Abstract
Aims: To assess the effects of (1) mydriasis and (2) single versus three field photography on screening for diabetic eye disease using digital photography
Method: Slit lamp examination findings were compared to digital fundal photographs for the detection of any retinopathy and for referable retinopathy in 398 patients (794 eyes). A Topcon TRC-NW6S digital non-mydriatic fundus camera was used. Three photographic strategies were used: undilated single field, dilated single field, and dilated multiple fields. The photographs were presented in random order to one of two retinal screeners. For the single field photographs the screeners were masked to the use of mydriatics. In 13% of fundal photographs, grading was performed by both, rather than just one grader.
Results: Mydriasis reduced the proportion of ungradable photographs from 26% to 5% (p<0.001). Neither mydriasis nor three field photography improved the sensitivity or specificity for the detection of any retinopathy or of referable retinopathy when compared with undilated single field photography. The sensitivity and specificity for detecting referable retinopathy using undilated single field photography was 77% (95% CI 71 to 84) and 95 % (95% CI 93 to 97) respectively. Using dilated single field photography the figures were 81% (95% CI 76 to 87) and 92% (95% CI 90 to 94) respectively. Using dilated three field photography the figures were 83% (95% CI 78 to 88) and 93% (95% CI 91 to 96) respectively. Intergrader reliability for the detection of referable retinopathy in gradable photographs was excellent (Kappa values 0.86–1.00).
Conclusions: Mydriasis reduces the technical failure rate. Mydriasis and the three field photography as used in this study do not increase the sensitivity or specificity of detecting diabetic retinopathy.
Keywords: diabetic retinopathy, mydriasis, mass screening, tropicamide
Diabetic retinopathy is the leading cause of blindness in the working population in England and Wales.1 In patients with type 2 diabetes, 15% will require laser treatment three years after detecting mild bilateral background retinopathy at baseline.2 Timely intervention with laser photocoagulation has been shown to reduce visual loss.3 The importance of screening is well acknowledged4,5 and reported to be cost effective6,7 resulting in the recommendation of a national programme for the detection of diabetic retinopathy.8,9
Reports from the UK National Screening Committee8 and a consultation document from the Health Technology Board9 both favour a digital camera based system for screening for diabetic retinopathy. The two groups differ in their recommendations on the use of mydriasis and the number of fields to be used per eye. The UK National Screening Committee recommends routine mydriasis with two fields for each eye: nasal and macula. The Health Technology Board has advised mydriasis only when undilated photography has failed and recommend the use of a single 45° field centred on the macula. Previous studies have shown that dilated two field photography was more sensitive than undilated single field photography,10,11 but these studies were not masked and used older cameras which required larger pupil size for successful photography. It was unclear whether multiple fields, or the use of mydriasis, was the important criterion resulting in improved sensitivity. Modern cameras can produce quality images using smaller pupil diameter, potentially obviating the need for mydriasis, unless multiple field photography is required.
The present study assesses using a digital camera, mydriasis, and multiple fields as separate issues, in a randomised, masked trial for the first time.
PATIENTS AND METHODS
Subjects
Ethical approval was obtained from the Tayside Regional Ethics Committee. The study population was recruited from consecutive patients with diabetes attending the medical diabetes clinic for annual review, and from ophthalmic diabetes clinics. Patients were excluded from the study if they declined the invitation, were unable to give informed consent, were unable to position at the slit lamp table, or were unable to fixate on the light target of the camera. All recruited patients provided written informed consent.
Protocol
A Topcon TRC NW6S non-mydriatic camera (Topcon, Tokyo, Japan) with pixel density of 752×582 pixels linked to a Sony DXC-390P PAL video camera (Sony, Tokyo, Japan) was used. Patients were given 5 minutes in a darkened room to allow dark adaptation. A trained photographer (AE) took a single undilated 45° field retinal photograph centred on the fovea of each fundus. Photographs were taken in a darkened room with no natural or artificial light apart from that produced by the monitor, which faced away from the patient. On each occasion the right eye was photographed before the left and up to 10 minutes was allowed between each photograph to allow redilation. Two drops of tropicamide 1% were then instilled into each eye.
