Furosemide is a potent diuretic which is an anthranilic acid derivative. Chemically, it is 4-chloro-N-furfuryl-5-sulfamoylanthranilic acid. Furosemide is indicated for the treatment of oedema associated with congestive heart failure, cirrhosis of the liver, and renal disease, including the nephrotic syndrome.
Here I report a case of a diabetic patient, with nephrotic syndrome, who experienced marked improvement in diabetic macular oedema after systemic treatment with furosemide.
Case report
A 41 year old woman with type II insulin dependent diabetes mellitus was referred for decrease in vision in both eyes over the past 2 months. Besides the diabetes, her past medical history was positive for irregular menstrual cycle and gastroparesis. The patient had also noticed a gain in weight of about 30 lb (13.5 kg) over the same period of time, from 154 lb (69.3 kg) to 196 lb (88.2 kg). She was treated with insulin for the diabetes and Regulin Forte for the irregular menstrual cycle. Her glycosylated haemoglobin was 9.5%.
On examination her best corrected visual acuity (VA) was 20/400 in both eyes. Anterior segment examination was normal. Dilated biomicroscopic examination of the retina of both eyes revealed diffuse macular oedema. There were also a few microaneurysms scattered throughout the posterior pole, but no hard exudates. Fluorescein angiography (FA) examination confirmed the presence of background diabetic retinopathy and demonstrated diffuse leakage in the macula of both eyes (fig 1). Optical coherence tomography (OCT) examination of the macula in both eyes confirmed the presence of macular oedema. The central retinal thickness measured by OCT was 763 μm in the right eye and 722 μm in the left eye (fig 2A–B). The patient was offered grid laser treatment for the macular oedema, but she did not feel well and she refused the treatment. A follow up appointment was arranged for 3 weeks’ time.
Figure 1.
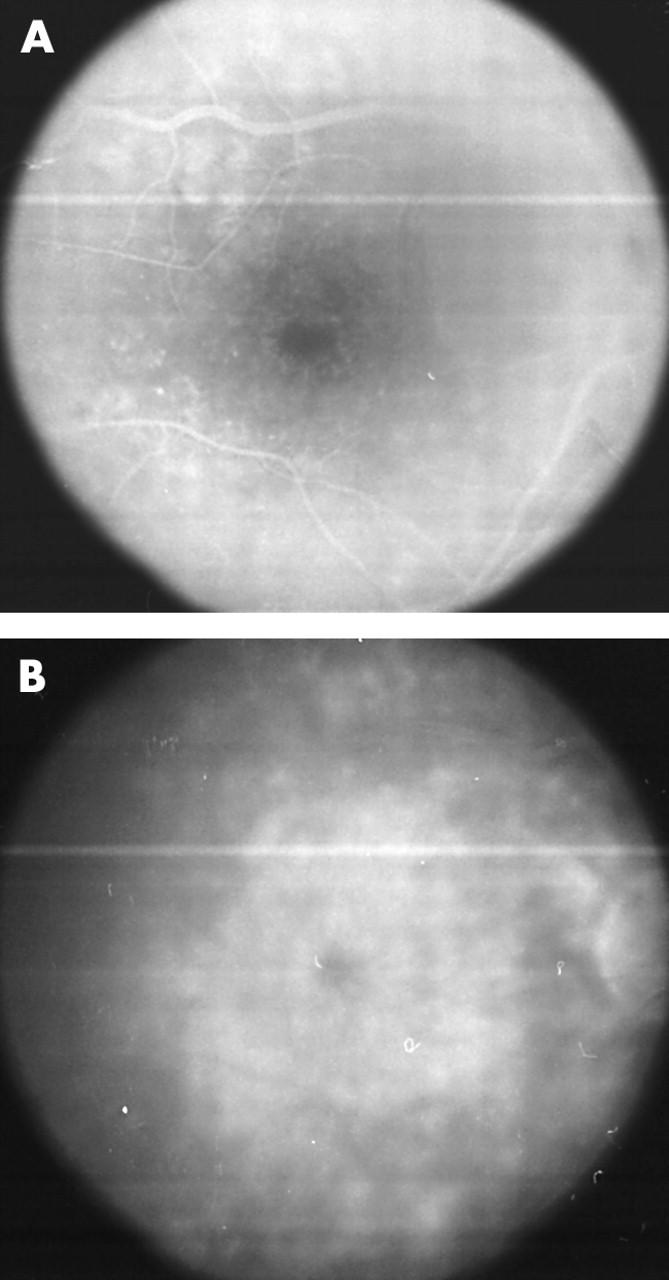
Early (A) and late (B) FA study of the right eye demonstrated diffuse leakage of dye in the macular area consistent with a diagnosis of diffuse diabetic macular oedema.
Figure 2.
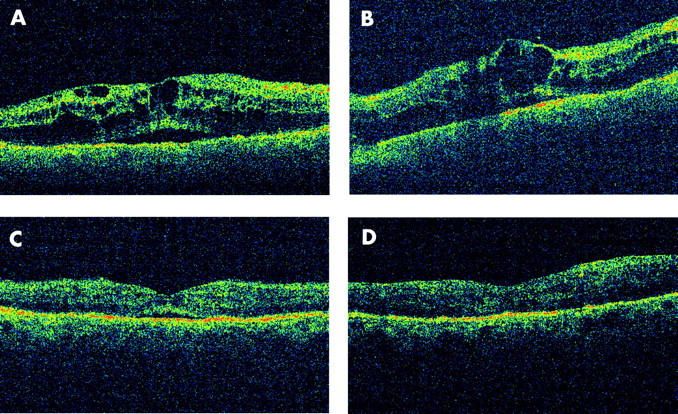
OCT examination of the right eye (A) and of the left eye (B) demonstrates marked thickening of the macula and large, intraretinal, fluid filled, cystoid spaces. Note the presence of a serous elevation of the neurosensory retina in the right eye. (C, D) OCT examination of the right eye (C) and of the left eye (D) of the same patient after systemic treatment with furosemide for 2 weeks demonstrates marked improvement in the macular oedema. There is almost complete resolution of the intraretinal cystoid spaces in both eyes. There is persistence of a small, shallow, subfoveal, serous, neurosensory detachment in the right eye.
