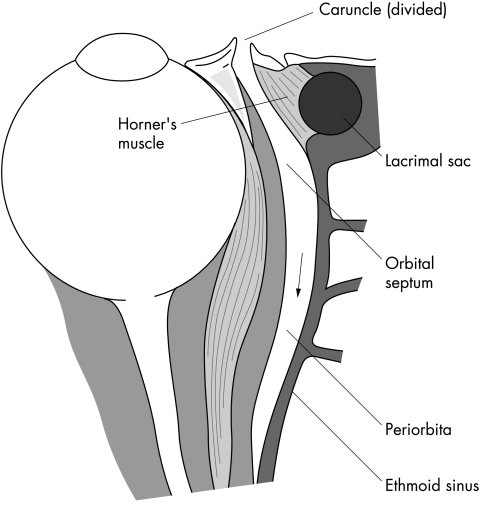
The anatomy relating to transcaruncular medial orbitotomy is shown in Figure 1. The posterior fibres of the pretarsal orbicularis muscle are known as Horner’s muscle. It inserts on the posterior lacrimal crest and ensures proper posterior apposition of the eyelids to the globe.4,7 After an incision through the caruncle, a natural plane would be dissected between Horner’s muscle and the medial orbital septum to expose the medial orbit. This approach could avoid manipulation of the lacrimal sac and medial canthal tendon.
Figure 1.
The anatomy related to the transcaruncular medial orbitotomy. The caruncle was divided to dissect a plane between Horner’s muscle and the medial orbital septum to expose the medial orbit, avoiding manipulation of lacrimal sac.
SUBJECTS AND METHODS
Eleven patients with frontoethmoid mucoceles underwent transcaruncular orbitotomy from 2000 to 2002 at the National Taiwan University Hospital. The surgery was performed with the patients under general anaesthesia. The medial and superior subconjunctival planes were infiltrated with approximately 3 ml of 2% Xylocaine with 1:100 000 adrenaline. Retraction of upper and lower lids by an eyelid speculum was performed, taking care to avoid damage to either lacrimal puncta or canaliculi. Once the area was well exposed, the first incision was made through the caruncle using Westcott scissors (Fig 2A). The traction sutures on lateral part of the caruncle incision wound were made by 4-0 silk to provide a wider surgical view. A curved Stevens scissors was then inserted into the incision with the tips placed on the posterior lacrimal crest. Gentle dissection with the tips of the scissors over the posterior lacrimal crest in an anteroposterior direction helped to identify the posterior side of the posterior lacrimal crest (Fig 2B). Blunt dissection with scissors and retraction of the orbital contents with a malleable ribbon retractor resulted in exposure of the medial periosteum and some yellowish mucoid material being encountered (Fig 2C). A Desmarres lid retractor was used at the medial edge of conjunctiva to enhance exposure. The eggshell-like, rounded mucoceles could be palpated after exposure of the medial orbit (Fig 2D). The thin walled mucoceles were easily penetrated with front biting forceps. After the yellowish mucoid material was suctioned out, the thin bone lined lesion was then excised together with the mucous membrane in a piecemeal manner with front biting forceps (Fig 3A and B). The entire mucocele floor was removed and the orbital rim was trimmed to a smooth contour. The mucous membrane was curetted from the sinus lining (Fig 3C). Because the mucoceles were formed by an obstructive sinus process, adequate drainage of the sinus had to be re-established into the nasal cavity. We did not manage the occluded frontal duct. However, we created a new communication from the frontal sinus through the ethmoid sinus into the intranasal cavity. This was done with the use of a haemostat introduced intranasally that penetrates into the mucocele cavity. The intranasal wall of the ethmoid area of the mucocele was excised; then a rubber catheter could be inserted from the frontal sinus through the ethmoid sinus into the nasal cavity (Fig 3D). The catheter was left in position for at least 7–10 days (Figs 4C, 5C). At the end of the procedure, the caruncle and conjunctiva were closed with interrupted 6-0 Vicryl sutures.
