As the number of infants born through in vitro fertilisation (IVF) grows, there is increased interest regarding the long term effects of IVF and other assisted reproduction techniques on such offspring. Recent reports have noted cancer in children born after IVF or fertility drug use (table 1).1
Table 1.
Anomalies and cancers reported in offspring of IVF
| Condition | Reference |
| Neuroectodermal tumours | White et al10 |
| Kobayashi et al11 | |
| Neuroblastoma (Note: associated with the use of fertility drugs only.) | Kramer et al12 |
| Michalek et al13 | |
| Retinoblastoma | Moll et al3 |
| Cruysberg et al14 | |
| Anteby et al2 | |
| Hepatoblastoma | Melamed et al15 |
| Toren et al16 | |
| Clear cell kidney sarcoma | Toren et al16 |
| Lymphoma | Kobayashi et al11 |
| Transposition of the great arteries | Lancaster17 |
| Berg et al18 | |
| Neural tube defects | Lancaster17 |
Several types of congenital anomalies and cancers have been reported in the literature, primarily in the form of case reports. The relation between IVF and these conditions is not definitively established.
In 2001, retinoblastoma was reported to occur in a child born through IVF in Israel.2 Since then, an additional report documented four cases from the Netherlands.3 Here we add a sixth case and the first from the United States. Of these children four had unilateral retinoblastoma and two bilateral disease (table 2).
Table 2.
Retinoblastoma in children born through IVF
| Reference | Sex and age at diagnosis (months) | Eye | Cause of subfertility | DNA 13q14 analysis | Assisted reproductive technique |
| Anteby et al2 | NR, 30 | Unilateral | NR | NR | IVF with donor sperm |
| Moll et al3 | F, 38 | Both | Unexplained | Exon 8 mutated | IVF with 6 courses of clomid |
| Moll et al3 | M, 15 | Left | Maternal cause | Normal | IVF |
| Moll et al3 | F, 34 | Right | Unexplained | Normal | IVF |
| Moll et al3 | M, 8.5 | Both | Unexplained | Intron 3 mutated | IVF with 8 AI attempts |
| Moll et al3 | F, 32 | Left | Paternal cause | Normal | IVF with ICSI |
| This report | F, 16 | Right | Maternal cause | NR | IVF |
NR, not reported; AI, artificial insemination; ICSI, intracytoplasmic sperm injection.
Current literature on retinoblastoma in children born through IVF includes three case reports that describe a total of six cases of retinoblastoma in these children. The characteristics of these patients and the patient discussed in this report are listed below.
During 2002, a 16 month old child was referred to The New York Eye Cancer Center with no known family history of eye disease. She had a blind painful right eye with neovascular glaucoma. Intraocular pressures were 35 mm Hg in the right eye, and 14 in the left. Examination of the anterior chamber of the right eye revealed cells on the corneal endothelium and iris neovascularisation. While ophthalmoscopic examination of the right eye was not possible because of opaque media, ultrasonography revealed a densely calcified mass in the posterior pole (fig 1). Computed radiographic tomography demonstrated tumour calcification with no evidence of extrascleral or optic nerve extension.4 Post-enucleation histopathology confirmed the diagnosis of retinoblastoma.5 The parents did not approve genetic studies of the child.
Figure 1.
