Abstract
Aim: To analyse the test characteristics of orthoptic screening for amblyopia or amblyogenic risk factors (target conditions) in kindergarten.
Methods: 1180 three year old children were screened by orthoptists in 121 German kindergartens. Orthoptic screening consisted of cover tests, examination of eye motility and head posture, and monocular visual acuity testing with the Lea single optotype test. Children were re-examined in kindergarten by different orthoptists after 3–6 months using a more demanding pass threshold for visual acuity. All children with at least one positive orthoptic test result or an inconclusive re-examination were referred to an ophthalmologist for diagnosis. The gold standard was set positive if a target condition was diagnosed on ophthalmological examination. It was set negative if no target condition was found upon ophthalmological examination, or if a child who screened negative or inconclusive passed the orthoptic re-examination without any positive test result.
Results: The gold standard was ascertained in 1114 children. 26 (2.3%) children had a “positive” gold standard. In 10.8% of the children the initial screening was “inconclusive,” mostly due to lack of collaboration. Screening test sensitivity (based on conclusive results only) was 90.9% and specificity was 93.8%.
Conclusions: Orthoptic vision screening of 3 year olds in kindergarten is sensitive and specific. However, owing to a substantial proportion of inconclusive screening results, rescreening of non-cooperative 3 year old children should be considered.
Keywords: preschool vision screening, amblyopia, kindergarten
The main purpose of preschool vision screening is to detect amblyopia so early that treatment is likely to be still effective.1,3 The fourth year of life is considered best for vision screening as from this age onwards in most children monocular visual acuity can reliably be assessed by simple screening methods.4,6 In Germany, vision assessment is part of the general preventive care examinations conducted by general practitioners and paediatricians, and is paid for by the statutory health insurance. The effectiveness of this programme with respect to the detection of amblyopia is considered insufficient,7,8 since general practitioners and paediatricians lack experience with ophthalmological tests.9 Screening by orthoptists has been studied as an option to improve the sensitivity and specificity of preschool vision screening,10,14 because orthoptists are familiar with visual acuity and cover testing in children. Because in Germany about 50% of children enter kindergarten at age 3, and more that 80% attend kindergarten at age 4,15 kindergarten offers easy access to large numbers of children without efforts from the parents. Vision screening has been conducted successfully in German kindergartens before.16,18 Yet, little is known about the test characteristics of orthoptic vision screening performed in German kindergartens. The purpose of this study was to determine the test characteristics of orthoptic vision screening for untreated amblyopia or amblyogenic risk factors performed on 3 year olds in kindergarten prospectively. Therefore, a community based study was conducted which aimed at recruiting a representative sample of 3 year old children to be screened in real world kindergarten settings. The evaluation of screening tests performed in a community are prone to be affected by examination, or verification, bias.19,20 This bias is introduced if the diagnosis for patients with different screening test results is not equally likely to be confirmed by a gold standard evaluation. Verification bias has been shown to be frequent in paediatric studies.21 In particular, if the gold standard evaluation inconveniences the parents, or if it is associated with possible side effects, children who screened positive will be more likely to have a gold standard evaluation than children who screened negative. This bias results in sensitivity being erroneously inflated, and specificity being falsely reduced.22 Thus, the design of this study aimed at avoiding verification bias by using a practicable gold standard evaluation which was likely to be obtained for all children in the study.
METHODS
The institutional review board approved the study design which followed the tenets of the Declaration of Helsinki.
Study population
In order to recruit a representative study sample, local and regional kindergartens in two counties of south west Germany (Tübingen and Reutlingen) were contacted systematically. The management and parents of 121 kindergartens opted for participation in the study. All 3 year old children (after the third, before the fourth birthday) attending these kindergartens were eligible. Their parents or legal guardians were asked for informed consent in writing. The exact number of eligible children could not be ascertained owing to personal data protection legislation which required that access to the parents had to be obtained through the kindergarten staff. However, the participating kindergarten management and staff welcomed vision screening and were highly committed to recruit all eligible children. According to the kindergarten staff, nearly all parents of eligible children agreed to let their child(ren) participate. To the best of our knowledge, only one mother of a strabismic child who was already being treated refused to let her child participate, and consent could not be obtained from a few parents who did not speak and/or write German well enough to complete the consent form, despite the help offered by the kindergarten staff. The resulting dropouts may be estimated at a maximum of 10 children. Therefore, we concluded that nearly all eligible children were enrolled and no significant bias resulted.
A succinct history of each child (known ocular diseases, wearing of glasses, current ophthalmological treatment) was collected from the parents on the consent form. Children were recruited regardless of their history; 1184 children recruited for the study received an orthoptic screening in kindergarten between July and December 1999 (phase I). Less than 10% of the children who were enrolled could not be examined on the scheduled day owing to absence (illness, vacation, or other). In four children examined, the birth date was not ascertained until February 2001, and verification was impossible because the families moved. These four children (all without pathology in the orthoptic examinations) were excluded from this analysis, resulting in a sample size of 1180. The mean age was 42.7 months, 50.6% were male.