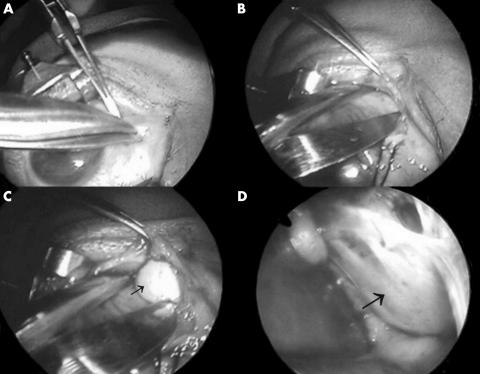
Figure 2.
(A) The first incision was made through the caruncle using Westcott scissors. (B) Gentle dissection with the tips of the scissors passed along the plane between Horner’s muscle and the medial orbital septum. (C) Retraction of the orbital contents with a malleable ribbon retractor resulted in exposure of the medial orbit and some mucoid material encountered (arrow). (D) The eggshell-like, rounded mucocele was shown (arrow).
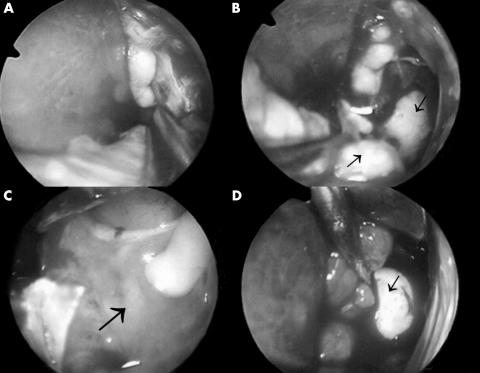
Figure 3.
(A) The outer wall of the mucocele was removed by forceps. (B) Yellowish mucoid material (arrows) was found after removal of outer shell of the mucocele. (C) The inner wall of the mucocele was shown (arrow). (D) A rubber catheter with a balloon (arrow) was inflated after excision of the mucocele.
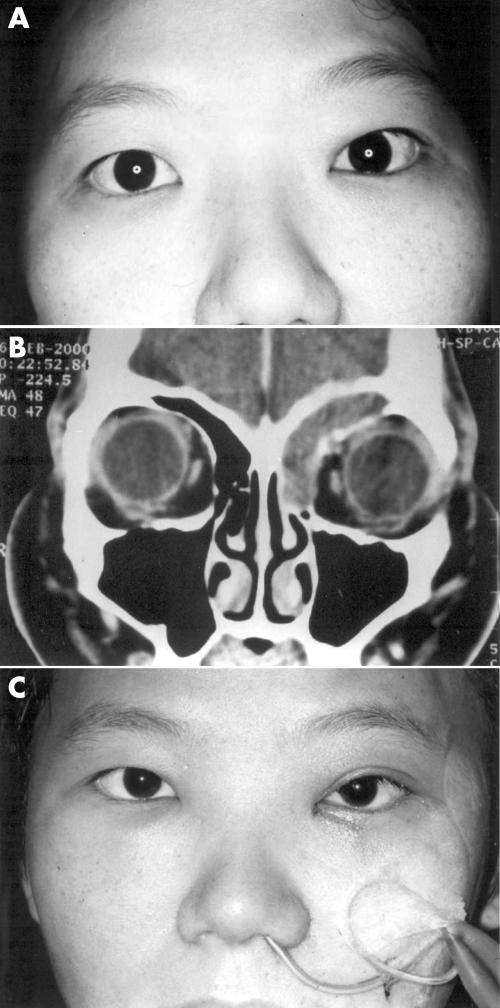
Figure 4.
A 31 year old woman (A) with a tender mass in the left superior medial orbit before operation, (B) CT scan findings showing a frontoethmoid mucocele, (C) a transnasal drainage tube in position.
Figure 5.
