Abstract
Background/aims: B-scan ultrasonography is an invaluable, versatile, non-invasive tool in ophthalmology. Recently, a “high frequency” contact 20 MHz probe has been introduced. B-scanning ultrasonography of orbital and ocular structures was performed with both a 10 MHz and the new 20 MHz probe, to evaluate what information was best obtained from each probe, and provide recommendations for the use of each.
Methods: Patients were selected from routine ultrasound clinics at Aberdeen Royal Infirmary between 1 January 2002 and 1 August 2002. The vitreous, retina, choroid, sclera and, in the orbit, the extraocular muscles, optic nerve, and orbital fat were assessed with both the 10 MHz and 20 MHz probes. In the laboratory, using a “point target,” the characteristics of the ultrasound beam at different distances from the probe were also assessed.
Results: The point target showed that focus was deeper and that the lateral, and to a lesser degree the axial, resolution are sharper with the 20 MHz probe, compared with the 10 MHz probe. In patients’ eyes, highly reflective structures are seen at higher resolution with the 20 MHz probe. Imaging of lower intensity reflectors such as the vitreous and particles within it are seen better with the 10 MHz probe. Increased tissue attenuation was evident with the 20 MHz probe.
Conclusion: The 20 MHz probe has a superior resolution and can be used to better detect details at the posterior pole and in the orbit. The 10 MHz probe can be used to examine low intensity scatterers, such as the vitreous humour, that cannot be seen using a higher frequency probe.
Keywords: B-scan, echography, high frequency ultrasound, ophthalmic ultrasound
The application of B-scan ultrasound in ophthalmology was first described by Baum and Greenwood,1 using an immersion technique. In 1972 Bronson and Turner2 developed a contact technique, making the examination easier and more acceptable to patients. Since then, increased experience and improvement in equipment has seen the B-scan develop into a powerful imaging tool in ophthalmic practice. The advantages of B-scanning over other imaging methods are safety, accessibility, and the ability to perform “real time” kinetic examination.
Using eye dedicated B-scanners and appropriate examination techniques the vitreous, chorioretinal layer and sclera can accurately be assessed,3,4 and, in the orbit, extraocular muscles, optic nerves, vascular and mass lesions can be visualised particularly in the anterior orbital compartment.5–7
The recent technological advances in ultrasound, particularly with the advent of high frequency transducers, have further increased the scope of use, and provided additional clinical applications in ophthalmology and other disciplines such as dermatology,8 cardiology,9 urology,10 and gastroenterology.11
Up until recently, most ophthalmic B-scans have employed frequency of 5–10 MHz. We have performed B-scan ultrasonography using 10 MHz and a new 20 MHz probe and evaluated their advantages and disadvantages. We compared images and ascertained what echographic information was best obtained from each probe both for ocular and orbital structures, and we provide recommendations for their use.
METHODS
We used the Alcon “Ultrascan” (Alcon Inc) B-scan, with a 10 MHz probe, and a newly developed 20 MHz probe. All settings and examination methods except the decibel (dB) gain were identical when comparing 10 and 20 MHz images. The dB gain was adjusted when using each probe to give the optimal images of the ocular or orbital structure of interest. Hard copies of the echograms were obtained using a Mitsubishi P90 printer, with identical printer settings for the 10 and 20 MHz probe. Patients were selected from routine ultrasound clinics at Aberdeen Royal Infirmary between 1 January 2002 and 1 August 2002.
B-scans were performed with the patients placed supine on a reclining chair. Viscotears was used as a coupling gel and all scans were performed with the probe placed directly on the sclera. We assessed the quality of images obtained using each probe with particular reference to the following structures; vitreous, retina, choroid, sclera, orbit, extraocular muscles, and optic nerves.
We also assessed in vitro the ultrasound beam profiles at different distances from the probe. Using a “point target,” which consisted of the end of a nylon filament of 0.3 mm diameter in a water bath, we compared the resultant images obtained from the 10 MHz and 20 MHz probe of the nylon filament at distances of 10–24 mm from the probes. The nylon filament was used as it produces an echo strength similar to that obtained from the eye. The resultant images effectively show the “point spread function” of the probes at these distances, allowing the lateral and axial resolution of the 10 MHz and 20 MHz probes to be compared.