Children already treated for amblyopia
Among the 1180 children examined and included, there were 21 (21/1, 180 = 1.8%, 95% CI 1.0% to 2.5%) who had already been treated for amblyopia, of whom 11 had large angle strabismic amblyopia and 10 were of refractive/anisometropic origin. This was verified by comparing the ophthalmological records with the information provided by the parents. For these children the gold standard which is explained in the following paragraphs was rated “negative,” since they were already treated. They were excluded from the sample for the calculation of the specificity of screening in order to avoid a bias towards false “positives.”
STUDY DESIGN
Orthoptic screening
Orthoptic screening was performed by five experienced orthoptists and consisted of four items. Results could be rated “positive” (any pathology), “negative” (within normal limits), or “inconclusive” (insufficient cooperation or unclear, borderline result) with the following criteria:
inspection of the anterior eye segment, “positive”: any potentially vision threatening macroscopic organic anomaly other than ocular misalignment or eye motility disorder
unilateral and alternate cover, and uncover tests at near and at distance, “positive”: manifest strabismus or unstable re-fusion upon uncovering
examination of eye motility and head posture, “positive”: any detectable anomaly
uncorrected monocular visual acuity testing with the Lea single optotype test at 3 metres/10 feet (single symbol book No 2506, Precision Vision, Villa Park, IL, USA) and an eye patch, “positive”: visual acuity £0.4 (10/25), OR if line difference >1 line and visual acuity in the worse eye equal 0.5 (10/20) to 0.63 (10/17) (L Hyvärinen, Lea Test Ltd, Helsinki, Finland, personal communication, 10 October 1998).23
The starting visual acuity was 0.4 (10/25). To pass a line, three out of four symbols (3/4) had to be identified correctly. If the child hesitated or seemingly guessed without concentrating on the symbols, or identified only two symbols correctly—for example, because it was unfamiliar with forced choice testing, it was shown another symbol except for the circle/“ball.” Then three correct symbols out of five (3/5) were accepted to pass the line with the final visual acuity of that eye.
For completeness, we mention that corrected visual acuity was also measured if children had brought their glasses and were cooperative enough to be tested a second time after uncorrected visual acuity testing. However, since all children were to be examined under the same conditions, and regardless of history, the measurement of corrected visual acuity was not used for study purposes but rather to be able to inform parents of their children’s corrected visual acuity—that is, for ethical reasons.
To save time, visual acuity testing of an eye was discontinued when 1.0 (10/10) was reached. Otherwise, visual acuity testing criteria followed the recommendations of the manufacturers’ user instructions.
Visual acuity testing would be performed under varying indoor lighting conditions because of season and weather. Therefore, the orthoptists were instructed to adjust the shades, and to seat the children in a way to avoid direct sunlight and high contrasts if there was bright sunlight; if the light level was low, a portable glass shielded 150 W halogen reflector lamp was used to light up the place from which the visual acuity test was shown. In 26 kindergartens, the ambient light level was monitored with a radiometer (Universal Photometer, Hagner, Solna, Sweden). It was ascertained that this procedure entailed photopic light levels (all measurements above 10 cd/m2, average 132 cd/m2).
In order to improve cooperation, the staff of the kindergarten were asked to train the children for the visual acuity testing, with photocopies of the Lea symbols. Parents were asked not to be present in kindergarten during the examination sessions. In the following text, “positive” and “negative” orthoptic examination results were also labelled “conclusive,” as opposed to “inconclusive” results.
Screening outcome
Orthoptic examinations were rated
“referral,” if any screening item was “positive”;
“no referral” if all screening items were within normal limits—that is, “negative”; or
“inconclusive” if cooperation was insufficient for at least one screening item, or if the result was ambiguous.
Gold standard
In this community based study, a mandatory ophthalmological gold standard examination with cycloplegia would most likely not have been acceptable to a considerable proportion of parents. These parents would either not let their child participate in the study at all, resulting in a non-representative study sample, or they would tend not to comply with the ophthalmological examination if the child screened negative, resulting in verification bias as described earlier. In order to avoid these types of selection bias, a practicable gold standard was defined which was likely to be obtained for all children in the study population.
Orthoptic examination
As part of the gold standard procedure, the study population was re-examined in kindergarten after 3–6 months by a different orthoptist (phase II) with a more demanding threshold for uncorrected monocular visual acuity of >0.63 (10/17) in either eye to pass the examination (that is, to be rated “no referral”). Children who only reached 0.5 (10/20) or 0.63 (10/17) in either eye were classified “borderline” which entailed referral for gold standard purposes. The other outcomes of the orthoptic examination were the same as in the screening phase I. The orthoptist in phase II was masked to the results in phase I. However, the orthoptist in phase II had the same history information as in phase I.
If the orthoptic screening (phase I) resulted in “no referral” or “inconclusive,” and the orthoptic examination (phase II) resulted in “no referral,” then the gold standard was set “negative.”
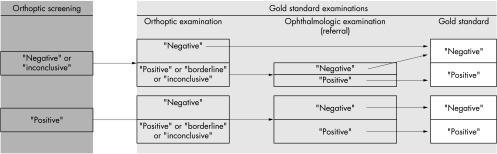
Figure 1 summarises how the gold standard was established starting from the results of the orthoptic screening.