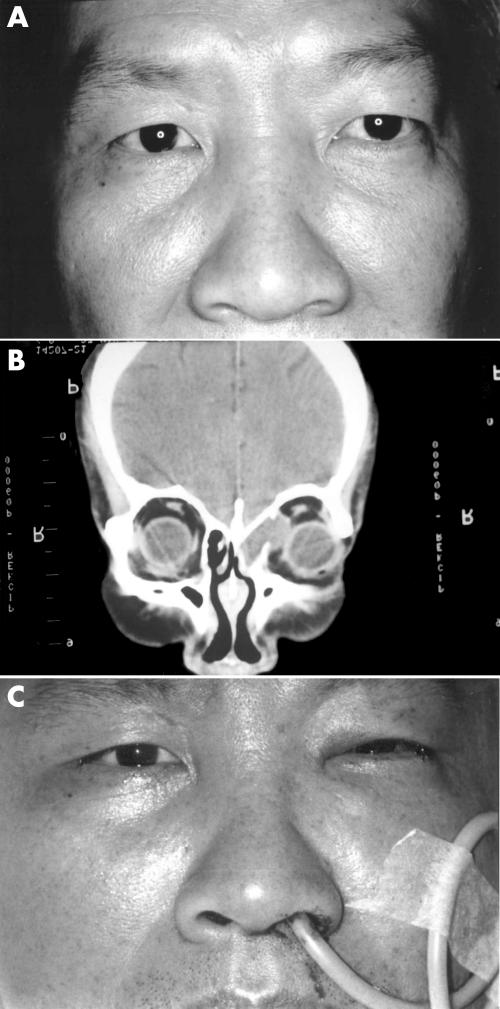
A 58 year old man (A) with left proptosis and exotropia before operation, (B) CT scan findings showing a mucocele extending to the orbital cavity, (C) a transnasal drainage tube in position.
RESULTS
The clinical features of 11 patients with frontoethmoid mucoceles after transcaruncular approach are summarised in Table 1. The mean follow up period was 12 (SD 9.1) months (range 1–26). At the end of follow up, both functional recovery and cosmetic outcome were excellent. No major complications and recurrences were observed. Only transient vertical diplopia was found in one patient after the operation, and diplopia subsided after 2 months. No sequelae were noted in this patient. Possible explanation for this mild complication was minor damage of superior oblique muscle during the surgery.
Table 1.
Clinical features of all 11 patients
| Patient No. | Age | Sex | Laterality | Presenting symptoms and signs | Complications | Follow up (months) |
| 1 | 31 | F | OS | Palpable mass | None | 26 |
| 2 | 58 | M | OS | Periorbital fullness and dull pain, diplopia | None | 24 |
| 3 | 51 | M | OS | Proptosis, supranasal pain | None | 24 |
| 4 | 80 | F | OD | Proptosis, diplopia | None | 15 |
| 5 | 39 | F | OD | Proptosis | None | 12 |
| 6 | 63 | F | OS | Proptosis | None | 10 |
| 7 | 34 | F | OD | Diplopia | Transient diplopia | 7 |
| 8 | 30 | M | OU | Palpable mass, periorbital pain and tenderness | None | 7 |
| 9 | 35 | M | OS | Proptosis, periorbital pain | None | 5 |
| 10 | 30 | F | OD | Proptosis | None | 1 |
| 11 | 55 | M | OS | Palpable mass, periorbital pain | None | 1 |
Here we describe two of our cases.
Case 1
This 31 year old woman had complained left upper medial eyelid swelling for about 2 months (Fig 4A). Visual acuity was 20/20 in both eyes with correction. Intraocular pressures were 13 mm Hg bilaterally. Examination showed a smooth fluctuant, tender mass in the left superior medial orbit. There was no evidence of pulsation or bruit. No lesion was seen in the left superior fornix. Exophthalmometry measurements were the same bilaterally. There was no conjunctival injection or chemosis. Extraocular eye movements were full and free. Visual fields and fundi were normal. Orbital computed tomograph (CT) scan views of sinuses were consistent with a mucocele of the left frontoethmoid sinuses without extension to the orbit and the cranial cavity (Fig 4B).
