No proved treatment exists for ischaemic macular oedema associated with branch retinal vein occlusion (BRVO) despite the potential for significant visual loss in affected eyes.
We report a patient with an ischaemic BRVO with associated macular oedema treated with intravitreal triamcinolone acetonide.
Case report
A 38 year old man was referred to our department with a 6 week history of acute visual loss in his right eye (RE). On examination, visual acuity was 6/60 RE and 6/6 LE. A right relative afferent pupillary defect was present. Intraocular pressures were 9 and 10 mm Hg, respectively. Anterior segment examination showed no evidence of neovascularisation. There was no vitreous inflammation. Dilated fundus examination revealed a right inferotemporal BRVO with macular oedema. Collateral disc vessels were present. Systemic and haematological examinations, including full blood count, erythrocyte sedimentation rate, C-reactive protein, clotting screen, serum angiotensin converting enzyme, serum cholesterol and triglycerides, clotting screen, chest x ray, and ECG, were negative for systemic vascular or vasculitic disease.
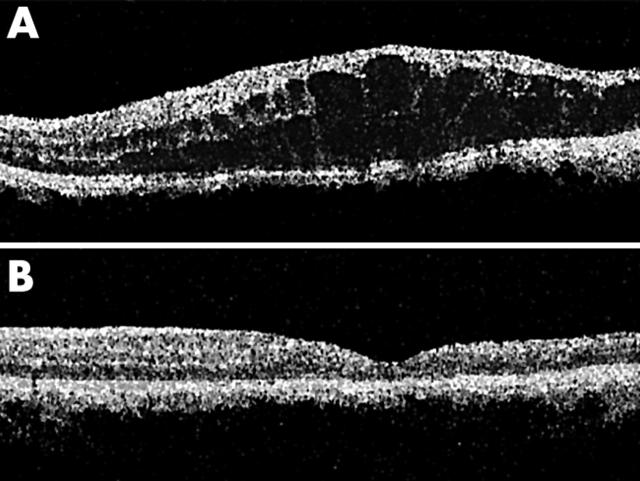
At review 4 months later, right visual acuity had reduced to counting fingers. Fluorescein angiography showed significant macular ischaemia and non-perfusion with a broken foveal capillary ring (fig 1A). There was diffuse leakage and additional masking from intraretinal haemorrhages (fig 1B). Optical coherence tomography measured a central macular thickness of 337 μm in the right eye (fig 2A). Owing to the poor visual outcome in the RE with observation, and the presence of macular ischaemia precluding argon laser grid treatment, the patient was offered an intravitreal injection of triamcinolone acetonide (Kenalog, Bristol-Myers Squibb, UK). Topical 0.5% amethocaine was used for anaesthesia. Povidone-iodine 5% was then applied to the conjunctiva. Triamcinolone, 4 mg (0.1 ml), was injected through the inferior pars plana, 4 mm from the limbus.
Figure 1.
(A) Transit phase of the fluorescein angiogram of the right eye demonstrates an inferotemporal branch retinal vein occlusion with capillary non-perfusion and a broken foveal ring. (B) Late phase fluorescein angiogram showing macular oedema.
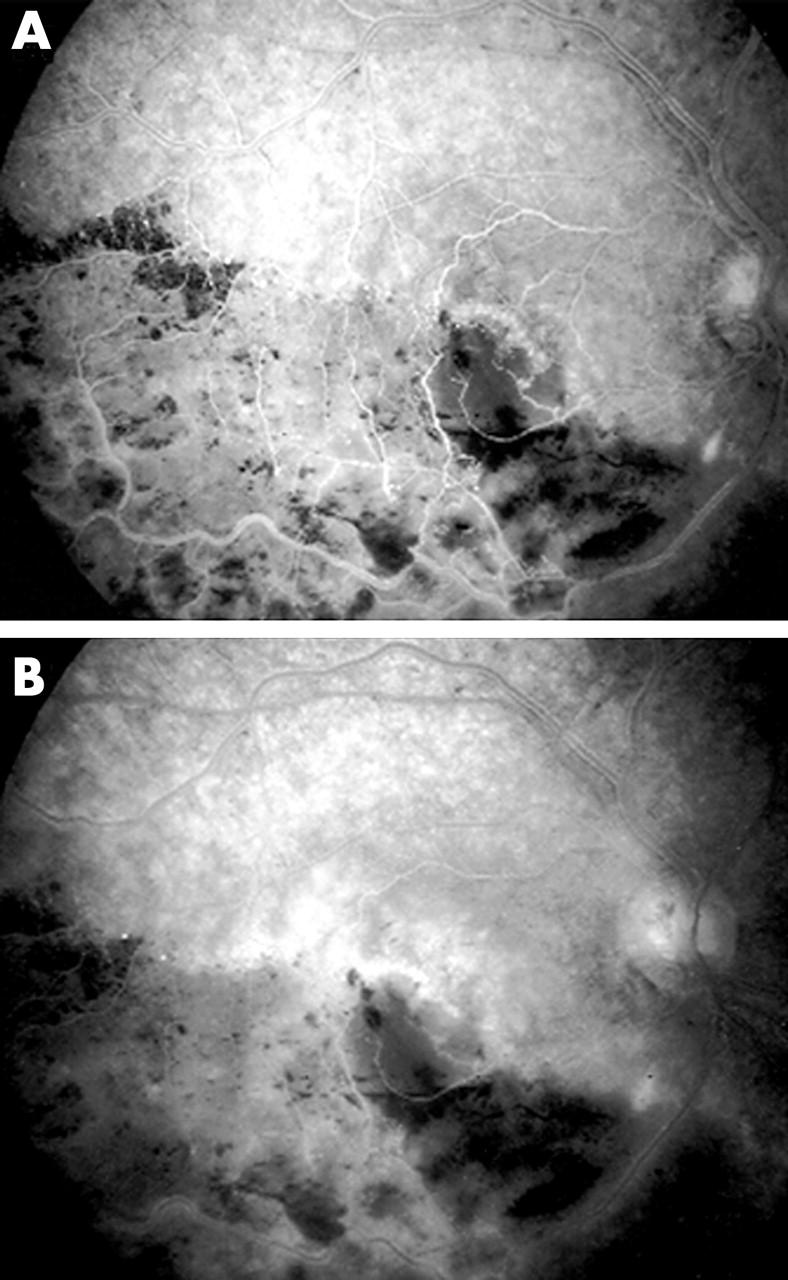
Figure 2.