Figure 1.
Flow diagram of gold standard determination. A child could be classified gold standard “negative” in several ways: the result was “negative” or “inconclusive” in the orthoptic screening and “negative” in the orthoptic examination: children who had a visual acuity of >0.63 (10/17) in either eye or better and no anomalies in the orthoptic examination were classified gold standard “negative” without further examination; children with “positive” or “inconclusive” or “borderline” results in the orthoptic examination were referred. Children with a “positive” screening were all referred. To be classified gold standard “positive,” a child had to be referred and had to have target conditions upon ophthalmological examination.
Ophthalmological examination
If any orthoptic screening item in phase I was “positive,” the child was referred for a full ophthalmologic examination; likewise, if upon the orthoptic examination (phase II) collaboration was insufficient so that findings were classified “inconclusive” or if the child was absent, the child was also referred to an ophthalmologist. Application of this procedure meant that any visual anomaly detected in kindergarten had to be confirmed by an ophthalmological examination. If the result of an ophthalmological examination was “positive,” then the gold standard was set “positive,” or if the result was “negative,” then the gold standard was set “negative.”
Parents were given the choice to have their child examined in the outpatient clinic of the strabology department of the University Eye Hospital, Tübingen, or in the office of an ophthalmologist in their vicinity to avoid verification bias. About half of the ophthalmological examinations were provided by the strabology department, and the other half by office based ophthalmologists.
To ascertain that parents complied, rigorous follow up contacting, by mail and telephone, was performed systematically and, if necessary, repeatedly within a year after the orthoptic examination of phase II. In addition, ophthalmological examination reports from all children who were currently seen by an ophthalmologist (irrespective of this study) were collected.
A standardised examination report was requested from the ophthalmologist which contained corrected and uncorrected visual acuity, cycloplegic refraction, ocular motility and ocular alignment assessed by cover testing, stereopsis, fundus examination and retinal fixation behaviour, as well as information on treatment, if started.
Criteria for “positive” gold standard
The gold standard classification of the ophthalmological examination records was done by the study team. The study protocol criteria for a “positive” gold standard were:
main criterion: any newly administered spectacle therapy if the corrected visual acuity was ≤0.4 (20/50) in either eye, OR difference of visual acuity between right and left eye >2 logarithmic lines, except for myopia; or
secondary criterion, in the event that the main criterion might not be applicable due to lack of cooperation in the visual acuity testing: any newly administered patching therapy5 in the presence of risk factors like monolateral strabismus or high refractive error (cycloplegic spherical equivalent difference of ≥1.5D, or ≥3D of astigmatism).
It has to be pointed out that the screening criterion for visual acuity line difference was just >1 logarithmic line. This option was chosen to achieve a high sensitivity of screening (that is, not to miss subthreshold borderline cases) and to avoid a definition of target conditions which would include suprathreshold borderline cases.
In cases of spectacle prescription in which visual acuities were above the thresholds defined above, the gold standard was set “negative.”
The study design aimed at performing a community study compatible with current, not necessarily standardised, diagnostic and treatment practice patterns, at bringing about a high participation rate, and avoid verification bias. Therefore no uniform guidelines were imposed upon ophthalmologists. This helped to obtain the participation of all ophthalmologists in the region (see list of more than 30 participating ophthalmologists in the acknowledgements). Parents were not dissuaded from participation in the study because they did not have to present their child to an ophthalmologist who would be complying with guidelines, while their family ophthalmologist might not.
Validity of the gold standard
The gold standard used in this study required all children who screened positive to have a full ophthalmological examination—that is, a “classic” gold standard evaluation, which by definition is 100% accurate, with sensitivity and specificity both being 100%. Hence all children who screened positive were correctly classified; thus no incorrectly “positive” gold standard result could occur, and consequently the specificity of the gold standard was 100%. However, the gold standard did not require all children who screened “negative” to have a full ophthalmological examination. Although a more demanding pass threshold was used in the orthoptic examination in phase II to make incorrectly “negative” gold standard results unlikely, some of those who screened “negative” may have been incorrectly classified as having a “negative” gold standard. Hence, the estimate of sensitivity may be biased. Yet, this bias is likely to be small, as shown in the following paragraph.