After 20 minutes, the patients were examined with a slit lamp biomicroscope by a single trained ophthalmologist (HM). The fundal features were recorded using the former UK National Screening Council recommendations (personal communication) shown in table 1. The retinal findings and further management were discussed with the patient.
Table 1.
Classification of diabetic retinopathy and outcome from the UK National Screening Committee on photograph grading guidelines
| Classification | Features | Outcome of screening |
| None | No diabetic retinopathy | Annual screening |
| Background | Microaneurysm(s) identified clinically | Annual screening |
| Retinal haemorrhage(s) +/- any exudates | Annual screening | |
| Preproliferative | Venous beading | Refer |
| Venous loop or reduplication | Refer | |
| IRMA | Refer | |
| Multiple deep, round haemorrhages | Refer | |
| Cotton wool spots | Refer | |
| Proliferative | New vessels at disc | Refer |
| New vessels elsewhere | Refer | |
| Preretinal or vitreous haemorrhage | Refer | |
| Preretinal fibrosis or tractional detachment | Refer | |
| Maculopathy | Exudate within 1 DD of fovea | Refer |
| Circinate or group of exudates within macula | Refer | |
| Any microaneurysm or haemorrhage within 1 DD of fovea | Refer | |
| Photocoagulation | Focal or macular grid | Refer |
| Peripheral scatter | Refer | |
| Other lesion | Non-diabetic pathology |
Preproliferative is the equivalent of moderate to very severe non-proliferative retinopathy.
DD, disc diameter; IRMA, intraretinal microvascular abnormalities.
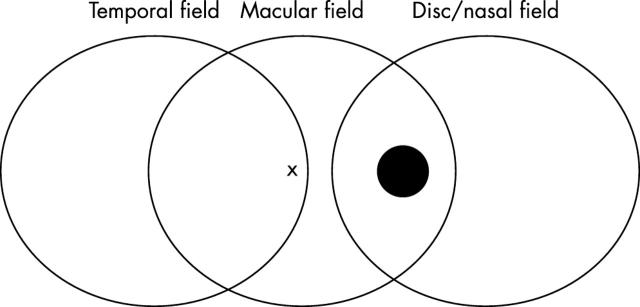
Finally a series of three 45° photographs were taken of each fundus: (1) centred on the fovea, (2) nasal retina with the temporal edge of the optic disc at the edge of the field, (3) temporal retina, with the fovea at nasal edge of the field (fig 1). The fixation targets helped achieve consistent photography, but made it difficult to perform two field photography because the fixation targets distracted the patient from looking sufficiently nasally. The three field strategy used the fixation targets available with the Topcon camera and allowed visualisation of the retinal territory included in the two field strategy of the EURODIAB protocol.12
Figure 1.
Schema of three field photography undertaken. X represents the fovea; • represents the optic disc.
The digitally stored images were presented, via TWAIN interface, onto Paint Shop Pro 5.03 software (JASC Software, Eden Prairie, MN, USA), at full capture resolution randomly to one of two retinal readers, one ophthalmologist (CM), and one diabetologist (GL). The retinal photographs were stored as bitmap images and viewed in a darkened room on CRT screens at a resolution of 1024×768 pixels.
For each eye the readers graded the three strategies of photograph: (1) single field undilated, (2) single field dilated, and (3) three fields dilated. The retinal readers were masked to any clinical information and, for the single field strategies, whether mydriasis had been used. For each individual eye the multiple field images were presented consecutively and treated as a single grading episode. For the multiple field images the graders were able to move back and forth within each triplet. The different photographic strategies were, however, randomly presented to the graders, and for an individual patient the different strategies of photography were presented to graders in a masked way and at separate times. The grading of fundal features and the guidelines for management were recorded using the same protocol as for the slit lamp examination (table 1) and was based on retinal features alone (no other clinical information was available to the photograph graders). To assess intergrader reliability for referable diabetic retinopathy 13% (50/398) of the photographs were read by both graders.
