We report a rare case of Langerhans cell histiocytosis (LCH) of bone in which recurrence occurred in the orbit 16 years after the initial lesion.
Case report
An otherwise healthy 23 year old man presented to the eye casualty department complaining of severe pain around his left lateral orbital rim for 8 days. Two weeks previously he had suffered a minor blow to the left side of his face. At the age of 7 he had had a sacroiliac eosinophilic granuloma, which was treated surgically.
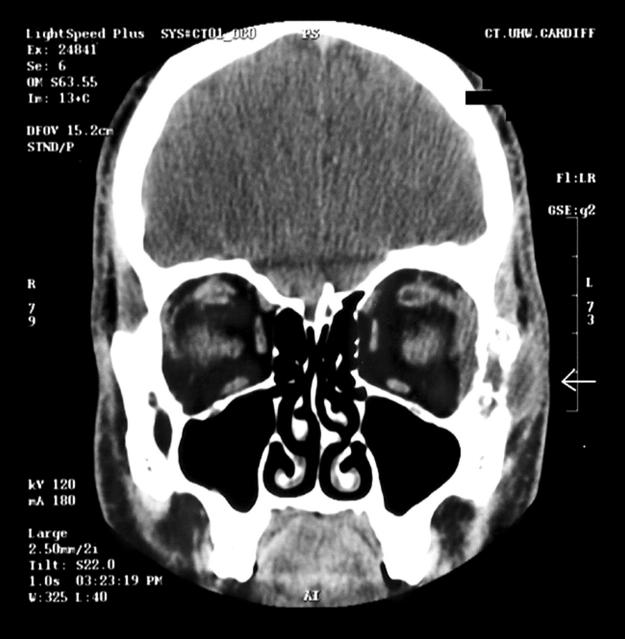
On examination, there was a small, tender, bony swelling immediately lateral to his left lateral canthus. There was no associated pyrexia, cellulitis, eyelid induration, or lymphadenopathy. Examination of the globe was normal. He was prescribed oral analgesics and antibiotics. One week later, the pain and swelling had increased and there was mild mechanical restriction of abduction of the left eye. His full blood count and liver function tests were normal. Computed tomography (CT) scanning revealed an osteolytic lesion of the lateral orbital rim (fig 1 ) with associated soft tissue swelling. A diagnosis of probable eosinophilic granuloma, disrupted by minor trauma, was made.
Figure 1.
CT scan showing the osteolytic lesion in the lateral orbital wall.
He underwent an open biopsy of the lesion, which was noted to be dark and friable with extensive oozing. A frozen section showed inflammation without giant cells or infection. Betamethasone was injected into the lesion (4 mg) and into the upper (2 mg) and lower (2 mg) eyelids.
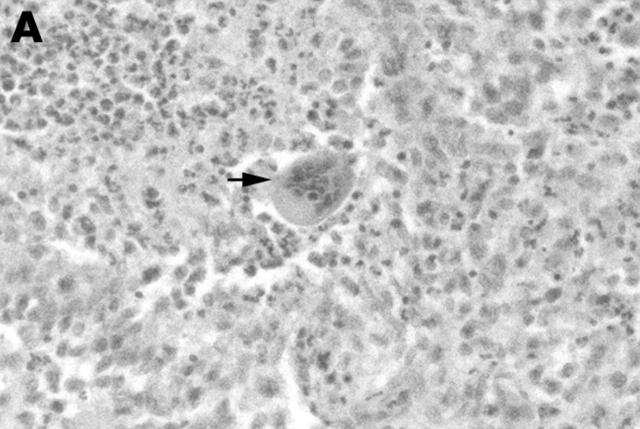
Histological examination revealed pathological Langerhans cells, CD1a and S100 positivity, and the characteristic electron microscopic appearance of Birbeck granules confirming the diagnosis of Langerhans cell histiocytosis (fig 2 ). Review of the pelvic biopsy 16 years previously demonstrated similar histological features with positive staining of tumour cells with anti CD1a. Magnetic resonance image (MRI) scanning of his brain, chest x ray, and bone scans did not reveal any other lesions. He did not have a bone marrow biopsy.
