Abstract
Background/aim: Current evidence suggests that vascular insufficiencies in the optic nerve head play an important part in the pathogenesis of glaucomatous optic neuropathy. Trabeculectomy is the most common operative procedure for the treatment of medically uncontrolled glaucoma. This study was conducted to investigate whether trabeculectomy may improve ocular haemodynamics.
Methods: 30 patients with primary open angle glaucoma about to undergo trabeculectomy were included in the study. Patients were evaluated before surgery and at 2 and 10 weeks after trabeculectomy. Optic nerve head blood flow (OnhBF) was assessed with scanning laser Doppler flowmetry. Fundus pulsation amplitude (FPA) measurements were obtained with laser interferometry.
Results: Because of the decrease in intraocular pressure there was a significant increase in ocular perfusion pressure (OPP) following trabeculectomy (18.5% (SD 12.0%) and 19.0% (17.1%) at 2 and 10 weeks postoperatively; p <0.001). A significant increase in OnhBF was observed after trabeculectomy (11.6% (16.4%) and 16.2% (20.2%) for each postoperative visit, respectively; p <0.001). FPA was also significantly higher compared with baseline values (17.2% (17.3%) and 17.4% (16.3%), respectively; p <0.001). A significant association between the increase in OPP and the increase in OnhBF and FPA was observed 10 weeks after surgery (r = 0.47; p = 0.009, and r = 0.50; p = 0.005, respectively).
Conclusion: The results of this study suggest that trabeculectomy improves ocular blood flow in patients with chronic open angle glaucoma.
Keywords: trabeculectomy, ocular blood flow
Although elevated intraocular pressure (IOP) is an important risk factor in glaucoma, there is increasing evidence that ocular blood flow impairment also contributes to the progression of glaucomatous damage.1 Blood flow abnormalities in glaucoma have been reported using a variety of techniques (for review see Flammer et al1), but it is not yet clear whether this disturbance of blood circulation is among the causes of the disease or a result of the glaucomatous process.
Trabeculectomy is commonly performed in patients with glaucoma, in which medical therapy has failed to control IOP. However, in many cases visual field loss is not completely prevented despite a decrease in IOP. Few data are available as to whether trabeculectomy improves ocular haemodynamics. An increase in ocular blood flow in patients undergoing trabeculectomy was shown in some2,3 but not in all4 studies. The reasons for these discrepancies remain to be elucidated, but may be related to the use of different techniques, heterogeneous patient groups, small sample sizes, and the possible confounding effects of ocular hypotensive agents.
The purpose of the present study was to investigate the effect of trabeculectomy on ocular haemodynamics in patients with primary open angle glaucoma (POAG) using scanning laser Doppler flowmetry (SLDF5) and laser interferometric measurement of fundus pulsation amplitude (FPA6).
PATIENTS AND METHODS
Patients
The study protocol was approved by the ethics committee of the Vienna University School of Medicine in accordance with the Declaration of Helsinki and the good clinical practice (GCP) guidelines. After written informed consent was obtained, 52 patients with POAG scheduled for trabeculectomy were recruited to the study, but only 30 fulfilled the reproducibility criteria for blood flow measurements. The mean age of the group was 67.5 (SD 5.7) years (range 56–77 years) with 15 men and 15 women participating. POAG was diagnosed as the presence of optic disc damage and visual field defects and a history of untreated IOP of more than 21 mm Hg, as evidenced from at least three independent measurements. Exclusion criteria were evidence of any other retinal or choroidal vascular disease and history of previous trabeculectomy. In addition, patients with any sign of cataract that was likely to interfere with the optical methods were excluded. Fifteen patients received topical antiglaucoma monotherapy, and the remaining 15 patients received two different types of topical antiglaucoma medication at the time of preoperative assessment; 21 patients received β adrenergic antagonists, 13 patients a carbonic anhydrase inhibitor, and 11 patients a prostaglandin analogue.
Before surgery, all patients underwent a complete ophthalmic examination, including medical history, visual acuity, biomicroscopy, gonioscopy, and IOP measurement using an applanation tonometer (Haag Streit, Bern, Switzerland). Mean defect was attained from visual field testing with the Humphrey field analyser (full threshold program 30–2; Zeiss, San Leandro, CA, USA) and the horizontal cup/disc (C/D) ratio was determined. The characteristics of the patients are presented in table 1.