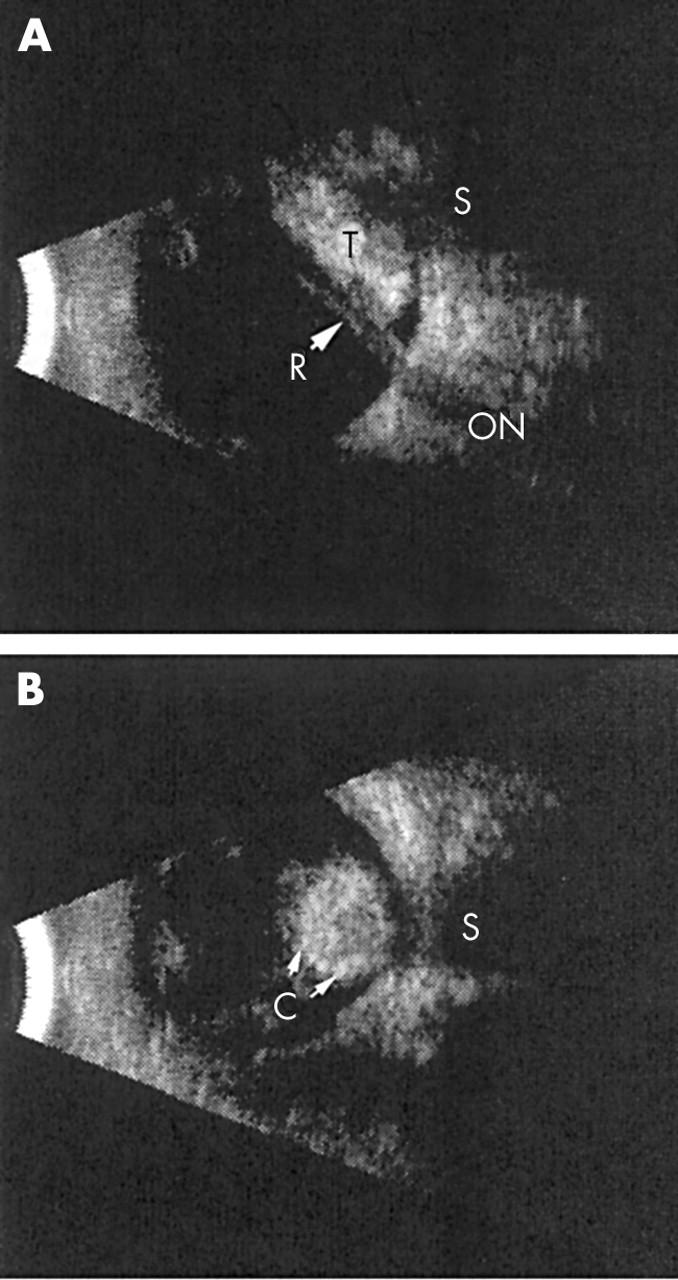
B-scan ultrasonography. (A) A longitudinal view of the right eye demonstrates a tumour posterior to a closed funnel retinal detachment. (B) A transverse view of the eye demonstrates a rounded, densely calcified tumour. R, retina; S, shadow in orbit; C, calcification; T, tumour; ON, optic nerve.
Further history revealed that this child was born through IVF with a donor egg and the father’s sperm. In order to carry the child, the postmenopausal mother received oestrogen and progesterone before and during gestation.
Comment
Several theories of IVF related carcinogenesis exist. Prenatal exposure to fertility drugs may initiate cancer in the embryo or parental germ cells. However, an evidence based association between IVF treatments and cancer development (in the women taking the drugs) has not been established.6
Another possible mechanism has been associated with the culture medium used in the IVF test tube. Experiments on mice suggest that subtle changes in the ingredients of the culture media may alter the activity of imprinted genes.7 Like fertility drugs, it remains to be seen whether altered gene imprinting can lead to cancers such as retinoblastoma.
A third possible mechanism of carcinogenesis includes inheritance of genetic defects from gametes and embryo trauma performed during routine intracytoplasmic sperm injection (ICSI) type IVF.
The most likely explanation for an increased risk of secondary carcinogenesis is that the population of patients seeking IVF is dissimilar to the general population. Patients seeking IVF are older or have medical problems that interfere with fertility. This poses a problem with any study other than a randomised prospective trial that compares babies from untreated infertility patients who become pregnant versus babies from infertile patients who become pregnant using IVF. To date all studies published are observations of clusters of disease with the suggestion that there is a cause and effect relation.8
Retinoblastoma is the most common intraocular cancer of childhood and affects approximately 300 children each year in the United States. Retinoblastoma is a manifestation of a de novo deletion or mutation of the q14 band of chromosome 13, occurring as a “second hit” during embryogenesis or the result of two hit deletions in retinal cells. In that it could be the result of chromosomal breakage and deletions in IVF born children, surveillance of retinoblastoma incidence in children born through IVF is warranted.7–9
With the advent of assisted reproductive technology (ART) in 1977, American couples have increasingly turned to such treatments to overcome fertility problems. Nationwide, 99 629 procedures were performed in 2000 by ART. In that year, fertility treatments in which the egg and sperm are handled in the laboratory resulted in 25 228 live births and 35 025 infants. This report expands information on geography and determinants of both ART success and multiple birth risks (beyond that which appears in the 2000 Assisted Reproductive Technology Success Rates19). Therefore, it seems reasonable to maintain a registry of post-IVF children, to support large epidemiological studies with long term follow up, and prospective randomised studies of infertile couples in order to determine if there is a relation between IVF and cancers such as retinoblastoma.