Image quality was also assessed using the system outlined in table 2, and this was used to determine gradability. Referable diabetic eye disease was defined as the presence of maculopathy, proliferative retinopathy, or preproliferative retinopathy on the UK National Screening Grading Programme. This latter category is the equivalent of moderate to very severe non-proliferative retinopathy.
Table 2.
Assessment of image quality and acceptability for grading. Photographs were deemed ungradable if any of the criteria below resulted in rejection, unless a specific reason for referral could be identified (for example, foveal changes seen even if only half the field could be visualised
| Criteria judged | Acceptance for grading |
| (a) Definition of image | |
| (i) Good; all features fully assessable | Accepted |
| (ii) Moderate; some haziness of some small vessels | Accepted |
| (iii) Poor; unable to define small vessels | Rejected |
| (b) Field of image seen | |
| (i) Full image seen | Accepted |
| (ii) >3/4 of image seen | Accepted |
| (iii) <3/4, but >1/2 of image seen | Rejected |
| (iv) <1/2 of image seen | Rejected |
| (c) Fovea visible | |
| (i) Yes | Accepted |
| (ii) No | Rejected |
Statistical analysis
A power calculation indicated that with a prevalence of referable retinopathy of 20%, and a photograph sensitivity of 80%, we would require 387 patients to be 95% confident to detect a 10% difference between screening strategies with 70% power. We thus aimed to enrol 400 patients.
Final data were placed in an SPSS database to allow statistical analysis. The χ2 test was used for categorical data. We did not carry out Fisher’s test for any table as no table had an expected cell count of less than five. Sensitivities and specificity values were calculated with 95% confidence intervals (CI) against the reference standard of slit lamp biomicroscopy. To assess the intergrader agreement the Kappa statistic is reported. The Kappa statistic represents the observed level of agreement adjusted with the level of agreement that could have been expected by chance alone.13 It is generally accepted that a value of 0.75–1.00 represents excellent agreement, 0.4–0.75 represents fair to good agreement, and values lower than this represent poor agreement.
RESULTS
The population
Of 407 patients approached, informed consent was secured from 398 (794 eyes). Six patients declined to take part in the study, two patients were unable to sit at the slit lamp, and one patient was unable to fixate the light target for the camera. The median age of patients excluded from the trial was 64.3 years (range 24–83 years). One patient was uniocular and a further patient had sufficient cataract in one eye to preclude any fundal view and was referred for cataract surgery. The median age of patients enrolled was 63.0 years (range 17–88 years, interquartile range 51.8–70.3) with 57% male. Mean duration of diabetes was 9.3 years (95% CI 8.5 to 10.1), and 35% were treated with insulin.
Of the 794 eyes, 487 (61.3%) had no retinopathy, 101 (12.7%) had background retinopathy, 162 (20.4%) had maculopathy, 37 (4.7%) had preproliferative or proliferative changes, and seven (0.9%) had non-diabetic eye disease.
Proportion of gradable photographs
Table 3 shows the percentage of photographs being reported as ungradable (technical failures) with the different photograph strategies.
Table 3.
Percentage of patients with photographs being reported as ungradable (technical failures)
| Undilated single field photographs | Dilated single field photographs | Dilated multiple field photographs | |
| Right eye only | 25% | 4% | 4% |
| Left eye only | 27% | 6% | 5.5% |
| Either eye | 36% | 7% | 6.5% |
A statistically significant difference was present in the proportion of gradable photographs between the undilated and dilated single field strategies (χ2 test statistic 135, p<0.001), and undilated and dilated multiple field strategies (χ2 test statistic 139, p<0.001). If insufficient time was allowed for redilation before photographing the second eye, a higher proportion of ungradable photographs would have been anticipated in the eye photographed second (left eye). There was no statistically significant difference in the proportion of ungradable photographs between the right and left eyes for the undilated photograph strategy (χ2 test statistic 0.254, p = 0.614).