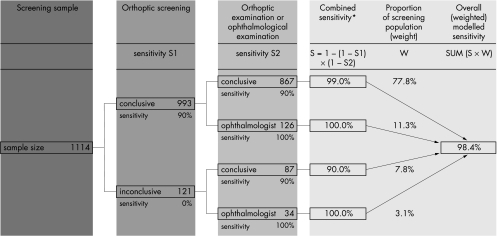
Assuming that the orthoptic screening and the orthoptic examination performed by different orthoptists were independent from each other, the accuracy of the gold standard used in this study can be assessed using conditional probability calculation. Through combining the sensitivities of the orthoptic examinations and those ophthalmological examinations, which were conducted because of “inconclusive” or missing orthoptic examinations in phase II, an overall sensitivity of the gold standard can be computed. Figure 2 shows an example of the calculation of the overall sensitivity of the gold standard used in this study. In this example, the true sensitivities of the orthoptic screening (S1) and the orthoptic examination (S2) were set at 90.0% each, while the number of examinations corresponds to those conducted in the study. The resulting overall sensitivity of the gold standard would be 98.4%, which means that of 100 children diagnosed “positive” through ophthalmological examinations, 1.6 would be misclassified by the gold standard used in this study. With respect to the observed sensitivity of the orthoptic screening, which was calculated based on “conclusive” results of phase I only, the bias would even be smaller. In the example shown in Figure 2, the sensitivity of the gold standard in children with “conclusive” results in phase I would be 99.2%. Hence, if the true sensitivity of the orthoptic screening was 90% as assumed in this example, it would be estimated at 90.0%/99.1% = 90.7%—that is, overestimated by only 0.8% percentage points. Table 1 lists other combinations of sensitivities of orthoptic screening and orthoptic examination. Even for unrealistically low sensitivities of orthoptic examinations, the results were still acceptable to achieve a valid gold standard.
Figure 2.
From the number of orthoptic screenings (phase I), orthoptic examinations (phase II), and ophthalmological examinations the overall test characteristics (sensitivity or specificity) of the gold standard may be assessed using conditional probability calculation. For example, assuming a 90% sensitivity of orthoptic screening, a 90% sensitivity of the orthoptic examination, and a 100% sensitivity of ophthalmological examination, the overall sensitivity of the gold standard would be 98.4%. Likewise, for those 993 children with conclusive results of phase I, the sensitivity of the gold standard would be 99.0% × 867/993 + 100% × 126/993 = 99.1%. (Only those ophthalmological examinations were included which were conducted because of inconclusive or missing orthoptic examinations in phase II; 42 additional ophthalmological examinations, which were conducted although the gold standard was already “negative” based on the orthoptic examinations, were not included. Those 132 ophthalmological examinations conducted as a consequence of “positive” orthoptic screening or orthoptic examinations were not included either.)
Table 1.
Modelled sensitivity of the gold standard computed for a range of parameters
| Sensitivity of orthoptic screening | Sensitivity of orthoptic examination | Modelled sensitivity of gold standard |
| 95.0% | 95.0% | 99.4% |
| 90.0% | 95.0% | 99.2% |
| 90.0% | 90.0% | 98.4% |
| 90.0% | 80.0% | 96.9% |
| 90.0% | 70.0% | 95.3% |
| 90.0% | 60.0% | 93.8% |
| 90.0% | 50.0% | 92.2% |
| 80.0% | 80.0% | 95.3% |
| 80.0% | 50.0% | 88.3% |
Owing to gold standard results incorrectly classified “negative,” the specificity of the orthoptic examination may also be overestimated; however, the magnitude of overestimation would even be smaller than for sensitivity.
RESULTS
Cooperation and attendance in the study population
In phase I, 1047 (88.7%) of all 1180 children showed sufficient cooperation with the orthoptic examination, providing a “conclusive” result (“referral” or “no referral”); 133 (11.3%) children had an “inconclusive” result.
In phase II, 194 (16.4%) of the children examined in phase I were not present in kindergarten on the days of the orthoptic examination, owing to illness, vacation, etc, 957 (97.1%) of the 986 children present were sufficiently cooperative.
Gold standard results
For 1114 children (94.4%), including the 21 children already treated before screening, the gold standard was ascertained as of February 2001. Of those 66 children for whom no gold standard result could be obtained, all had “inconclusive” orthoptic examination results, almost all of them because they did not attend the orthoptic examination in phase II, having mostly “negative,” and to a lesser extent, “inconclusive” findings in the orthoptic screening.
Forty two children were examined by an ophthalmologist although for them the gold standard was already “negative” based on both orthoptic examinations. Some of these children happened to have an ophthalmological examination some time before the kindergarten screening and a few children were presented to an ophthalmologist after the first or second screening because the parents became sensitised. In none of these 42 children was a target disease detected.
“Positive” gold standard results
In 26 children the gold standard was “positive” (26/1, 114=2.3%, 95% CI 1.4% to 3.2%). Of these, three had small angle or accommodative strabismic amblyopia; the rest had refractive/anisometropic amblyopia. Patching and spectacle treatment was started in seven gold standard “positive” children, 19 received glasses only.
Table 2 shows the ophthalmological findings and orthoptic vision screening results (phase I) obtained in the 26 children with a “positive” gold standard. The cycloplegic refractive, ocular alignment, and morphological anomalies found in the ophthalmological examinations suggest that these children were affected by amblyopia or amblyogenic risk factors, which should be treated early in childhood in order to avoid lifelong reduced visual acuity.
Table 2.