Figure 2.
(A) Photomicrograph from the orbital biopsy showing a mixed population of cells together with a multinucleated cell (arrow) typical of LCH (×100). (B) Electron microscopical photograph showing Langerhans cell with several Birbeck granules (arrows) (×26 000).
He was referred to the haematology department and was treated with intravenous vinblastine, 6 mg/m2 bolus, weekly for 6 weeks, and oral prednisolone, 40 mg/m2 per day, for 4 weeks then tapered over 2 weeks. As this represented a recurrence of the disease, systemic treatment was chosen over local excision or radiotherapy. He suffered no adverse effects from the treatment. Within 2 months, he was asymptomatic and had recovered full eye movements. A post-treatment CT scan showed no evidence of residual disease.
Comment
Langerhans cell histiocytosis encompasses three different clinical entities: (1) eosinophilic granuloma, (2) Hand-Schüller-Christian disease, and (3) Letterer-Siwe disease. They range in disease course from a benign entity with excellent prognosis in eosinophilic granuloma to the fulminant, often fatal, leukaemia-like Letterer Siwe disease. The hallmark of LCH is the pathological Langerhans cell (PLC), which is cytologically benign and resembles the normal Langerhans cell but is not morphologically dendritic. 1 PLCs result from monoclonal proliferation of CD1a histiocytes and co-express CD1a and S100 antigens on their surface. 2 They also contain the characteristic Birbeck granules as seen with electron microscopy. These are striated cytoplasmic structures with a terminal or central fusiform swelling. They are believed to originate from invaginations of the cell membrane.
LCH of bone affects children more frequently than adults and occurs most commonly in the skull. Although the orbit has been implicated previously as a primary site of LCH, 3, 4 we could not find any cases of recurrence within an orbit in our Medline literature search. Survival of bony LCH is excellent with treatment and spontaneous remission can also occur. Recurrences after initial treatment are commonly found in both mono-ostotic and polyostotic cases, usually within 12–18 months of diagnosis. 4– 6 A 16 year disease free interval is very rare. We have only found two other reports of recurrence after a quiescent period longer than 7 years. The first is a case of the same lesion recurring 13 years after original presentation. 5 The second is that of a mastoid lesion presenting 33 years after the original mandibular lesion. 5 To our knowledge, the case we have reported here represents the second longest disease free interval between consecutive LCH lesions and also the first case to reveal the orbit as a site of LCH recurrence.
References
- 1. Schmitz L, Favara BE. Nosology and pathology of Langerhans cell histiocytosis. Hematol/Oncol Clin N Am 1998;12:221246. [DOI] [PubMed] [Google Scholar]
- 2. Willman CL, Busque L, Griffith BB, et al. Langerhans’-cell histiocytosis (histiocytosis x)–a clonal proliferative disease. N Engl J Med 1994;331:154–60. [DOI] [PubMed] [Google Scholar]
- 3. Webb DKH. Histiocytic syndromes. In: Lilleyman JS, Hann IM, Blanchette VS, eds. Pediatric haematology, 2nd ed. London: Churchill Livingstone, 1999:355–69.
- 4. Feldman RB, Moore DM, Hood I, et al. Solitary eosinophilic granuloma of the lateral orbital wall. Am J Ophthalmol 1985;100:318–23. [DOI] [PubMed] [Google Scholar]
- 5. Kilpatrick SE, Wenger DE, Gilchrist GS, et al. Langerhans’ cell histiocytosis (histiocytosis X) of bone—a clinicopathologic analysis of 263 pediatric and adult cases. Cancer 1995;76:2471–84. [DOI] [PubMed] [Google Scholar]
- 6. Lieberman PH, Jones CR, Steinman RM, et al. Langerhans cell (eosinophilic) granulomatosis—a clinicopathologic study encompassing 50 years. Am J Surg Pathol 1996;20:519–52. [DOI] [PubMed] [Google Scholar]