The total number of patients with either or both eyes unreadable was 144 of the 398 (36%). Of these 144 patients, in 65 (45%) patients both eyes were unreadable, with 36 unreadable only on the right eye (25%), and 43 only on the left eye (30%).
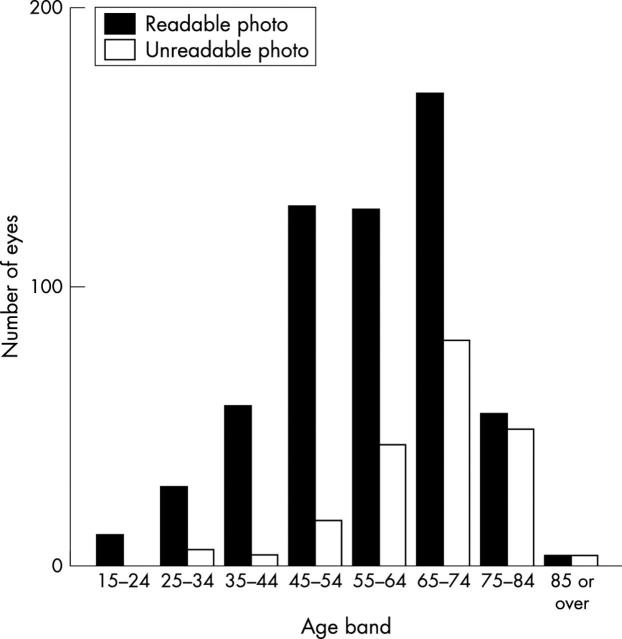
Figure 2 shows the proportion of ungradable single field images obtained through undilated pupils against age band. It illustrates the proportion of ungradable photographs increasing with age, particularly above age 55 years.
Figure 2.
Proportion of ungradable and gradable photographs within each age band for photography through undilated pupils.
No dilation resulted in 74% gradable photographs, whereas dilating all patients over 60 years of age resulted in 90% of photographs being gradable; the figure was 93% if all patients over 50 years were dilated. Dilating pupils in all patients resulted in 95% of images being gradable, with the remaining 5% being ungradable because of persistently small pupils or media opacities such as cataracts.
Sensitivity and specificity of detection of any retinopathy and of referable retinopathy (gradable photographs only)
The sensitivity and specificity for the detection of any retinopathy or of referable retinopathy with the different photography strategies are presented in table 4. These calculations are made including the results from gradable photographs only. There is no statistically significant difference in the sensitivity or specificity of the detection of any retinopathy or of referable retinopathy between the different photography strategies (table 4).
Table 4.
Sensitivity and specificity of the detection of any retinopathy with different photograph strategies (only gradable photographs included). No statistically significant difference between photography strategies
| Undilated single field (n = 585) | Dilated single field (n = 750) | Dilated multiple field (n = 752) | |
| Detection of any retinopathy | |||
| Sensitivity (95% CI) | 83% (78–88%) | 86% (82–90%) | 90% (86–93%) |
| Specificity (95% CI) | 91% (88–94%) | 91% (89–94%) | 90% (88–93%) |
| Positive predictive value (95% CI) | 85% (80–90%) | 87% (83–91%) | 86% (82–90%) |
| Negative predictive value (95% CI) | 90% (87–93%) | 91% (88–94%) | 93% (91–95%) |
| Detection of referable retinopathy | |||
| Sensitivity (95% CI) | 77% (71–84%) | 81% (76–87%) | 83% (78–88%) |
| Specificity (95% CI) | 95% (93–97%) | 92% (90–94%) | 93% (91–96%) |
| Positive predictive value (95% CI) | 85% (79–91%) | 79% (73–85%) | 82% (77–87%) |
| Negative predictive value (95% CI) | 92% (89–95%) | 93% (91–95%) | 94% (92–96%) |
Intergrader reliability
To assess intergrader reliability 50 patients (100 eyes, 500 photograph episodes) were reviewed by both screeners. The outcome of each gradable photograph for detecting referable retinopathy was used to assess reliability. Ungradable photographs were treated as “missing data”. The kappa value was 1.00 (56 cases) for the undilated single field strategy, 0.86 (90 cases) for the dilated single field strategy, and 0.88 (89 cases) for the three field strategy, representing near “excellent” agreement.