Ophthalmological examination findings and orthoptic vision screening results of gold standard “positive” children; all children received spectacle treatment. Refractive errors are those measured under cycloplegia. Subjects 1222, 1221, and 1855 had moderate risk factors, but they nevertheless failed the more important visual acuity testing performed in offices of participating ophthalmologists
| Subject ID | Ocular alignment |
Eye motility/ head posture |
Sphere RE/D |
Cyl RE/D |
Axis RE/° |
Sphere LE/D |
Cyl LE/D |
Axis LE/° |
Funduscopy | Retinal fixation | Patching | Other findings | Orthoptic screening |
| 1363 | small angle strabismus LE | “positive’ | 2 | 0 | 2 | 0 | yes | accommodative strabismus | “positive” | ||||
| 1777 | small angle strabismus RE | 4 | −0.5 | 0 | 3.5 | −0.5 | 6 | no | “positive” | ||||
| 1869 | small angle strabismus RE | “positive” | 5 | 0 | 2.5 | 0 | morning glory optic disc RE | eccentric RE | yes | ptosis RE>LE | “positive” | ||
| 1642 | 6.25 | −3.5 | 0 | 6.25 | −3.5 | 0 | no | “negative” | |||||
| 1347 | 3.75 | −3.5 | 173 | 2.75 | −3.75 | 179 | no | “inconclusive” | |||||
| 264 | 0.75 | −3.25 | 0 | 1.25 | −3.75 | 0 | no | “inconclusive” | |||||
| 1253 | 5 | −2 | 10 | 3 | 0 | no | “positive” | ||||||
| 118 | 1 | −2.5 | 10 | 1 | −3.25 | 170 | unsteady RE and LE | no | “positive” | ||||
| 184 | 3.5 | −0.75 | 155 | 3.5 | −1.5 | 0 | eccentric LE | no | “positive” | ||||
| 1222 | 3 | −1 | 0 | 3 | −0.75 | 10 | no | “positive” | |||||
| 1221 | 1.25 | −0.75 | 18 | 1.25 | −0.75 | 160 | no | “positive” | |||||
| 1292 | 1.75 | −0.75 | 27 | 4.75 | −4 | 5 | no | “positive” | |||||
| 1426 | 6.75 | −2.5 | 2 | 7.5 | −2.5 | 8 | no | “inconclusive” | |||||
| 1626 | 0.5 | −2.75 | 8 | −1.25 | −2.5 | 18 | no | “inconclusive” | |||||
| 1825 | “inconclusive” | 0 | −3.75 | 0 | 0.25 | −3.25 | 0 | no | “positive” | ||||
| 1855 | 2.75 | −1.25 | 58 | 2 | −0.5 | 101 | no | “positive” | |||||
| 1881 | 2.5 | −2 | 15 | 3 | −2.5 | 0 | no | “positive” | |||||
| 1933 | 2 | −2 | 0 | 1.75 | −2 | 0 | no | “positive” | |||||
| 2052 | 8.5 | −0.5 | 95 | 7 | −0.5 | 98 | no | “positive” | |||||
| 2093 | 3.5 | −0.5 | 20 | 6.5 | −1 | 140 | no | “positive” | |||||
| 2149 | 4.75 | −3.75 | 7 | 4.25 | −3.75 | 170 | no | “positive” | |||||
| 110 | 1.5 | −2 | 125 | 1.75 | −1 | 55 | yes | “negative” | |||||
| 1205 | 5.75 | −0.5 | 175 | 7.75 | −1.25 | 95 | yes | “positive” | |||||
| 1667 | 7.25 | −2 | 160 | 2 | 0 | yes | “positive” | ||||||
| 1769 | 2.25 | −0.25 | 160 | 6.5 | −0.25 | 160 | yes | “positive” | |||||
| 2124 | 4 | −0.5 | 20 | 1 | 0 | yes | “positive” |
One may speculate that some of the patching prescribed in the offices of participating ophthalmologists may not have been necessary. However, it was not the purpose of the study to examine the current practice patterns. These patterns were not questioned, they were rather a basis for a study which should reflect the impact of orthoptic kindergarten screening if it were added to existing eye care procedures.
In a further 26 children glasses were prescribed until February 2001 because of subnormal visual acuities and moderate ametropia which did not qualify as amblyogenic according to the study criteria.
Strabismic children
In total, there were 13 children whose strabismus was already known mostly due to a large angle of strabismus, and seven who were newly detected; in two more children there were known ocular motility disorders. One strabismic child treated for amblyopia was not included in the study because the mother refused participation. There were six children with decompensating exophorias without amblyopia of which four were newly detected by the screening. In six strabismic children, the gold standard was “negative”: these were mostly children with intermittent divergent strabismus, and four of these were detected by the screening. In addition, there was one case of nystagmus, who was already known and did not need treatment for amblyopia, and one already known case of Duane’s motility disorder without amblyopia.
Test characteristics of orthoptic vision screening
Table 3 shows the results of the orthoptic screening for those 1114 children for whom the gold standard was obtained and Table 2 links the ophthalmological findings in the 26 gold standard “positive” children with the orthoptic examination results. In 993 of these 1114 children a “conclusive” screening result was obtained in phase I (see Fig 2). Of 26 gold standard “positive” children, there were 22 with “conclusive” results in phase I. Based on the results of the children with “conclusive” results, and without the 18 children among them who were already treated for amblyopia or amblyogenic factors, the sensitivity of the orthoptic vision screening was 90.9% (20/22) and the specificity was 93.8% (894/953). The positive predictive value was 25.3% (20/79), the negative predictive value was 99.8% (894/896).