RESULTS
In vitro comparison of 10 and 20 MHz probes
Figures 1A and B show the backscatter pattern of the end of the nylon filament at various distances from the 10 and 20 MHz probes (these are composite images of several individual ones). They, in conjunction with the schematic in figure 1C, illustrate various features of the ultrasound beam from each probe. Firstly, the absence of beam formation until a certain distance, 12 mm for the 10 MHz probe and 16 mm for the 20 MHz probe, is apparent. Secondly, shortly beyond this distance the central main lobe is at its most intense (“focused”), and then diverges the further away the filament is from the probe. Thirdly, side lobes surround the main lobe and separate as the distance between the filament and the probe is increased.
Figure 1.
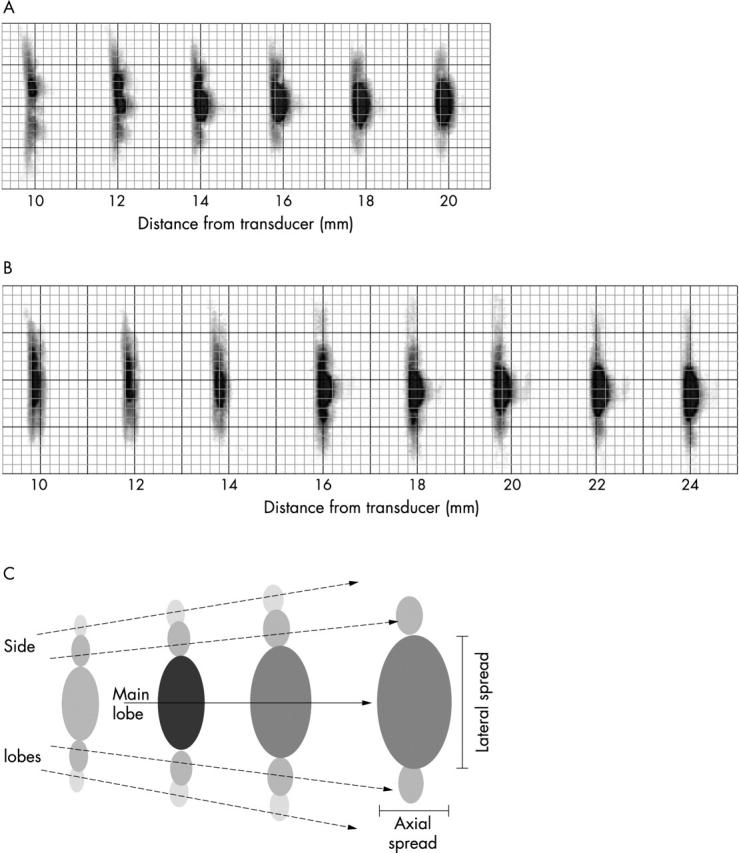
Point spread function of (A) the 10 MHz probe (B) the 20 MHz probe. (C) Schematic of point spread function showing strong main lobe with axial and lateral spread, and weaker, diverging side lobes.
The lateral spread and, to a lesser degree, axial spread of the central lobe of point target echoes is less with the 20 MHz probe, compared with the 10 MHz probe. The difference in lateral spread is most marked at 16 mm, where it is about 1.5 times narrower for the 20 MHz probe than for the 10 MHz probe.
The deeper and sharper 20 MHz focus shows the probe designer exploiting this potential of a high frequency probe, in order to combat the greater propagation loss and to achieve good resolution at the posterior pole of the eye.
A gain setting of 68 dB with the 20 MHz probe was found to give a similar display strength to that of the 10 MHz probe with a gain of 60 dB. This shows that the 20 MHz probe is less sensitive than the 10 MHz probe.