DISCUSSION
Mydriasis significantly reduced the proportion of ungradable photographs from 26% to 5% (p<0.001). Without mydriasis the proportion of ungradable photographs increased with patient age. However the use of mydriasis or of three field photography did not improve the sensitivity or specificity for the detection of any retinopathy or of referable retinopathy when using the Topcon TRC NW6S non-mydriatic camera.
The criteria we used for gradability were stringent. There will always be some degree of subjectivity when assessing image quality, but the system we developed attempted to limit this by making the reason for rejection explicit (table 2). We reported 26% (mean of right and left eyes) of ungradable photographs; this figure was of the same order of magnitude (19.7%) as another study similarly using a non-mydriatic camera.14
Calculations for sensitivity and specificity in this study are based only on the photographs that were gradable. Review of the literature suggests that most studies have excluded photograph failures,15,16 but a few have treated them as a positive diagnoses.10,11,14
Comparing this study with other studies in the literature can be difficult because of different reference parameters. In our study, we choose slit lamp biomicrosopy as our reference standard for the screening of diabetic retinopathy, which has been shown to compare favourably with seven field photography and is more acceptable for quality monitoring of screening programmes.17
Scanlon recently reported sensitivity of 87.8% and specificity of 86.1% for referable diabetic retinopathy using mydriatic digital photography,14 and Olson reported sensitivity of 93% and specificity of 87%.18 These studies used slit lamp biomicroscopy as their reference standard and are comparable with our results.
A variety of photography strategies have been suggested for screening including the use of two and three fields.12,19 The three field strategy chosen for this study was different from other groups. Our intention had been to perform two field photography according to the EURODIAB protocol,12 but the internal fixator on the Topcon camera distracted patients such that the area covered by two fields was not quite sufficient. We thus performed the three fields shown in figure 1 to ensure the EURODIAB area was covered, although, there was some additional coverage at either extreme.
We found no statistically significant difference between the proportion of readable non-mydriatic photographs on the first eye compared to the second eye (p = 0.614). Other groups have found a higher rate of unreadable non-mydriatic second eye photographs, and attributed this to insufficient dark adaptation time.20 In this study with the low illumination of the digital camera, we would suggest that a dark adaptation time of 5 minutes would probably be sufficient.
There are a clinically significant number of patients who require mydriasis to achieve gradable images. This is important if a screening programme is to achieve the National Screening Committee target of less than 5% of photographs being ungradable.8 This target has been shown to be achievable in a screening programme.21 However, 64% of patients had gradable images without the need for mydriasis. In addition, neither mydriasis nor three field photography improved sensitivity or specificity. This suggests that mydriasis is helpful in improving the proportion of gradable photographs but does not improve screening sensitivity directly. As three field photography did not improve sensitivity or specificity, our study found no justification for using mydriasis as a prerequisite for multiple fields (which require dilated pupils). To achieve optimal quality of screening in a practical setting, on the basis of our results, mydriasis could be offered either to everyone or targeted to the minority who need it. Targeted mydriasis could be implemented in a number of ways. Digital photography allows an immediate assessment of image quality, and mydriasis could be offered immediately to those who appear to need it. This would however require the judgment of the photographer. Pupil size decreases with increasing age,22 although this may be a function of diabetes duration.23 We have shown that the proportion of ungradable photographs increases with age. Using an age cut off of 55 or 60 years may be an alternative way of targeting mydriatic use and increasing the number of gradable photographs from 74% to over 90%. This has been used successfully in some screening projects as in Belfast.24 For a year on year screening programme, patients who required mydriasis one year are likely to need them subsequently, and could be targeted appropriately.