Table 1.
Baseline patient characteristics
| Mean (SD) | |
| Number of patients | 30 |
| Mean age | 67.5 (5.7) |
| Male/female | 15/15 |
| SBP (mm Hg) | 148.9 (25.3) |
| DBP (mm Hg) | 76.4 (11.0) |
| MAP (mm Hg) | 99.1 (13.5) |
| Pulse rate (min) | 75.1 (10.4) |
| IOP (mm Hg) | 23.5 (3.8) |
| Ocular perfusion pressure (mm Hg) | 42.6 (10.1) |
| Mean deviation (dB) | −8.0 (3.4) |
| C/D ratio | 0.8 (0.1) |
Ocular haemodynamic measurements were performed before surgery. All the patients then underwent standard trabeculectomy. Ocular and systemic haemodynamic parameters were measured again at 2 and 10 weeks after surgery.
Methods
Non-invasive measurement of systemic haemodynamics
Systolic, diastolic, and mean arterial blood pressure (SBP, DBP, MAP) were measured on the upper arm by an automated oscillometric device. Pulse rate (PR) was automatically recorded from a finger pulse oximeter (HP-CMS patient monitor; Hewlett-Packard, Palo Alto, CA, USA). Ocular perfusion pressure (OPP) in the sitting position was calculated as 2/3×MAP–IOP.
SLDF
The principles of SLDF (Heidelberg retina flowmeter (HRF), Heidelberg Engineering, Heidelberg, Germany) have been described in detail previously.5 Briefly, vascularised tissue is illuminated by coherent laser light. Scattering by moving red blood cells (RBCs) leads to a frequency shift in the scattered light. Accordingly, the mean RBC velocity, blood volume, and blood flow can be calculated in relative units. With SLDF these parameters are calculated for each point during the scanning process resulting in a two dimensional map of retinal and optic nerve perfusion. In the present study, one 10×10 pixel area (100×100 μm) in the optic disc (OnhBF) located temporally between the outer margin of the pallor and the margin of the optic nerve head was chosen for calculation of haemodynamic parameters. The selection of the measurement areas was based on the method described by Nicolela et al.7 Reproducibility is a critical issue with SLDF.8 Hence, at least two recordings were taken, and the mean of the two values from the best images obtained was calculated. Only flow readings with a coefficient of variation of less than 20% were included in the analysis.
Laser interferometric measurement of fundus pulsation
Pulse synchronous pulsations of the eye fundus were assessed by laser interferometry as described previously.6 Briefly, the eye is illuminated by the beam of a laser diode with a wavelength of 783 nm. The light is reflected at both the front surface of the cornea and the fundus. The two re-emitted waves produce interference fringes from which the changes in distance between cornea and retina during a cardiac cycle can be calculated. The maximum distance change is called FPA and estimates the local pulsatile ocular blood flow (POBF9). Measurements of FPA were performed in the fovea to assess pulsatile choroidal blood flow. Again, two measurements were performed at each fundus location, and the mean of the two measurements was calculated. FPAs with a coefficient of variation of more than 20% were not included in the analysis.
Data analysis
All statistical analyses were performed with Statistica for Windows (StatSoft, version 6.0). Statistical comparisons of the preoperative and postoperative parameters were made with repeated measures ANOVA. Linear correlation analysis was performed to assess the association between percentage changes in ocular haemodynamic parameters and percentage changes in IOP and OPP. Data are presented as means (SD). A two tailed p <0.05 was considered the level of significance.
RESULTS
According to the reproducibility criteria for SLDF and laser interferometry the results of 30 patients were considered for analysis only. MAP was 99.1 (13.5) mm Hg preoperatively, 100.0 (13.9) mm Hg at the first visit postoperatively, and 99.3 (12.2) mm Hg at the second visit. Mean PRs (beats/min) were 75.1 (10.4), 81.3 (10.5), and 79.2 (10.8) at baseline, and 2 and 10 weeks after surgery. A significant increase (p <0.05) in PR was observed at both postoperative visits, whereas MAP remained unchanged during the study period.