The following day the patient presented to the emergency room complaining of nausea and weakness. She was admitted to the hospital with a diagnosis of nephrotic syndrome and fluid overload. Her albuminuria level was 350 mg/l (normal value <12 mg/l).
She was treated with systemic furosemide 40 mg twice a day for 2 weeks. A few days after starting the treatment with furosemide she began to lose weight. She also noticed an improvement in her vision. In 3 weeks the patient lost 30 lb (13.5 kg) and she had returned to her usual weight of 154 lb (69.3 kg). Three weeks later her vision had improved to 20/80 in both eyes. On fundus examination there was marked improvement in the macular oedema in both eyes. OCT examination confirmed the partial resolution of the macular oedema. The central retinal thickness measured by OCT was 250 μm in the right eye and 218 μm in the left eye (fig 2C, D)
Comment
Diabetic macular oedema is characterised by hyperpermeability of retinal blood vessels and subsequent formation of hard exudates and macular oedema, the degree of which can be estimated by measurement of retinal thickness. The severity and progression of diabetic macular oedema has been associated with the presence of nephrotic syndrome and to the degree of proteinuria.1–5 In a recent study Knudsen et al demonstrated the presence of an association between retinal thickness as evaluated OCT, and glomerular leakage as evaluated by urinary albumin excretion rate in type II diabetic patients with diabetic macular oedema.5
Nephrotic syndrome is characterised by massive proteinuria, which leads to hypoproteinaemia/hypoalbuminaemia, hyperlipidaemia with elevated cholesterols, triglycerides and other lipids, and oedema. The oedema results not only from the hypo-osmolar state caused by the loss of plasma proteins, but also from abnormal salt and water retention.
Furosemide is used in the treatment of fluid overload experienced by patients with nephrotic syndrome because it is a potent and rapid acting diuretic. It has been demonstrated that furosemide inhibits primarily the absorption of sodium and chloride not only in the proximal and distal tubules but also in the loop of Henle.
I reported what is, to my knowledge, the first case of marked improvement of diabetic macular oedema after systemic treatment with furosemide documented by OCT examination. I think that the fluid overload secondary to the nephrotic syndrome was the main cause of the worsening of the macular oedema in this patient, and that the intensive treatment with furosemide was responsible for reducing the amount of fluid overload and resolving the macular oedema. The exact mechanism of the action of furosemide in resolving the macular oedema is unknown. Tsuboi et al demonstrated that furosemide inhibits fluid absorption across retinal pigment epithelium (RPE) in an experimental model of retinal detachment in monkeys.6 According to their study furosemide could worsen the presence of a neurosensory macular detachment especially in a patient where the subneurosensory retina fluid collection is secondary to a defect in RPE pump.7 However, the FA study of this patient at presentation demonstrated multiple retinal microaneurysms at the posterior pole of both eyes and diffuse intraretinal microvascular leakage of dye in the late phase of the study. The FA study was consistent with the appearance of diffuse diabetic macular oedema. In such cases the intraretinal and subneurosensory retina leakage of dye is secondary to a microvascular retinal defect and not to a failure in the RPE pump. I think that restoration of more normal oncotic pressure within the retinal vasculature was the underlying reason for the response to the drug of the diabetic macular oedema.
References
- 1.Klein R, Klein BE, Moss SE, et al. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. IV. Diabetic macular edema. Ophthalmology 1984;91:1464–74. [DOI] [PubMed] [Google Scholar]
- 2.Sinclair SH, Nesler C, Foxman B, et al. Macular edema and pregnancy in insulin-dependent diabetes. Am J Ophthalmol 1984;97:154–67. [DOI] [PubMed] [Google Scholar]
- 3.Agardh CD, Agardh E, Torffvit O. The association between retinopathy, nephropathy, cardiovascular disease and long-term metabolic control in type 1 diabetes mellitus: a 5 year follow-up study of 442 adult patients in routine care. Diabetes Res Clin Pract 1997;35:113–21. [DOI] [PubMed] [Google Scholar]
- 4.Klein R, Klein BE, Moss SE, et al. The Wisconsin Epidemiologic Study of Diabetic Retinopathy: XVII. The 14-year incidence and progression of diabetic retinopathy and associated risk factors in type 1 diabetes. Ophthalmology 1998;105:1801–15. [DOI] [PubMed] [Google Scholar]
- 5.Knudsen ST, Bek T, Poulsen PL, et al. Macular edema reflects generalized vascular hyperpermeability in type 2 diabetic patients with retinopathy. Diabetes Care 2002;25:2328–34. [DOI] [PubMed] [Google Scholar]
- 6.Tsuboi S, Pederson JEXI. Furosemaide inhibitable fluid absorption across retinal pigment epithelium in vivo. Arch Ophthalmol 1986;104:602–3. [DOI] [PubMed] [Google Scholar]
- 7.Spitznas M. Central serous chorioretinopathy. Ophthalmology 1980;87 (8S) :88. [DOI] [PubMed] [Google Scholar]