(A) Optical coherence tomography of the left eye before first intravitreal triamcinolone injection demonstrating marked macular oedema with intraretinal cysts. (B) Resolution of macular oedema with restoration of normal foveal contour 2 weeks after intravitreal triamcinolone injection.
Two weeks post-injection, visual acuity had improved to 6/36 in the right eye On biomicroscopic examination the macula oedema had resolved fully. Central macular thickness measured 160 μm with a normal foveal contour (fig 2B).
Visual acuity at 3 months post-injection was 6/24 with no macular oedema detectable on biomicroscopic examination.
Comment
Macular oedema caused by BRVO carries a variable visual prognosis. After 3 years, 23% of untreated eyes will have visual acuity 20/200 or worse. Only 37% of eyes will gain two or more lines of visual acuity. The Branch Vein Occlusion Study group showed that argon laser grid photocoagulation can improve visual acuity in eyes with BRVO with macular oedema reducing vision to 20/40 or worse.1
However, laser treatment is inappropriate in eyes with foveal capillary non-perfusion. Eyes with BRVO and a broken foveal capillary ring have a poorer prognosis for visual acuity.2 Although one study reported a favourable visual outcome in 91% of eyes with BRVO and macular oedema associated with incomplete macular perfusion,3 the majority of cases with a good visual outcome presented with visual acuities of 20/100 or better. Poor presenting visual acuity is correlated to poor visual prognosis.4
In this case, a patient with a chronic BRVO and ischaemic macular oedema had complete resolution of the macular oedema 2 weeks following intravitreal injection of triamcinolone. The resolution of macular oedema was associated with a significant improvement in visual acuity from counting fingers to 6/24. This final visual acuity was presumably limited because of residual ischaemic macular damage.
Although the mode of action by which triamcinolone induces resolution of macular oedema remains poorly understood, in vitro studies and clinical observations indicate that triamcinolone has the capacity to reduce the permeability of the outer blood-retinal barrier.5
Intravitreal triamcinolone has been shown to be safe and effective when used for the treatment of cystoid macular oedema caused by uveitis,6 diabetic maculopathy,7 central retinal vein occlusion,8 and post-cataract surgery.9 IOP elevation may occur in up to 50% of eyes after triamcinolone injection.10 Other potential risks include cataract development, retinal detachment, and endophthalmitis. Despite good initial anatomical and visual response to intravitreal triamcinolone when used in these conditions, macular oedema has been reported to recur following treatment, often necessitating repeated injections. Further follow up is required to determine if macular oedema recurs following treatment in branch retinal vein occlusions.
This case suggests that the use of intravitreal triamcinolone acetonide for the treatment of macular oedema due to BRVO warrants further study.
References
- 1.The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol 1984;98:271–82. [DOI] [PubMed] [Google Scholar]
- 2.Shilling JS, Jones CA. Retinal branch vein occlusion: a study of argon laser photocoagulation in the treatment of macular oedema. Br J Ophthalmol 1984;68:196–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finkelstein D. Ischemic macular edema. Recognition and favorable natural history in branch vein occlusion. Arch Ophthalmol 1992;110:1427–34. [DOI] [PubMed] [Google Scholar]
- 4.Glacet-Bernard A, Coscas G, Chabanel A, et al. Prognostic factors for retinal vein occlusion: prospective study of 175 cases. Ophthalmology 1996;103:551–60. [DOI] [PubMed] [Google Scholar]
- 5.Penfold PL, Wen L, Madigan MC, et al. Triamcinolone acetonide modulates permeability and intercellular adhesion molecule-1 (ICAM-1) expression of the ECV304 cell line: implications for macular degeneration. Clin Exp Immunol 2000;121:458–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Young S, Larkin G, Branley M, et al. Safety and efficacy of intravitreal triamcinolone for cystoid macular oedema in uveitis. Clin Exp Ophthalmol 2001;29:2–6. [DOI] [PubMed] [Google Scholar]
- 7.Martidis A, Duker JS, Greenberg PB, et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology 2002;109:920–7. [DOI] [PubMed] [Google Scholar]
- 8.Greenberg PB, Martidis A, Rogers AH, et al. Intravitreal triamcinolone acetonide for macular oedema due to central retinal vein occlusion. Br J Ophthalmol 2002;86:247–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conway MD, Canakis C, Livir-Rallatos C, et al. Intravitreal triamcinolone acetonide for refractory chronic pseudophakic cystoid macular edema. J Cataract Refract Surg 2003;29:27–33. [DOI] [PubMed] [Google Scholar]
- 10.Jonas JB, Kreissig I, Degenring R. Intraocular pressure after intravitreal injection of triamcinolone acetonide. Br J Ophthalmol 2003;87:24–7. [DOI] [PMC free article] [PubMed] [Google Scholar]