Coat’s disease is an idiopathic condition characterised by telangiectatic and aneurismal retinal vessels changes with intraretinal and subretinal exudates.1–3 Here we report one case of a young female with an unusual manifestation of Coat’s disease.
Case report
A 14 year old female was referred for loss of vision in the left eye of a few weeks’ duration. The referring ophthalmologist thought the patient had a chorioretinal inflammatory process with secondary exudative retinal detachment and had recommended a complete medical examination for chorioretinitis.
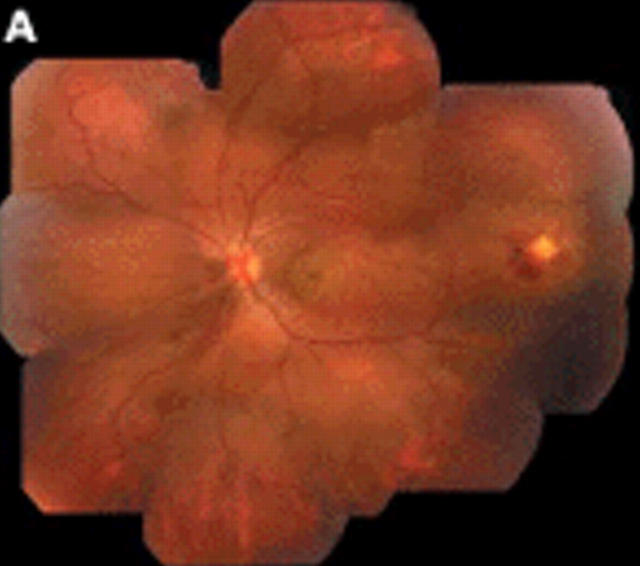
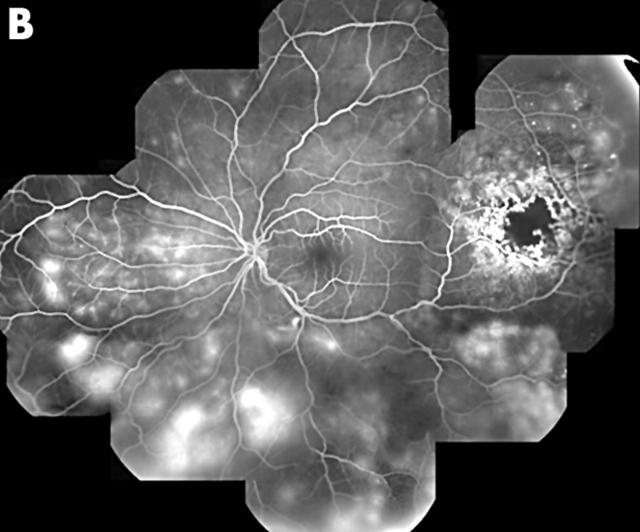
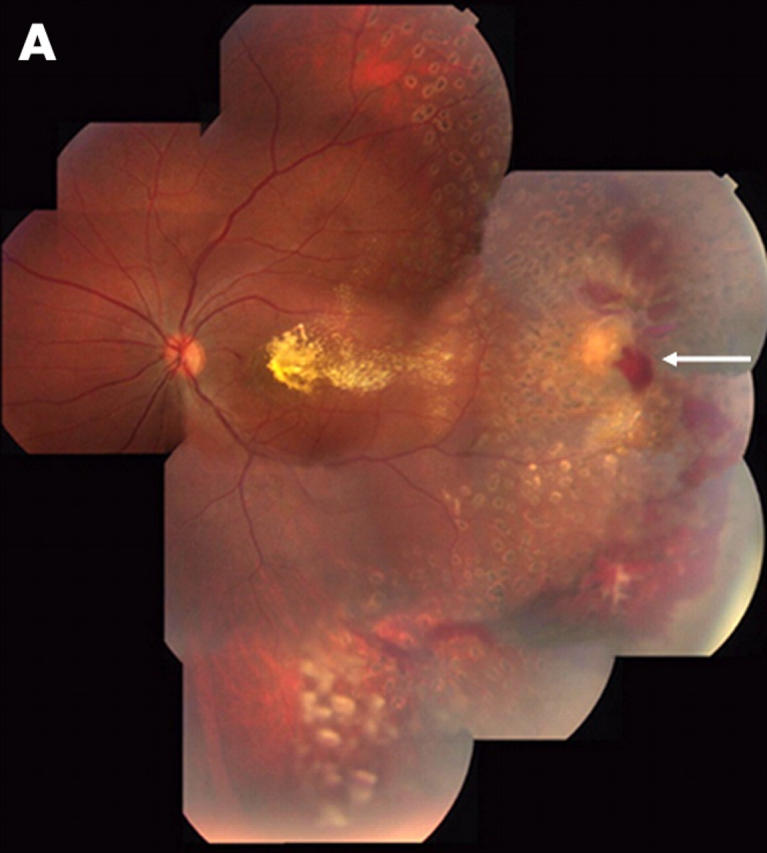
Visual acuity was 20/20 right eye and 20/400 left eye. Anterior segment examination was normal in both eyes. There were no cells or flare in the anterior chamber and in the anterior vitreous in either eye. Posterior fundus examination of the right eye was normal. In the left eye there was an exudative, neurosensory macular detachment and intraretinal lipid exudation temporally (fig 1A), leading to an area of microvascular changes in the temporal periphery. A serous, dependent neurosensory detachment with intraretinal lipid exudation was present as well. Fluorescein angiography study of the left eye confirmed the presence of marked microvascular changes in the peripheral retina (fig 1B). There was capillary non-perfusion, dilation and beading of the larger vessels, aneurysmal and telangiectasia formation. There were also telangiectatic vascular changes and intraretinal leakage of fluorescein dye throughout the peripheral fundus. The patient was diagnosed with Coats’ disease, even if the clinical presentation was somewhat unusual for Coats’ disease, given the absence of massive intraretinal and subretinal lipid exudation. A complete medical examination inclusive of PPD, chest x ray, lime titre, Bartonella titre, FTA-abs, VDRL, ACE level, CBC with differential, was negative. The patient had been an absolute vegetarian from birth; her cholesterol level was 116, and her triglyceride level was 83.