Table 3.
Results of orthoptic screening (phase I) by test items and cumulated, in 1093 children for whom the gold standard was obtained and who were not treated for amblyopia or amblyogenic risk factors before screening. Inconclusive results of orthoptic screening items were excluded to compute the proportion of gold standard “positive” cases which were detected by each item, and the resulting per item sensitivity and specificity
| Inconclusive results | Positive results | Negative results | ||||||||
| Screening item | No | % | No | % | No | % | No of conclusive results | Proportion of detected gold standard “positive” cases* | Sensitivity | Specificity |
| Inspection | 0 | 0.0 | 2 | 0.2 | 1091 | 99.8 | 1093 | 1/26 | 3.8% | 99.9% |
| Ocular motility/head posture | 47 | 4.3 | 12 | 1.1 | 1034 | 94.6 | 1046 | 3/25 | 12.0% | 99.1% |
| Cover testing | 51 | 4.7 | 13 | 1.2 | 1029 | 94.1 | 1042 | 4/25 | 16.0% | 99.1% |
| Visual acuity | 118 | 10.8 | 63 | 5.8 | 912 | 83.4 | 975 | 19/22 | 86.4% | 95.4% |
| Cumulated | 118 | 10.8 | 79 | 7.2 | 896 | 82.0 | 975 | 20/22 | 90.9% | 93.8% |
*Proportion of detected cases with positive gold standard among all cases with positive gold standard in children with conclusive result for the screening item (equal to sensitivity).
Table 3 illustrates the relative importance of the screening items when “inconclusive” results were excluded to compute the test characteristics of orthoptic vision screening in 3 year old kindergarten children. The most sensitive single test item was visual acuity testing. Two children screened “positive” upon inspection: one child with a “red eye” who was gold standard “negative”, and another child with bilateral ptosis (subject ID 1869, see Table 2) who was gold standard “positive” because of strabismic amblyopia. Therefore, inspection was little helpful for screening in this sample.
DISCUSSION
Study population
Only 3 year olds were included, because these were the youngest children who could be examined in kindergarten in Germany. However, the results are likely to be more favourable in 4 year olds, since these are in general examined more easily. This means that children who enter kindergarten later, and escape screening at age 3, could be screened at age 4.
Two cases of strabismic amblyopia were newly detected in children whose parents erroneously indicated current ophthalmological treatment of their child on the consent form. Therefore, inclusion of children in the screening programme should not be based on the history provided by the parents.
The results of this study suggest that at age 3 most strabismic amblyopias with visible angular deviation have already been detected and that the remaining target conditions are mostly due to refractive errors. Since visual acuity testing—the most important single screening item in detecting refractive errors—depends more on cooperation and age than cover testing does, orthoptic screening in populations with a greater proportion of strabismic amblyopias may be even more sensitive and specific, with less “inconclusive” results.
Choice of screening items
A single optotype test, and without crowding bars, was used because this would make testing of 3 year olds easier: this was backed by the finding in a study which showed that the Lea single optotype test was nearly as sensitive to detect amblyopia as a line test.24,25 Similar findings were obtained when using the Sheridan-Gardiner single optotype test of visual acuity.5 The use of a more difficult test and a higher threshold may have increased the proportion of “inconclusive” or false positive results, without raising the sensitivity. Children with “positive” gold standard who were not detected through screening (phase I) had bilateral balanced refractive errors (see Table 2), and probably a lower risk of severe amblyopia than the unilateral visual deficits of which none escaped the screening.
While there is agreement that line tests exhibit a better sensitivity for amblyopia than single optotype tests, and that crowded optotypes could be even more sensitive when tested in cooperative subjects, screening with such tests in 3 year old children may not necessarily be more advantageous, since their testability and specificity may be inferior. For instance, a study of the testability of Lea symbols (line chart) versus HOTV line charts found that in three year old children the testability was better for Lea symbols (92%) than for HOTV charts (85%).26 The authors concluded that Lea symbols should be preferred over HOTV and tumbling E tests. Yet, in the cited study, two screeners were used for each chart. In the study presented here, using the Lea single symbols book administered by a single screener recruited from outside laboratories and universities, the percentage of untestable 3 year old children was 10.8% (95% CI 9% to 13%) compared to 8% (95% CI 4% to 12%) using Lea line charts in the above cited study,26 which leaves the results fairly comparable at the testability level. However, the intervention of two trained research screeners to perform visual acuity testing would not seem to be a realistic option to conduct screening cost effectively in a real world setting. Another study reported success (testability) rates of 76% (3 year olds) and 95% (4 year olds) with Lea line symbols.27 In the light of the present study’s results these data rather point to a lower testability of line symbol tests in 3 year olds.
The rationale of the present study was to foster feasibility at all levels. Therefore, a most simple, fast and easy to use test, the Lea single symbol book, was preferred over the corresponding line or crowded test.