It may be easier to use mydriasis in everyone, as it is arguable whether patients would be deterred from attending screening if drops have to be used. The risk of precipitating glaucoma is negligible.25 Mydriasis does not seem to affect driving vision in young patients,26 but has been shown to do so in a group of patients of mean age 55 years,27 such that the legal requirements for driving may not be met after mydriasis. This requires further study. Avoidance of mydriasis may make a screening programme more cost effective by increasing throughput.9 This may however be offset by the delay involved in having to dilate those who fail initial undilated photography. The effects on throughput time by using such a strategy need to be tested in a field study. Single field photography will also improve cost effectiveness compared with multiple field photography by reducing patient throughput time and reducing grading time.
CONCLUSIONS
This study shows that mydriatic eye drops significantly increase the proportion of gradable photographs when using a modern digital camera in a masked study. To reduce the adverse impact of mydriasis, patients could be targeted for dilation in a number of ways that have been discussed. The use of three fields did not improve the sensitivity or specificity for the detection of any retinopathy or of referable retinopathy. On the basis of this study we would recommend consideration of selective mydriasis and single field strategy for the screening of diabetic eye disease.
Acknowledgments
We would like to thank the Ross Foundation, Tenovus, and Tayside University Hospital Trust Grants for the financial support of the project. The help and advice of Paul Baines and the statistical advice of Simon Ogston have been invaluable. Finally we would like to thank all the staff and patients in the diabetes and eye clinics who agreed to participate in the study.
Abbreviations
CI, confidence interval
DD, disc diameter
Funding: Ross Foundation, Tenovus Scotland and TUHT grant scheme.
Proprietary interests: none.
REFERENCES
- 1.Evans J , Rooney C, Ashwood F, et al. Blindness and partial sight in England and Wales: April 1990–March 1991. Health Trends 1996;28:5–12. [Google Scholar]
- 2.Kohner EM, Stratton IM, Aldington SJ, et al. Relationship between the severity of retinopathy and progression to photocoagulation in patients with type 2 diabetes mellitus in the UKPDS (UKPDS 52). Diabet Med 2001;18:178–84. [DOI] [PubMed] [Google Scholar]
- 3.Ferris FL. How effective are treatments for diabetic retinopathy? JAMA 1993;269:1290–1. [PubMed] [Google Scholar]
- 4.Fong DS, Gottlieb J, Ferris FL, et al. Understanding the value of diabetic retinopathy screening. Arch Ophthalmol 2001;119:758–60. [DOI] [PubMed] [Google Scholar]
- 5.Garvican L , Clowes J, Gillow T. Preservation of sight in diabetes: developing a national risk reduction programme. Diabet Med 2000;17:627–34. [DOI] [PubMed] [Google Scholar]
- 6.Javitt JC, Aiello LP. Preventative eye care in people with diabetes is cost-saving to the federal government: implications for health-care reform. Diabetes Care 1994;17:909–17. [DOI] [PubMed] [Google Scholar]
- 7.James M , Turner D, Broadbent DM, et al. Cost effectiveness analysis of screening for sight threatening diabetic eye disease. BMJ 2000;320:1627–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gillow JT, Gray JA. The National Screening Committee review of diabetic retinopathy screening. Eye 2001;15:1–2. [DOI] [PubMed] [Google Scholar]
- 9.Facey K , Cummins E, Macpherson K, et al. Organisation of services for diabetic retinopathy screening. Health Technology Assessment Report 1. Glasgow 2002, Health Technology Board Scotland (www.htbs.org.uk).