Supported by The EyeCare Foundation, Inc and Research to Prevent Blindness, New York City, USA.
The authors have no proprietary interest in any material mentioned in this study.
References
- 1.Klip H , Burger CW, deKraker J, et al. Risk of cancer in the offspring of women who underwent ovarian stimulation for IVF. Hum Reprod 2001;16:2451–8. [DOI] [PubMed] [Google Scholar]
- 2.Anteby I , Cohen E, Anteby E, et al. Ocular manifestations in children born after in vitro fertilization. Arch Ophthalmol 2001;119:1525–9. [DOI] [PubMed] [Google Scholar]
- 3.Moll AC, Imhof SM, Cruysberg JR, et al. Incidence of retinoblastoma in children born after in-vitro fertilisation. Lancet 2003;361:309–10. [DOI] [PubMed] [Google Scholar]
- 4.Finger PT, Harbour JW, Karcioglu Z. Risk factors for metastasis in retinoblastoma. Surv Ophthalmol 2002;47:1–16. [DOI] [PubMed] [Google Scholar]
- 5.Moshfeghi DM, Moshfeghi AA, Finger PT. Enucleation. Surv Ophthalmol 2000;44:277–301. [DOI] [PubMed] [Google Scholar]
- 6.Lerner-Geva L , Geva E, Lessing JB, et al. The possible association between in vitro fertilization treatments and cancer development. Int J Gynecol Cancer 2003;13:23–7. [DOI] [PubMed] [Google Scholar]
- 7.Doherty AS, Mann MR, Tremblay KD, et al. Differential effects of culture on imprinted H19 expression in the preimplantation mouse embryo. Biol Reprod 2000;62:1526–35. [DOI] [PubMed] [Google Scholar]
- 8.Bruinsma F , Venn A, Lancaster P, et al. Incidence of cancer in children born after in-vitro fertilization. Human Reprod 2000;15:604–7. [DOI] [PubMed] [Google Scholar]
- 9.Lerner-Geva L , Toren A, Chetrit A, et al. The risk for cancer among children of women who underwent in vitro fertilization. Cancer 2000;88:2845–7. [DOI] [PubMed] [Google Scholar]
- 10.White L , Giri N, Vowels MR, et al. Neuroectodermal tumours in children born after assisted conception. Lancet 1990;336:1577. [DOI] [PubMed] [Google Scholar]
- 11.Kobayashi N , Matsui I, Tanimura M, et al. Childhood neuroectodermal tumours and malignant lymphoma after maternal ovulation induction. Lancet 1991;338:955. [DOI] [PubMed] [Google Scholar]
- 12.Kramer S , Ward E, Meadows AT, et al. Medical and drug risk factors associated with neuroblastoma: a case-control study. J Natl Cancer Inst 1987;78:797–804. [PubMed] [Google Scholar]
- 13.Michalek AM, Buck GM, Nasca PC, et al. Gravid health status, medication use, and risk of neuroblastoma. Am J Epidemiol 1996;143:996–1001. [DOI] [PubMed] [Google Scholar]
- 14.Cruysberg JR, Moll AC, Imhof SM. Bilateral sporadic retinoblastoma in a child born after in vitro fertilization. Arch Ophthalmol 2002;120:1773 author reply 1773–4. [PubMed] [Google Scholar]
- 15.Melamed O , Bujanover Y, Hammer J, et al. Hepatoblastoma in an infant born to a mother after hormonal treatment for sterility. N Engl J Med 1982;307:820. [DOI] [PubMed] [Google Scholar]
- 16.Toren A , Sharon N, Mandel M, et al. Two embryonal cancers after in vitro fertilization. Cancer 1995;76:2372–4. [DOI] [PubMed] [Google Scholar]
- 17.Lancaster PA. Congenital malformations after in vitro fertilization. Lancet 1987;2:1392–3. [DOI] [PubMed] [Google Scholar]
- 18.Berg T , Ericson A, Hillensjo T, et al. Deliveries and children born after in-vitro fertilization in Sweden 1982–95: a retrospective cohort study. Lancet 1999;354:1579–85. [DOI] [PubMed] [Google Scholar]
- 19.National Summary and Fertility Clinic Report. Assisted reproductive technology success rates. MMWR 2000;52 No SS-9. [DOI] [PubMed] [Google Scholar]