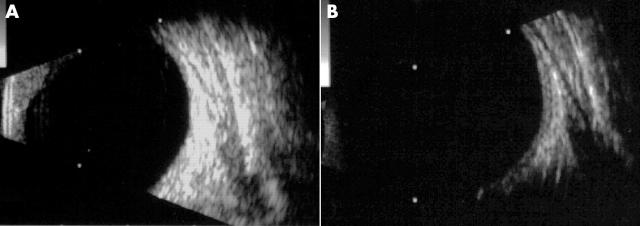
Clinical comparison of the 10 and 20 MHz probes for ocular images
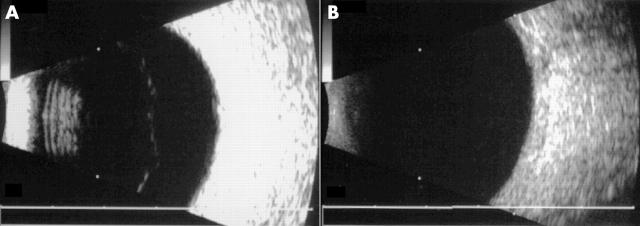
Figures 2 and 3 show images of a posterior vitreous detachment and a mild vitreous haemorrhage, respectively, obtained from the 10 and 20 MHz probes. The 10 MHz probe clearly shows the posterior hyaloid face in figure 2A and posterior hyaloid face, intragel, and posterior hyaloid haemorrhage in figure 3A. In contrast, the 20 MHz probe is unable to demonstrate the posterior hyaloid face in figure 2B, and only just shows the anterior portion of the posterior hyaloid face in figure 3B. With the 20 MHz probe the vitreous haemorrhage is only just visible at in figure 3B. For both these patients the gain was set to maximum (80 dB) for both probes. The 20 MHz probe is clearly not sensitive enough to detect weakly echoing vitreous structures.
Figure 2.
Posterior vitreous detachment scanned with (A) 10 MHz probe (gain 80 dB) and (B) 20 MHz probe (gain 80 dB).
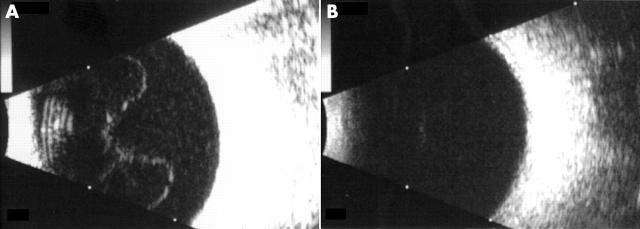
Figure 3.
Vitreous haemorrhage scanned with (A) 10 MHz probe (gain 80 dB) and (B) 20 MHz probe (gain 80 dB).
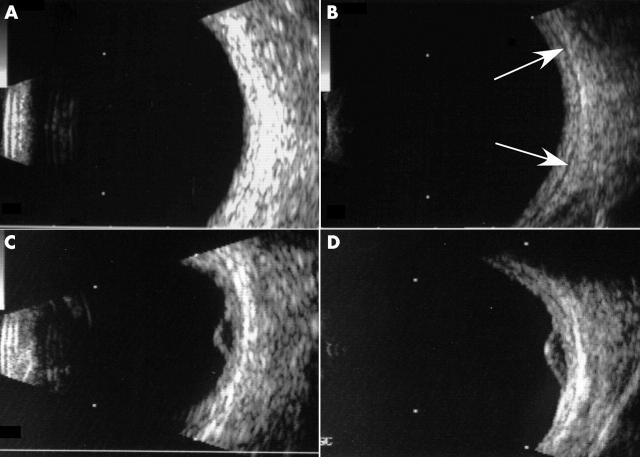
Figures 4A and B show imaging of the globe wall and the “episcleral space.” The episcleral space separates the globe wall from the orbit, and is seen as a thin dark line. It is often used as a reference point for measuring the height of chorioretinal lesions such as choroidal melanoma (figs 4C and D), and is enlarged in scleritis. This, therefore, is an important landmark and is used often by us to determine the sensitivity of B-scanners and their suitability for ophthalmic use. The definition of the episcleral space and choroidal melanomas is better with the 20 MHz probe than with the 10 MHz probe.
Figure 4.