- 10.Lairson DR, Pugh JA, Kapadia AS, et al. Cost-effectiveness of alternative methods for diabetic retinopathy screening. Diabetes Care 1992;15:1369–77. [DOI] [PubMed] [Google Scholar]
- 11.Pugh JA, Jacobson JM, Van Heuven WA, et al. Screening for diabetic retinopathy. The wide angle camera. Diabetes Care 1993;16:889–95. [DOI] [PubMed] [Google Scholar]
- 12.Aldington SJ, Kohner EM, Meuer S, et al. Methodology for retinal photography and assessment of diabetic retinopathy: the EURODIAB IDDM complications study. Diabetologia 1995;38:437–44. [DOI] [PubMed] [Google Scholar]
- 13.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. [PubMed] [Google Scholar]
- 14.Scanlon PH, Malhotra R, Foyt C, et al. The effectiveness of screening for diabetic retinopathy by digital imaging photography and technician ophthalmoloscopy. Diabet Med 2003;20:467–74. [DOI] [PubMed] [Google Scholar]
- 15.Taylor R , Lovelock L, Tunbridge WMG, et al. Comparison of non-mydriatic retinal photography with ophthalmoscopy in 2159 patients: mobile retinal camera study. BMJ 1990;301:1243–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stellingwerf C , Hardus PL, Hooymans JM. Two field photography can identify patients with vision-threatening diabetic retinopathy: a screening approach in the primary care setting. Diabetes Care 2001;24:2086–90. [DOI] [PubMed] [Google Scholar]
- 17.Scanlon PH, Malhotra R, Greenwood RH, et al. Comparison of two reference standards in validating two field mydriatic digital photography as a method of screening for diabetic retinopathy. Br J Ophthalmol 2003;87:1258–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olson JA, Strachan FM, Hipwell JH, et al. A comparative evaluation of digital imaging, retinal photography and optometrist examination in screening for diabetic retinopathy. Diabet Med 2003;20:528–34. [DOI] [PubMed] [Google Scholar]
- 19.Harding SP, Broadbent DM, Neoh C, et al. Sensitivity and specificity of photography and direct ophthalmoscopy in screening for sight threatening eye disease: the Liverpool Diabetic Eye Study. BMJ 1995;311:1131–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heaven CJ, Cansfield J, Shaw KM. The quality of photographs produced by the non-mydriatic fundus camera in a screening programme for diabetic retinopathy: a 1 year prospective study. Eye 1993;7:787–90. [DOI] [PubMed] [Google Scholar]
- 21.Gibbins RL, Owens DR, Allen JC, et al. Practical application of the European Field Guide in screening for diabetic retinopathy by using ophthalmoscopy and 35mm retinal slides. Diabetologia 1998;41:59–64. [DOI] [PubMed] [Google Scholar]
- 22.Hreidarsson AB. Pupil size in insulin-dependent diabetes. Relationship to duration, metabolic control and long-term manifestations. Diabetes 1982;31:442–8. [DOI] [PubMed] [Google Scholar]
- 23.Cahill M , Eustace P, de Jesus V. Pupillary autonomic denervation with increasing duration of diabetes mellitus. Br J Ophthalmol 2001;85:1225–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taylor R . Practical community screening for diabetic retinopathy using the mobile retinal camera: report of a 12 centre study. Diabet Med 1996;13:946–52. [DOI] [PubMed] [Google Scholar]
- 25.Pandit RJ, Taylor R. Mydriasis and glaucoma: exploding the myth. A systematic review. Diabet Med 2000;17:693–9. [DOI] [PubMed] [Google Scholar]
- 26.Montgomery DM, MacEwen CJ. Pupil dilation with tropicamide. The effects on acuity, accommodation, and refraction. Eye 1989;3:845–8. [DOI] [PubMed] [Google Scholar]
- 27.Jude EB, Ryan B, O’Leary BM, et al. Pupillary ditatation and driving in diabetic patients. Diabetic Med 1998;15:143–7. [DOI] [PubMed] [Google Scholar]