Myasthenia gravis has been reported to be associated with both ulcerative colitis (UC) and Crohn’s disease (CD).1–3 The link between inflammatory bowel disease (IBD) and myasthenia gravis (MG) is thought to be related to the production of autoantibodies.1 Myasthenia gravis is also associated with other autoimmune diseases including alopecia, lichen planus, vitiligo, and systemic lupus erythematosus.4
Similarly, IBD frequently presents with other autoimmune disorders. One study demonstrated a 9.4% prevalence of autoimmune disorders in patients with UC including sclerosing cholangitis, thyroid disorders, vitiligo, insulin dependent diabetes mellitus, thyroid disease, pernicious anaemia, scleroderma, and seropositive rheumatoid arthritis.4,5 Despite the association between MG and other autoimmune disorders, there are relatively few reports of ocular findings as the presenting sign of MG in patients with IBD.
Case report
A 21 year old African-American male, with a medical history of biopsy proved ulcerative colitis diagnosed in 1995, focal segmental glomerular sclerosis determined by renal biopsy in 1995, and primary sclerosing cholangitis determined by liver biopsy in 2000 presented to the neuro-ophthalmology service with complaints of binocular diplopia and ptosis of the left upper eyelid. Both the diplopia and the ptosis were better in the morning and worsened during the course of the day. His ulcerative colitis had been in remission for the past 5 years without medication.
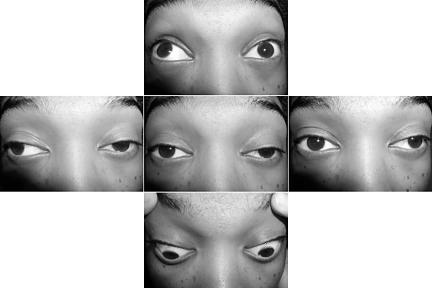
Best corrected visual acuity was 20/25 in each eye. The external examination revealed ptosis of the left upper eyelid that worsened in sustained upgaze. He had limited extraocular motility in all fields of gaze (Fig 1). The remainder of the neuro-ophthalmic examination was normal and he had no difficulty with speech or swallowing.
Figure 1.
External photograph shows ptosis of the left upper eyelid, restriction of all extraocular movements of the left eye, and an elevation and adduction deficit of the right eye.
Laboratory evaluation revealed a positive acetylcholine receptor antibody and normal thyroid function studies. There was no evidence of a thymic mass on magnetic resonance imaging of the chest.
The patient returned to the emergency room 1 week later with difficulty swallowing and shortness of breath. He was hospitalised for plasmapheresis and upon discharge treated with imuran, prednisone, and mestinon. One month later his ptosis resolved and his extraocular motility was normal.
Comment
Autoimmune disorders, including MG, occur more frequently in UC than in CD.3 It is not clear how many other cases of IBD manifested with ocular presentations as the initial finding of MG as in our case report. Our literature review revealed only one other purely ocular presentation of myasthenia associated with ulcerative colitis; however, details of the ocular examination were not included.5 Another report, of a 21 year old woman with a 3 year history of Crohn’s disease, documented diplopia and unilateral ptosis as the initial findings of MG.3 She was found to have acetylcholine receptor antibodies and her ocular findings improved with pyridostigmine.
Because of the relatively few reports of ocular myasthenia in patients with IBD we reviewed the English literature and found four additional reports of MG in patients with IBD. Based on these four reports and the three (including the present report) with ocular MG in patients with IBD (Table 1), the mean duration of IBD before the diagnosis of MG was 10 years.
Table 1.
Previous reports of myasthenia gravis occurring in patients with inflammatory bowel disease
| Reference | Age (years) | Sex | IBD | Duration of IBD before diagnosis of MG (years) | AchR antibody reactivity |
| Miller 19715 | 35 | Male | UC | 13 | Unknown |
| Tan 19744 | 38 | Male | UC | 12 | Unknown |
| Martin et al, 19911 | 63 | Male | CD | 15 | Positive |
| Gower-Rousseau et al, 19938 | 27 | Female | UC | 10 | Positive |
| Finnie et al, 19943 | 21 | Female | CD | 3 | Positive |
| Lossos et al, 19959 | 11 | Male | CD | 9 | Unknown |
| Present report | 21 | Male | UC | 7 | Positive |
IBD = inflammatory bowel disease, MG = myasthenia gravis, AchR = acetylcholine receptor, UC = ulcerative colitis, CD = Crohn’s disease.
Autoimmune dysregulation is the central defect in both MG and IBD. Both IBD and MG may be associated with an elevated carcinoembryonic antigen (CEA) and decreased peripheral lymphocyte counts that subsequently normalise following thymectomy.6 Some studies have shown abnormal thymic involution and the presence of an abnormal ratio of T suppressor to T helper cells in both MG and UC, while others have noted a decline in suppressor T cells and an increase in immature helper T cells suggesting migration without normal maturation.2,7
The immunological link between MG and IBD is highlighted by two reports of patients undergoing surgical treatment. One report of a patient with both MG and CD documented improvement in perineal and perianal disease following thymectomy for severe uncontrolled MG.3 Another patient with both MG and UC demonstrated regression of the myasthenia following proctolectomy.8
Although the simultaneous occurrence of these two autoimmune disorders is uncommon, it is important to understand that ocular findings may be the initial manifestation of MG in patients with IBD.
The authors have no proprietary interest in any contents of this manuscript
References
- 1.Martin RW, Shah A. Myasthenia gravis coexistent with Crohn’s disease. J Clin Gasteroenterol 1991;13:112–13. [PubMed] [Google Scholar]
- 2.Souadijian JV, Enriquez P, Silverstein MN, et al. The spectrum of disease associated with thymoma. Coincidence or syndrome? Arch Intern Med 1974;134:374–9. [PubMed] [Google Scholar]
- 3.Finnie IA, Shields R, Sutton R, et al. Crohn’s disease and myasthenia gravis: a possible role for thymectomy. Gut 1994;35:278–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tan RS. Ulcerative colitis, myasthenia gravis, atypical lichen planus, alopecia areata, vitiligo. Proc R Soc Med 1974;67:195–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Miller TN. Myasthenia gravis, ulcerative colitis and lichen planus. Proc R Soc Med 1971;64:806. [PMC free article] [PubMed] [Google Scholar]
- 6.Papatestas AE, Kim U, Genkins G, et al. The association of carcinoembryonic antigen and peripheral lymphocytes. Surgery 1974;78:343–48. [PubMed] [Google Scholar]
- 7.Aiso S, Yoshida T, Watanabe M, et al. Characterization of thymus cells in hyperplastic thymuses in patients with myasthenia gravis and ulcerative colitis with monoclonal antibodies. J Clin Lab Immunol 1984;13:137–9. [PubMed] [Google Scholar]
- 8.Gower-Rousseau C, Reumaux D, Bellard M, et al. Remission of myasthenia gravis after proctolectomy in a patient with ulcerative colitis. Am J Gastroenterol 1993;88:1136–8. [PubMed] [Google Scholar]
- 9.Lossos A, River Y, Eliakim A, et al. Neurologic aspects of inflammatory bowel disease. Neurology 1995;45(Pt 1):416–21. [DOI] [PubMed] [Google Scholar]