A transcaruncular medial orbitotomy was performed without complications, and the patient’s postoperative course was uneventful (Fig 4C). Her final result was both cosmetically and functionally satisfactory. No recurrence was found after 26 months’ follow up.
Case 2
For 1 week, this 58 year old man had a sensation of fullness in the left eye, binocular diplopia, and left periorbital dull pain, especially during eye movement (Fig 5A). Visual acuity was 20/20 bilaterally with correction. Intraocular pressures were 15 mm Hg bilaterally. Examination showed a smooth, fluctuant tender mass in the left medial orbit. There was no pulsation or bruit. Hertel exophthalmometry measurements were 14 mm right eye and 18 mm left eye. Primary eye position was left exotropia. Extraocular muscle movements were full and free in the right eye, but showed limitation at upper and medial gaze in the left eye. Visual fields and fundi were normal. Orbital CT scan showed a mass protruding into the orbit from left ethmoid sinus with displacement of medial rectus muscle (Fig 5B). No cranial cavity involvement was noted.
A transcaruncular medial orbitotomy was done without complications (Fig 5C). Postoperatively the patient had an uneventful recovery. The final cosmetic and functional results were satisfactory. There was no recurrence after 24 months’ follow up.
DISCUSSION
In the past, virtually all mucoceles were treated by two main transcutaneous approaches.3,8–10 The first one is the Lynch incision, an incision over the superomedial orbital rim. It is used most commonly to enter the superomedial orbit for removal of the frontoethmoid mucoceles by British surgeons.3,8 The second choice is the osteoplastic flap obliterative procedure, particularly favoured in the United States, with coronal or transcutaneous incision through the glabella to the anterior wall of the frontal sinus to obliterate the air space with dermal fat.9,10 Disadvantages of the Lynch incision are obvious skin scarring near the medial canthus, disinsertion of the medial canthal tendon, or the possibility of damage to the lacrimal sac.4,5 An exacerbation of diplopia might occur following the Lynch incision. It is caused by direct trauma to the trochlea of the superior oblique muscle or scarring of adjacent structures.2 To avoid the visible skin scar resulting from the Lynch incision, a coronal approach in which an incision is made across the scalp posterior to the hairline is another choice. Although it provides optimal exposure of the frontoethmoid bone, the incision is large, the forehead flap dissection is time consuming and complicated by scalp numbness, hair loss, flap haematoma, and frontalis palsy. An upper lid crease approach is chosen over both the typical Lynch incision and the transcutaneous glabella incision to optimise scar placement and minimise the potential for prominent scar formation. Complications include asymmetry or deformity of the upper lid crease or upper lid fold, and trauma to the anatomical structures in the superior orbit.
Endoscopic sinus surgery has been practised by otorhinolaryngologists since the 1980s.11 The goals of endoscopic sinus surgery are to develop a wide and patent sinus-nasal communication, to prevent possible causes of recurrent obstruction, and to provide optimal conditions for re-epithelialisation of sinus and the outflow tract.12 Reduced hospital stay and cosmetic satisfaction are the main advantages. Some of the potential complications in the Lynch incision could be avoided.13 Contraindications include lesions located at the lateral frontal sinus, excessive sclerosis of the bone, and large osteomas.12 Intracranial, intranasal, and orbital complications have been reported. Possible ophthalmic complications include rupture of lamina papyracea, damage to the medial rectus muscle, and optic nerve trauma.14,15
The transcaruncular approach to the medial orbit provides wide exposure and safe access to the medial extraperiosteal space.4–7 Potential advantages over the classic transcutaneous incision include more rapid entry into the orbit, less damage to skin and muscle layers, and a better cosmetic result owing to the reduced likelihood of postoperative scarring. Furthermore, there is less manipulation of other ocular adnexal structures such as the medial canthal tendon and lacrimal sac and, consequently, reduced likelihood of damage to theses structures.