Figure 1.
(A) Composite clinical picture of the left eye demonstrated the presence of serous, neurosensory macular detachment, and mild lipid exudation. A well localised area of microvascular retinal changes was present in the temporal periphery. There was also a dependent, exudative, neurosensory detachment and mild lipid exudation throughout the fundus. (B) Composite fluorescein angiography photograph of the same eye confirmed the presence of vascular changes consistent with Coats’ disease. There was capillary non-perfusion, microaneurysm and telangiectasia formation, beading and irregularity of the larger vessel walls. Intraretinal vascular leakage was present throughout the fundus.
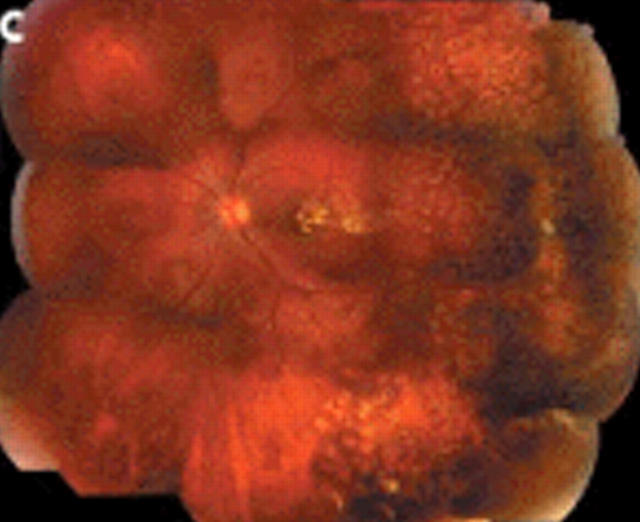
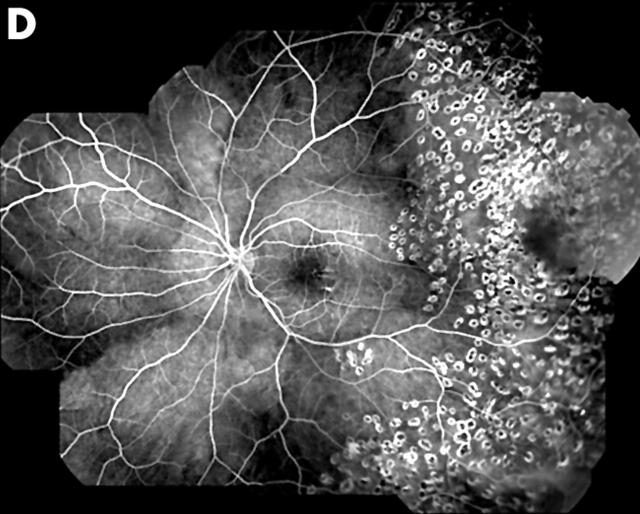
Scatter laser photocoagulation was applied around the area of telangiectatic retinal changes and in the temporal retina. Six months later the vision was improved to 20/100. There was partial resolution of the exudative, neurosensory retinal detachment and more lipid deposition in the macula. There was also new occurrence of preretinal neovascularisation and vitreous haemorrhage (fig 2A, B). Further scatter photocoagulation was applied to the temporal retina. One year after the original presentation the vision in the left eye had improved to 20/40. There was complete resolution of the exudative neurosensory detachment both in the macula and in the inferior periphery. The lipid exudation in the macula had mostly reabsorbed. There was also total regression of the preretinal neovascularisation in the temporal periphery (fig 2C, D). There was also complete resolution of the microvascular telangiectatic changes and intraretinal leakage both in the temporal retina, which had been treated with scattered laser photocoagulation and in the nasal retina, which had received no treatment.
