Myasthenia gravis (MG) causes diplopia in about 90% of patients with the disease. 1– 3 Regardless of systemic treatments, complete remission occurs in only about 37%; and, even with prism glasses, an acceptable field of binocular single vision (BSV) is not always achieved. 1– 3, 5 Minimal literature has emerged describing success with strabismus surgery in patients with diplopia caused by MG despite systemic treatments. 6– 10 In all cases found published to date, surgery had been performed only after the strabismus angle concerned had been stable for at least five months. We describe two patients where strabismus surgery was used to manage unstable diplopia caused by MG with longstanding success.
Case 1
A 36 year old woman presented in 1992 with fatigable right lateral rectus weakness. She later also developed fatigable dysphagia and dysphonia. Tests for MG were equivocal until 1999 when the diagnosis was supported by Tensilon testing (with eye movement recordings) and a highly suggestive single fibre EMG. Initially, she was managed satisfactorily with systemic treatments and prisms. However, in 1995, her lateral rectus weakness became increasingly worse and she began to develop fatigable right medial rectus weakness. When there was diplopia even in the primary position she was referred for surgery. At that time there was right convergent strabismus of 45 prism dioptres and limitation of full abduction, some of which was considered likely to represent permanent muscle damage. There was no vertical component. In June 2002, with her strabismus angles still unstable, she underwent surgery involving 6 mm right medial rectus recession on an adjustable suture, and 7 mm right lateral rectus resection. The result of the extent of recession was an overcorrection and was reduced on day one. Some limitation of abduction persisted as predicted. Over the last six months measured strabismus angles have been stable and the patient describes an incremental increase in her field of BSV.
Case 2
A 59 year old woman presented in 1986 with isolated fluctuating right ptosis. Ocular MG was diagnosed with positive Tensilon testing and increased anti-acetylcholine receptor and anti-nuclear antibodies. Computed tomography (CT) of the chest was unremarkable. She later also developed fatigable diplopia but was satisfactorily controlled with systemic medical treatments. After two years of relatively stable symptoms these treatments were weaned. However, after two months, she relapsed. Furthermore, the recurrent diplopia was unstable and unresponsive to retreatment. On examination there was elevation and adduction of the left eye even in the primary position. She underwent surgery in May 1989 involving 6 mm left superior rectus recession and 5 mm right inferior rectus recession. Postoperatively there was still some left hypertropia. It was thought that this might improve with time and ongoing prednisolone but, because it did not, in July 1989 she underwent left inferior oblique recession. This resulted in complete resolution of diplopia. However, in August 1989, the patient developed generalised MG and diplopia due to involvement of previously unaffected extraocular muscles. Repeat chest CT showed an enlarged thymus which was resected with subsequent remission of all symptoms and signs. Fatigable ptosis is the only recurrent disease manifestation.
Comment
The sustained success with strabismus surgery in these two patients is related to the fact that diplopia in MG is the result of pure motor dysfunction. Central neurological mechanisms for binocular fusion remain intact. The fact that the results of the extent of surgical resection or recession varied from that anticipated in both cases is probably a consequence of the muscle pathology. Adjustable sutures allowed the necessary changes to be made relatively easily.
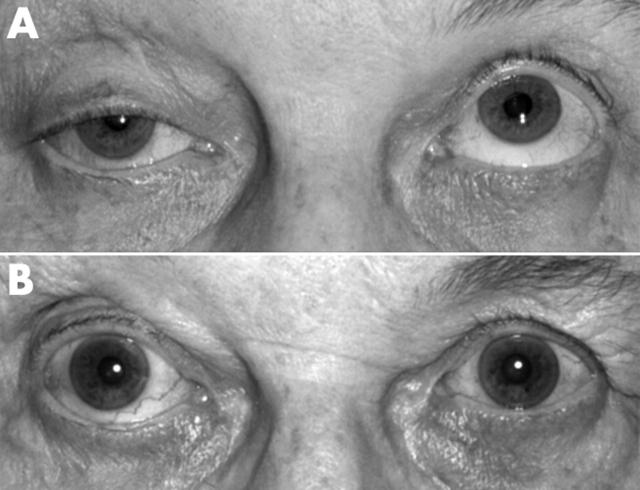
Figure 1.
Primary gaze position photographs (A) preoperatively and (B) 14 years postoperatively (July 2003).
Table 1.
Prism measurements preoperatively and 13 months postoperatively
| Prism measurements | ||
| Preoperative | ||
| 45Δ esodeviation | 45Δ esodeviation | 45Δ esodeviation |
| >45Δ esodeviation | >45Δ esodeviation | >45Δ esodeviation |
| >45Δ esodeviation | 45Δ esodeviation | >45Δ esodeviation |
| 13 months postoperative (July 2003) | ||
| 18Δ esodeviation | 0 | 10Δ esodeviation |
| 10Δ esodeviation | 0 | 0 |
| 20Δ esodeviation | 18Δ esodeviation | 1Δ exodeviation |
References
- 1. Oosterhuis HJGH. The natural course of myasthenia gravis: a long term follow-up study. J Neurol Neurosurg Psyciatry 1989;52:1121–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sommer N, Melms A, Weller M, et al. Ocular myasthenia gravis: A critical review of clinical and pathophysiological aspects. Doc Ophthalmol 1993;84:309–33. [DOI] [PubMed] [Google Scholar]
- 3. Oosterhuis HJGH. Long-term effects of treatment in 374 patients with myasthenia gravis. Monogr Allergy 1988;25:75–85. [PubMed] [Google Scholar]
- 4. Simpson JF, Westerberg MR, Magee KR. Myasthenia gravis: An analysis of 295 cases. Acta neurol scand 1966;42:1–27. [Google Scholar]
- 5. Weinberg DA, Lesser RL, Vollmer TL. Ocular myasthenia: a protean disorder. Surv Ophthalmol 1994;39:169–210. [DOI] [PubMed] [Google Scholar]
- 6. Bentley CR, Dawson E, Lee JP. Active management of patients with ocular manifestations of myasthenia gravis. Eye 2001;15:18–22. [DOI] [PubMed] [Google Scholar]
- 7. Acheson JF, Elston JS, Lee JP, et al. Extraocular muscle surgery in myasthenia gravis. Br J Ophthalmol 1991;75:232–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hamed LM, Challa P, Fanous MM, et al. Strabismus surgery in selected patients with stable myasthenia gravis. Bin Vis Eye Muscle Surg 1994;9:283–90. [Google Scholar]
- 9. Ohtsuki H, Hasebe S, Okano M, et al. Strabismus surgery in ocular myasthenia gravis. Ophthalmologica 1996;210:95–100. [DOI] [PubMed] [Google Scholar]
- 10. Davidson JL, Rosenbaum AL, McCall LC. Strabismus surgery in patients with myasthenia. J Pediatr Ophthalmol Strabismus 1993;30:292–5. [DOI] [PubMed] [Google Scholar]