Some precautions should be considered to reduce possible complications.4,5,7 The need for careful edge to edge closure of the conjunctiva to decrease the postoperative formation of medial caruncular scar tissue that can grow to involve the lacrimal puncta or canaliculi, to avoid conjunctiva granuloma, prolonged chemosis, or inclusion cyst. As the medial orbit is approached, caution must be exercised to avoid disruption of the lacrimal system. It is important to be constantly aware of pressure on the globe and other orbital contents during retractions for adequate surgical exposure. Because mucocele formation is an obstructive sinus process, complete removal of epithelial lining and adequate drainage of the sinus into the nasal cavity are important. In our cases, keeping the drainage tube in position at least for 7–10 days is enough to reduce recurrence.
In conclusion, transcaruncular medial orbitotomy is well suited to surgical management of frontoethmoid mucoceles. Advantages over other approaches include cosmetically satisfactory results, less damage to adjacent tissue, and wide exposure and rapid access to the medial orbit.
REFERENCES
- 1.Evans C. Aetiology and treatment of frontoethmoidal mucocele. J Laryngol Otol 1981;95:361–75. [DOI] [PubMed] [Google Scholar]
- 2.Valerie JL, Muriel ER. Ophthalmic considerations in fronto-ethmoid mucoceles. J Laryngol Otol 1989;103:667–9. [DOI] [PubMed] [Google Scholar]
- 3.Lynch RC. The technique of a radical sinus operation which has given me the best result. Laryngoscope 1921;31:1–5. [Google Scholar]
- 4.Balch KC, Goldberg RA, Green JP, et al. The transcaruncular approach to the medial orbit and ethmoid sinus. A cosmetically superior option to the cutaneous (Lynch) incision. Facial Plast Surg Clin North Am 1998;6:71–7. [Google Scholar]
- 5.Garcia GH, Goldberg RA, Shorr N. The transcaruncular approach in repair of orbital fracture: a retrospective study. J Cranio Maxillofac Trauma 1998;4:7–12. [PubMed] [Google Scholar]
- 6.Shorr N, Baylis HI, Goldberg RA, et al. Transcaruncular approach to the medial orbit and orbital apex. Ophthalmology 2000;107:1459–63. [DOI] [PubMed] [Google Scholar]
- 7.Lai PC, Liao SL, Jou JR, et al. Transcaruncular orbitotomy—a new approach to the medial wall. J Tzu Chi Med 2001;13:211–16. [Google Scholar]
- 8.Jhon SR, Valerie JL, Barbara S. Frontoethmoidectomy in the treatment of mucoceles. Arch Otolaryngol Head Neck Surg 1986;112:434–6. [DOI] [PubMed] [Google Scholar]
- 9.Goodale RL, Montgomery WW. Experiences with osteoplastic anterior wall approach to frontal sinus, case histories and recommendations. Arch Otolaryngol 1958;68:271–83. [DOI] [PubMed] [Google Scholar]
- 10.Gary AH, Richard KD, James B. Treatment of frontal sinus mucoceles with the osteoplastic flap technique. Ophthalmic Surg 1978;9:40–66. [PubMed] [Google Scholar]
- 11.Kennedy DW, Josephson JS, Zinreich SJ, et al. Endoscopic sinus surgery for mucoceles: a viable alternative. Laryngoscope 1989;99:885–95. [DOI] [PubMed] [Google Scholar]
- 12.Valerie JL. Endoscopic management of paranasal sinus mucoceles. J Laryngol Otol 1998;112:36–40. [DOI] [PubMed] [Google Scholar]
- 13.Gady HE, Frank EL. Endoscopic intranasal frontal sinusotomy. Laryngoscope 1995;105:440–3. [DOI] [PubMed] [Google Scholar]
- 14.Rene C, Rose GE, Lenthall R, et al. Major orbital complications of endoscopic sinus surgery. Br J Ophthalmol 2001;85:598–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neuhaus RW. Orbital complications secondary to endoscopic sinus surgery. Ophthalmology 1990;97:1512–18. [DOI] [PubMed] [Google Scholar]