Abstract
Aim: Face seeking flies have long been thought to transmit Chlamydia trachomatis, the causative agent of trachoma, but this has never been proven. The four criteria proposed by Barnett, previously used to incriminate other arthropods suspected of transmitting disease, were examined. One of these criteria remains unmet: the repeated demonstration of the presence of C trachomatis on flies. The authors used polymerase chain reaction (PCR) to look for the presence of C trachomatis DNA on flies in the Gurage Zone of Ethiopia.
Methods: Using sticky paper, one fly was collected from the face of each of 103 children aged 1–10 years. The piece of fly paper to which the fly was attached was cut out, followed by the collection of an empty piece from an arbitrary area of the fly paper, which served as control. Roche Amplicor PCR kits were used to detect C trachomatis DNA.
Results: Evidence of C trachomatis by PCR was found on 15 of 103 flies versus 0 of 103 controls (p = 0.0001).
Conclusion: These results meet the final criterion needed to incriminate flies as a vector of trachoma. However, interventional studies will be needed to show the importance of fly control.
Keywords: Chlamydia trachomatis, Musca soerbens, flies, trachoma
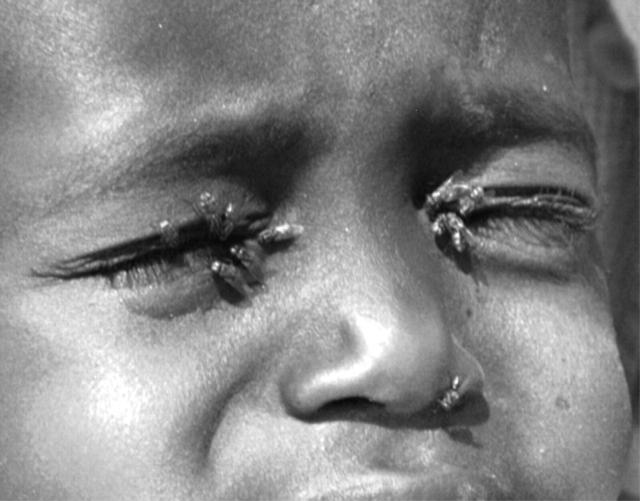
It is humbling that although trachoma has been known to cause blindness for over 3500 years, we are still not certain how it is transmitted from eye to eye. In 1598 Baron Harant de Poljits suggested that the disease was transmitted by face flies. 1 Medical students continue to be taught that along with fingers and fomites, flies are a mechanical vector for the chlamydia that causes trachoma. Anyone who has observed the staggering number of face flies passing from child to child in trachoma endemic areas needs no convincing of their vector potential (fig 1 ). In fact, a significant part of the World Health Organization’s (WHO) trachoma elimination strategy is geared towards reducing transmission by flies, but is there proof that flies can transmit trachoma?
Figure 1.
Moisture seeking Musca sorbens flies congregate around the eyes of an Ethiopian child.
To verify that flies are a vector of trachoma we can look to Barnett’s four criteria, modelled after Koch’s postulates. 2 These have been used previously to show that the mosquito, Culex tritaeniorhynchus, spreads Japanese encephalitis, and to disprove the theory that mosquitoes are a vector for HIV. For face flies and trachoma, three of the four criteria have previously been met and are described in table 1 . The final remaining criterion is in a sense the most straightforward, yet it has not been adequately demonstrated: the “repeated demonstration that the suspected arthropod species, collected under natural conditions, harbors the completely identified infectious agent ...”. 2 One anecdotal report describes chlamydia isolated with flies in Iran, but apparently there were no controls to rule out contamination. 3 In an area of the Gambia with a modest prevalence of trachoma, Emerson et al reported finding evidence of chlamydia on two of 395 flies using polymerase chain reaction (PCR), 4 which is approximately the false positive rate of the test (even PCR can have false positives). 5 We have extended these previous efforts to detect chlamydia on flies in an area of Ethiopia where approximately 50% of children aged 1–5 years are infected with chlamydia.
Table 1.