Gold standard
The study protocol was tailored to assess the test properties of orthoptic kindergarten screening in German kindergartens. A practicable gold standard was used, which did not require all children to undergo a full ophthalmological examination. This made it possible to recruit almost all eligible children in the participation kindergartens. The gold standard was ascertained in more than 94% of the study population, thus avoiding verification bias. The effectiveness of screening was based upon practical treatment decisions. The study design helped avoid laboratory conditions which could not necessarily be reproduced in reality.
The validity of the gold standard in children without pathological findings in the orthoptic examinations may be questioned because an ophthalmological examination was not mandatory to rule out the presence of target conditions. This might entail a reduced sensitivity of the gold standard, and an overestimation of the sensitivity and specificity of orthoptic screening. However, this error, if it exists, would be small, as demonstrated by the decision analytic model.
Prevalence of amblyopia and amblyogenic risk factors compared to other studies. In a recent review28 the prevalence of amblyopia (estimated from the yield of screening programmes) was found to be between 2.7% and 4.4%. The prevalence of amblyopia or amblyogenic risk factors in the present sample was 47/1114 = 4.2% (95% CI 2.1% to 5.4%) which fits into the cited bracket, and would suggest that the sample prevalence was at the upper end of established prevalence limits.
CONCLUSIONS
In this study, orthoptic screening performed in kindergarten was sensitive and specific for detecting amblyopia and amblyogenic risk factors in 3 year old children. However, in approximately 11% of 3 year olds no “conclusive” screening results were obtained because of insufficient cooperation. To increase effectiveness “inconclusive” results could be rated “referral” together with the “positive” screening results, which would also raise the sensitivity to 92.3% (23/26). In turn, the specificity would decrease considerably. This may require rescreening of these children at a later time, when children will be slightly older and adequate cooperation will be more likely as a result of further developed social behaviour. This and other options were analysed in economic evaluations of different vision screening methods in kindergarten,29,30 which demonstrated the impact of test characteristics on the cost effectiveness of screening. While the data show that the screening programme can be conducted effectively, the evaluation of treatment effectiveness was beyond the scope of this study, and remains to be addressed separately.
Acknowledgments
Faculty grant UKT fortüne 447. Supported by grants and donations from: E and B Grimmke Foundation, Düsseldorf, Carl Zeiss, Aalen; Trusetal Verbandstoffwerk, Schloss Holte-Stukenbrock; Hewlett-Packard GmbH, Sindelfingen; W Vaillant Foundation, Munich.
Commercial relationship disclosure: None (all).
The authors gratefully acknowledge the contributions of the following collaborators and institutions: (A) Orthoptic examinations; kindergarten staff and administration of the participating institutions; Reutlingen and Tübingen Municipal and County Public Health Services. Contract orthoptists: I Bleher, G Wenzel, E Joos-Kratsch, U Haerten-Margulies, A Laaff, I Jäger-Leininger, U Baedorf; Organising team: B Hartmann, G Kempter, J Eisert; (B) Ophthalmological examinations: staff of the department for eye motility disorders: Orthoptists: B Nüssle, D Müller, B Rapp, E Oechsner; Physicians: V Herzau, H Hettesheimer, K Siepmann; Office based ophthalmologists (mostly from the Tübingen and Reutlingen regions) for providing their examination records: T Adis, A Riester, F Lorch, A Stanowsky, L Flögel, W Dechant, E Bader, I Hirsch, S Boddin, E Ellinger, K König, B Kreutzer, KP Krug, D Lemke, M Reichel, N Wenzel, H Engelke, A Fries-Woye, A Sperber, M Sperber-Szymankiewicz, R Mittelstaedt, C Pohl, I Schuster, D Seuffer-Schulze, G Stehberger, R Zevallos-Möll, B Ohmer, M Heimann, H Karcher, B Kampeter U Seidel, U Veith, E Mueller, E Hirnle, S Meilinger-Krebs, T Wolf, B Hoyer, H Maier.
REFERENCES
- 1.Sjöstrand J, Abrahamsson M. Prevention of amblyopia and the concept of cure. Eur J Ophthalmol 1997;7:121–9. [DOI] [PubMed] [Google Scholar]
- 2.Lennerstrand G, Jakobsson P, Kvarnström G. Screening for ocular dysfunction. Acta Ophthalmol Scand 1995;73(Suppl 214):26–38. [DOI] [PubMed] [Google Scholar]
- 3.Fulton AB, Mayer DL. Esotropic children with amblyopia: effects of patching on acuity. Graefes Arch Clin Exp Ophthalmol 1988;226:309–12. [DOI] [PubMed] [Google Scholar]
- 4.Egan DF, Brown R. Vision testing of young children in the age range of 18 months to 4½12 years. Child Care Health Dev 1984;10:381–90. [DOI] [PubMed] [Google Scholar]
- 5.Newman DK, East M. Preschool vision screening: negative predictive value for amblyopia. Br J Ophthalmol 1999;83:676–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics Committee on Practice and Ambulatory Medicine. Vision screening and eye examination in children. Pediatrics 1986;77:918–19. [PubMed] [Google Scholar]
- 7.Bode CP, v Kries R, Gröning A, et al. Welchen Beitrag zur Auffindung von Sehstörungen leistet die Früherkennungsuntersuchung U7. Monatsschr Kinderheilkd 1994;142:901–4. [Google Scholar]
- 8.Hohmann A, Rüssmann W, Kaszli FA. Qualität des Sehscreenings im Kindesalter. Klin Monatsbl Augenheilkd 1997;211:41–7. [DOI] [PubMed] [Google Scholar]
- 9.Allhoff P, Bachmann KD, Flatten G, et al. Beraterkreis “Krankheitsfrüherkennung im Kindesalter” des Zentralinstituts für die kassenärztliche Versorgung: Hinweise zur Durchführung der Früherkennungsuntersuchungen im Kindesalter. Köln: Dt Ärzte Verlag, 1991.