Globe wall scanned with (A) 10 MHz probe (gain 68 dB) and (B) 20 MHz probe (gain 62 dB) in which “episcleral space” is better defined (arrows). Choroidal melanoma scanned with (C) 10 MHz probe (gain 64 dB) and (D) 20 MHz probe (gain 63 dB).
Clinical comparison of the 10 and 20 MHz probes for orbital images
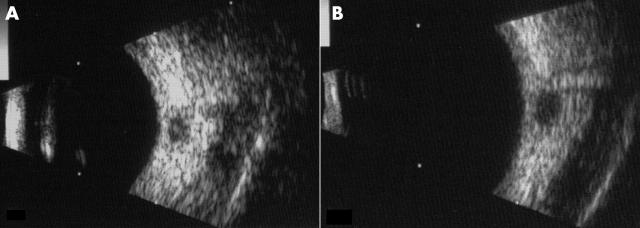
Figures 5 and 6 compare images of orbital structures. Figures 5A and B show the optic nerve, and figures 6A and B show a rectus muscle. There is a clear difference in resolution, with the 20 MHz probe able to resolve the respective orbital structure better. The increased resolution of the 20 MHz probe allows better definition of the low reflective optic nerve proper and muscle fibres from their respective high reflective sheaths. The images from the 10 MHz probe do not provide as good definition as the 20 MHz probe, and suffer from saturation of the image. The orbit is normally very bright from highly reflective fat, therefore the 20 MHz probe, which is less sensitive than the 10 MHz probe, provides images that are less susceptible to image saturation, which when taken with the better resolution of the probe gives a better imaging of orbital structures.
Figure 5.
Optic nerve scanned with (A) 10 MHz probe (gain 61 dB) and (B) 20 MHz probe (gain 69 dB).
Figure 6.
Extraocular muscle scanned with (A) 10 MHz probe (gain 67 dB) and (B) 20 MHz probe (gain 67 dB).
DISCUSSION
B-scan ultrasonography is an invaluable, versatile, non-invasive imaging tool in ophthalmology, and in experienced hands can be used to diagnose and monitor a wide variety of ocular and orbital diseases. Recent developments in the technology have allowed a steady increase in the resolution of images obtainable. Most recently, a 20 MHz probe has been introduced which does not require immersion, and is compact and easy to use. We have been using and evaluating the Alcon 20 MHz probe versus 10 MHz probe in our department for the past year.
The advantages of increasing the frequency of the ultrasound probe is that there should be a proportional increase in the resolution—that is, the resolution of the 20 MHz probe should be twice as good as that achieved by the 10 MHz probe (other parameters being equal). From our in vitro work with the point target, the improvement is about 1½ times. This allows the orbital and intraocular structures to be seen more clearly. Unfortunately, as the frequency of ultrasound increases, the attenuation by tissue also increases. Nevertheless, attenuation by the aqueous and vitreous humour is low even at 20 MHz, so the posterior segment of the eye and orbit can be seen. However, the penetration into the orbit is expected to be less than can be achieved with a lower frequency probe.
The 10 MHz probe is more “sensitive” and has a closer focal distance, so that lower intensity reflectors, such as weakly reflective particles—for example, blood in the vitreous humour, can be detected. This occurs at the expense of imaging at the posterior pole. When the vitreous humour can be visualised, the echoes received from the posterior pole are so strong that the image will be saturated.
If the gain for the 10 MHz probe is decreased, allowing structures at the posterior pole to be distinguished, it can be seen that the resolution is poorer than that of the 20 MHz probe (figs 4A, 4C, 5A, 6A)
Our results confirm that highly reflective structures at the back of the eye such as chorioretina, sclera, optic nerve sheaths, and extraocular muscles sheaths are seen at higher resolution with the 20 MHz probe. This allows better imaging of chorioretinal lesions such as melanoma and naevi, with the measurements of the height of such lesions being more reproducible because of a more accurate reference to the “episcleral space.” However, identification of normal retina and choroid as a separate layer remains difficult, even at 20 MHz frequency, hence our reference to these structures as the “chorioretinal layer.” Optic nerve and extraocular muscle imaging is also better at 20 MHz frequency with more subtle deviations from the normal being detectable. Imaging of lower intensity reflectors such as the vitreous and particles within the vitreous is seen to be quite poor with the 20 MHz probe, but with the 10 MHz probe these low reflectivity structures are readily seen.