Evidence for incrimination of flies as vectors of trachoma
| Summary of Barnett’s Criteria | Evidence for accepting criterion |
| I Effective contact under natural conditions | (A) Frequent fly eye contacts shown in the Gambia (3 every 15 minutes) 4 |
| (B) Children with infective discharge had double the fly eye contacts 4 | |
| (C) Greater than 90% of fly eye contacts were Musca sorbens 4 | |
| II Convincing temporal and geographic association of the presence of vector and infection | (A) Musca sorbens recorded in areas of Australia, Africa, and the Middle East affected by trachoma 7 |
| (B) High fly densities associated with outbreaks of trachoma 7 | |
| (C) Pilot interventional study showed a significant reduction in trachoma following decrease in fly prevalence and fly eye contacts after pesticide application 6 | |
| III Vector harbours pathogen | ? |
| IV Experimental transmission | Flies shown capable of transmitting Chlamydia spp between guinea pigs under experimental conditions 8 |
MATERIALS AND METHODS
This study was conducted in May 2003 in three villages of the Gurage zone, Ethiopia. Single flies were caught with Silva Sleeve Fly Trap paper (Knäred, Sweden) from 103 children aged 1–10 years, avoiding any contact with the child’s face. Flies identified as Musca sorbens from the characteristic appearance of the thorax were passed to an assistant who cut out an approximately 1 cm2 segment of paper with the fly. Using the same scissors, a second equal sized segment was cut from an arbitrary location of the same piece of fly paper, serving as a control. The assistant then wiped the scissors with sterile alcohol pads and regloved. Samples and controls were placed at 4°C for up to 8 hours and then stored at −20°C until they were transported in cooler packs to the University of California, San Francisco, USA where they were frozen at −80°C until processing. Samples and controls were then thawed and 375 µl of sterile saline was added. Each was vortexed for two minutes and the resulting wash was pipetted into separate sterile vials labelled with random numbers to mask laboratory workers to whether the wash was from a fly or a control. The samples were then heated at 100°C for 10 minutes to reduce inhibition in the PCR assay. Roche Amplicor PCR kits were used for the detection of Chlamydia trachomatis DNA. If inhibition occurred, the samples were diluted fivefold and retested. We have previously shown that the fly paper alone does not inhibit PCR amplification of known quantities of chlamydial DNA. Equivocal reactions were repeated and counted as negative unless a single repeat reaction was positive.
RESULTS
Fifteen of 103 flies had evidence of chlamydial DNA (15%; 95% confidence interval 8 to 23%), significantly more than the matched controls (0/103, McNemar test, p = 0.0001). Five additional samples (flies and not controls) had two consecutive equivocal results, and were recorded as negative.
DISCUSSION
Our results show that a significant proportion of flies in this region carry chlamydia. In fact, 15% may be an underestimate. Some of the fly samples with equivocal results may have contained chlamydia. Additionally, transport or dilution may have lost some chlamydial bodies, and chlamydia in the stomach would not necessarily have been identified, as we performed just an external washing of the fly. Further studies will be necessary to estimate the precise proportion of flies that harbour chlamydia and how this is related to the prevalence of ocular chlamydia in a community.
Proving that chlamydia can indeed be found on face flies may be the last piece necessary to fulfil Barnett’s criteria. However, this does not establish the epidemiological importance of flies; their role may be large or insignificant. Interventional studies will be necessary to show the impact of fly control. One pilot study (referred to in table 1 ) suggested that pesticide application reduced both fly populations and active trachoma. 6 Larger scale studies examining the effect of pesticides and other more sustainable measures will be necessary to justify the large role that fly control plays in the WHO’s strategy to eliminate blinding trachoma. The benefits of fly reduction will likely not be limited to trachoma programmes. Reducing the bothersome presence of flies would be a welcome relief to those living in trachoma endemic areas and might also decrease fly borne diarrhoeal diseases.
Abbreviations
PCR, polymerase chain reaction
REFERENCES
- 1. Duke-Elder S. Conjunctival diseases. In: Diseases of the outer eye, Part 1. Volume 8 of 15. London: Kimpton, 1965:263.
- 2. Barnett HC. The incrimination of arthropods as vectors of disease. In: Strouhal H, Beier M, eds. Proceedings of the 11th International Congress of Entomology; 1960; Vienna, Austria. Vienna: Wien, 1962:341–5.
- 3. Jones BR. The prevention of blindness from trachoma. Trans Ophthalmol Soc UK 1975;95:16–33. [PubMed] [Google Scholar]
- 4. Emerson PM, Bailey RL, Mahdi OS, et al. Transmission ecology of the fly Musca sorbens, a putative vector of trachoma. Trans Roy Soc Trop Med Hyg 2000;94:28–32. [DOI] [PubMed] [Google Scholar]
- 5. Johnson RE, Green TA, Schachter J, et al. Evaluation of nucleic acid amplification tests as reference tests for Chlamydia trachomatis infections in asymptomatic men. J Clin Microbiol 2000;38:4382–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Emerson PM, Lindsay SW, Walraven GE, et al. Effect of fly control on trachoma and diarrhoea. Lancet 1999;353:1401–3. [DOI] [PubMed] [Google Scholar]
- 7. Emerson PM, Cairncross S, Bailey RL, et al. Review of the evidence base for the ‘F’ and ‘E’ components of the SAFE strategy for trachoma control. Trop Med Int Health 2000;5:515–27. [DOI] [PubMed] [Google Scholar]
- 8. Forsey T, Darougar S. Transmission of chlamydiae by the housefly. Br J Ophthalmol 1981;65:147–50. [DOI] [PMC free article] [PubMed] [Google Scholar]