- 10.Jarvis SN, Tamhne RC, Thompson L, et al. Preschool vision screening. Arch Dis Child 1990;65:288–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bolger PG, Stewart-Brown SL, Newcombe E, et al. Vision screening in preschool children: comparison of orthoptists and clinical medical officers as primary screeners. BMJ 1991;303:1291–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wormald RPL. Preschool vision screening in Cornwall: performance indicators of community orthoptists. Arch Dis Child 1991;66:917–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beardsell R. Orthoptic visual screening at 3.5 years by Huntingdon Health Authority. Br. Orthopt. J 1989;46:7–13. [Google Scholar]
- 14.Fathy VC, BSc, Elton PJ, MFCM. Orthoptic screening for three- and four-year-olds. Public Health 1993;107:19–23. [DOI] [PubMed] [Google Scholar]
- 15.Bundesamt S. Statistisches Bundesamt. Statistisches Jahrbuch 2000 für die Bundesrepublik Deutschland. Stuttgart: Metzler-Poeschel, 2000.
- 16.Käsmann-Kellner B, Ruprecht KW. Vision screening survey of all children starting primary school in 1998 in the Federal State of Saarland, Germany. Strabismus 2000;8:201–7. [PubMed] [Google Scholar]
- 17.Schröpfer HD, Meinert K. 15 Jahre Schielprophylaxe in den Kindergärten des Kreises Zittau. Folia Ophthalmol 1986;11:61–3. [Google Scholar]
- 18.Schütte E, Groten H, Leymann J, et al. Augenärztliche Reihenuntersuchungen im Kindergarten. Klin Monatsbl Augenheilkd 1976;168:584–90. [PubMed] [Google Scholar]
- 19.Ransohoff DF, Feinstein AR. Problems of spectrum and bias in evaluating the efficacy of diagnostic tests. N Engl J Med 1978;299:926–30. [DOI] [PubMed] [Google Scholar]
- 20.Harper R, Reeves B. Compliance with methodological standards when evaluating ophthalmic diagnostic tests. Invest Ophthalmol Vis Sci 1999;40:1650–7. [PubMed] [Google Scholar]
- 21.Bates AS, Margolis PA, Evans AT. Verification bias in pediatric studies evaluating diagnostic tests. J Pediatr 1993;122:585–90. [DOI] [PubMed] [Google Scholar]
- 22.Choi B. Sensitivity and specificity of a single diagnostic test in the presence of work-up bias. J Clin Epidemiol 1992;45:581–6. [DOI] [PubMed] [Google Scholar]
- 23.Hartmann EE, Dobson V, Hainline L, et al. Preschool vision screening: summary of a task force report. Pediatrics 2000;106:1105–12.11061783 [Google Scholar]
- 24.Gräf M, Becker R. Sehschärfenbestimmung mit LH Symbolen und Landoltringen. Klin Monatsbl Augenheilkd 1999;215:86–90. [DOI] [PubMed] [Google Scholar]
- 25.Gräf MH, Becker R, Kaufmann H. Lea symbols: visual acuity assessment and detection of amblyopia. Graefes Arch Clin Exp Ophthalmol 2000;238:53–8. [DOI] [PubMed] [Google Scholar]
- 26.Hered RW, Murphy S, Clancy M. Comparison of the HOTV and Lea symbols chart for preschool vision screening. J Pediatr Opthalmol Strabimus 1997;34:24–8. [DOI] [PubMed] [Google Scholar]
- 27.Becker R, Hübsch S, Gräf M, et al. Examination of young children with Lea symbols. Br J Ophthalmol 2002;86:489–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Snowdon SK, Stewart-Brown SL. Preschool vision screening. Health Technol Assess 1997;1(8). [PubMed]
- 29.König HH, Barry JC, Leidl R, et al. Economic evaluation of orthoptic vision screening: results of a field study in 121 German kindergartens. Invest Ophthalmol Vis Sci 2002;43:3209–15. [PubMed] [Google Scholar]
- 30.König HH, Barry JC. Economic evaluation of different methods of screening for amblyopia in kindergarten. Pediatrics 2002;109 :http://www.pediatrics.org/cgi/content/full/109/4/e59. [DOI] [PubMed]