Figure 2.
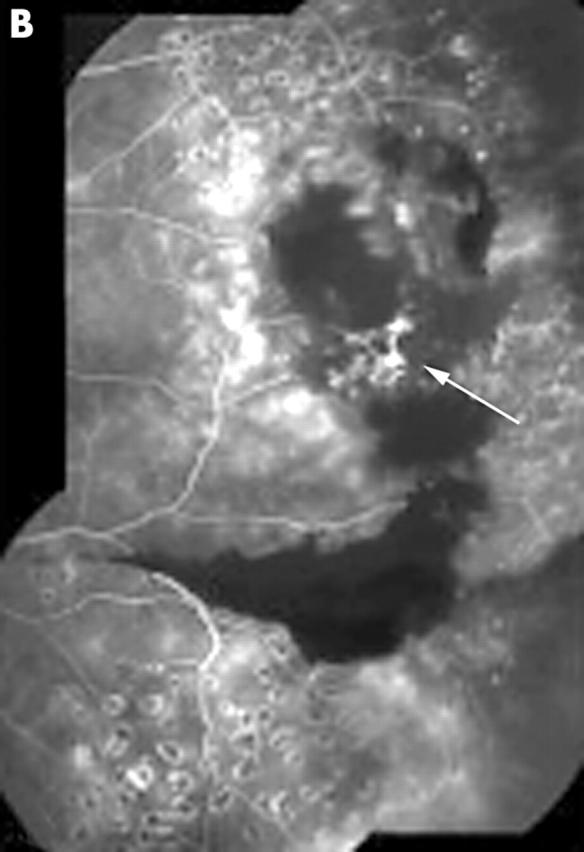
(A) Composite clinical photograph of the same eye 6 months after presentation. There was scatter laser photocoagulation temporally, partial resolution of the serous neurosensory detachment, and more lipid deposition in the macula. There was also new onset of preretinal neovascularisation temporally (arrow) and vitreous haemorrhage. (B) Composite fluorescein angiography photograph at the same time confirmed the presence of preretinal neovascularisation (arrow). (C) Composite clinical photograph of the same eye 1 year after presentation demonstrated total resolution of the exudative neurosensory detachment both in the macula and in the inferior fundus. There was regression of the preretinal neovascularisation and partial resorption of the lipid exudation. (D) Composite fluorescein angiography photograph at the same time confirms the resolution of the preretinal neovascularisation. Note also the disappearance of microvascular retinal changes and intraretinal leakage throughout the fundus.
Comment
This is an unusual manifestation of Coats’ disease because of the limited intraretinal lipid exudation.4 A possibility is that the reduced lipid exudation was related to the fact that the patient was totally vegetarian with very low cholesterol and triglyceride levels. The development of preretinal neovascularisation in the temporal periphery was also unusual. We thought that it was secondary to retinal ischaemia and not to a break in Bruch’s membrane after laser photocoagulation. We also found interesting the fact that the scatter photocoagulation of the temporal periphery resulted in regression of the microvascular telangiectatic changes both in the area that had received laser treatment and in the nasal periphery that had received no treatment. As expected, scatter laser photocoagulation resulted also in reduction of the lipid exudates, similar to what has been described in diabetic retinopathy.5
References
- 1.Egerer I , Tasman W, Tomer TL. Coats’ disease. Arch Ophthalmol 1974;92:109–12. [DOI] [PubMed] [Google Scholar]
- 2.Imre G . Coats’ disease and hyperlipemic retinitis. Am J Ophthalmol 1967;64:726–8. [DOI] [PubMed] [Google Scholar]
- 3.Silidor SW, Augsburger JJ, Shields JA, et al. Natural history and management of advanced Coats’ disease. Ophthalmic Surg 1988;19:89–93. [PubMed] [Google Scholar]
- 4.Shields JA, Shields CL. Review: Coats’ disease: the 2001 LuEsther T Mertz lecture. Retina 2002;22:80–91. [DOI] [PubMed] [Google Scholar]
- 5.Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema, ETDRS Report no 1. Arch Ophthalmol 1985;103:1796–806. [PubMed] [Google Scholar]