It has always been the authors’ practice to scan through the open eye, directly on the sclera and avoid scanning through the lens in order to prevent or minimise tissue attenuation. This attenuation was seen more noticeably with the 20 MHz probe, whereas with the 10 MHz probe scanning through the lids was possible and did not significantly affect the quality of the image. The 10 MHz probe, therefore, would be preferable in traumatised eyes or when scanning on the sclera is not advisable or practical such as in infected eyes, or with uncooperative patients. We also found that marked attenuation is encountered in eyes filled with intraocular silicone oil, making scanning of such eyes with the 20 MHz probe impossible.
CONCLUSION
The 20 MHz probe has a superior resolution and can be used to better detect details at the posterior pole and in the orbit. The 10 MHz probe has superior sensitivity and can be used to examine low intensity scatterers, such as those in the vitreous humour that cannot be easily seen using a higher frequency probe.
In general, we recommend the 10 MHz probe for initial screening of the globe and for evaluation of vitreoretinal disorders, in particular the detection of posterior vitreous detachment, vitreous haemorrhage, and subtle vitreous change such as inflammatory cells, etc. The 20 MHz probe is best utilised to better identify ocular wall and its lesions such as choroidal melanoma, choroidal naevi, disciform lesions, and posterior scleritis. The 20 MHz probe is also superior to the 10 MHz probe in the imaging of orbital fat, differentiating lesions in the orbit, extraocular muscles and optic nerve. Whenever possible, it is also advisable to scan directly on the sclera and avoid passing the beam through the lens
The development of high frequency ultrasound is a breakthrough in ultrasound technology. It allows a better choice of transducer and frequency that can be applied to a variety of clinical situations. It should be possible to develop ophthalmic ultrasound instruments with “multiple frequency transducers” for multiple clinical tasks.
REFERENCES
- 1.Baum G, Greenwood I. The application of ultrasonic locating techniques to ophthalmology: theoretic considerations and acoustic properties of ocular media: Part 1. Reflective properties. Am J Ophthalmol 1958;46:319–29. [DOI] [PubMed] [Google Scholar]
- 2.Bronson NR, Turner FT. A simple B-scan ultrasonoscope. Arch Ophthalmol 1973;90:237–8. [DOI] [PubMed] [Google Scholar]
- 3.Fielding JA. Imaging the eye with ultrasound. Br J Hosp Med 1992;47:805–15. [PubMed] [Google Scholar]
- 4.Atta HR. Ophthalmic ultrasound, a practical guide. Oxford: Butterworth-Heinemann Medical, 1996.
- 5.Atta HR. Imaging of the optic nerve with standardised echography. Eye 1988;2:358–66. [DOI] [PubMed] [Google Scholar]
- 6.Byrne SF, Glaser JS. Orbital tissue differentiation with standardised echography. Ophthalmology 1983;90:1071–90. [DOI] [PubMed] [Google Scholar]
- 7.Ossoinig KC. Echographic differentiation of vascular tumours in the orbit. Doc Ophthalmol Proc Ser 1981;29:283–91. [Google Scholar]
- 8.Thiboutot DM. Dermatological applications of high-frequency ultrasound. Proc SPIE 1999;3664:7–16. [Google Scholar]
- 9.Tobis JM, Mallery J, Mahon D, et al. Intravascular ultrasound imaging of human coronary arteries in vivo. Analysis of tissue characterizations with comparison to in vitro histological specimens. Circulation 1991;83:913–26. [DOI] [PubMed] [Google Scholar]
- 10.Kirschner-Hermanns R, Klein HM, Muller U, et al. Intra-urethral ultrasound in women with stress incontinence. Br J Urol 1994;74:315–8. [DOI] [PubMed] [Google Scholar]
- 11.Miller LS, Liu JB, Klenn PJ, et al. Endoluminal ultrasonography of the distal esophagus in systemic sclerosis. Gastroenterology 1993;105:31–9. [DOI] [PubMed] [Google Scholar]