Following trabeculectomy there was a highly significant reduction in IOP. At 2 and 10 weeks after surgery the mean IOP reductions were 6.8 (28.5) mm Hg (4.5%) and 6.8 (28.9) mm Hg (4.6%), respectively (p <0.001; fig 1A). Because of the decrease in IOP there was a significant increase in OPP (18.5% (12.0%) and 19.0% (17.1%) for each postoperative visit, respectively; p <0.001).
Figure 1.
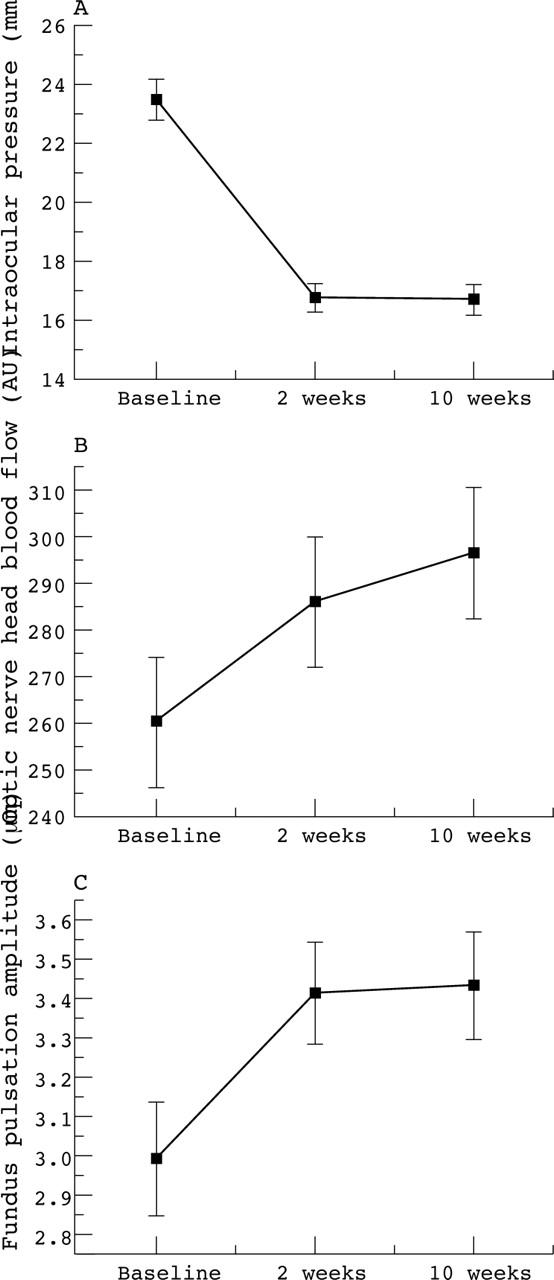
Changes in intraocular pressure (p <0.001) (A), optic nerve head blood flow (p <0.001) (B), and fundus pulsation amplitude (p <0.001) (C) in patients following trabeculectomy (n = 30). There was a significant increase in OnhBF at 2 weeks postoperatively (11.6% (16.4%); p<0.001), and at 10 weeks (16.2% (20.2%); p <0.001; B). At the first and second postoperative evaluations, FPAs were also significantly higher as compared to baseline values (17.2% (17.3%) and 17.4% (16.3%), respectively; p <0.001; C).
There was no significant correlation between percentage changes in OnhBF and percentage changes in IOP postoperatively (r = 0.25 and r = −0.15, respectively), and between percentage changes in FPA and percentage changes in IOP (r = 0.23 and r = −0.20, respectively). Increasing OPP was associated with an increase in OnhBF and FPA. This effect tended to be significant at 2 weeks (percentage changes in OPP versus percentage changes in OnhBF: r = 0.28; p = 0.128, and percentage changes in OPP versus percentage changes in FPA: r = 0.33; p = 0.07), and reached the level of significance at 10 weeks after surgery (r = 0.47; p = 0.009, and r = 0.50, p = 0.005; respectively) (fig 2). Neither OnhBF measurements nor FPA measurements were dependent on antiglaucoma therapy (p = 0.583, and p = 0.394, respectively).
Figure 2.
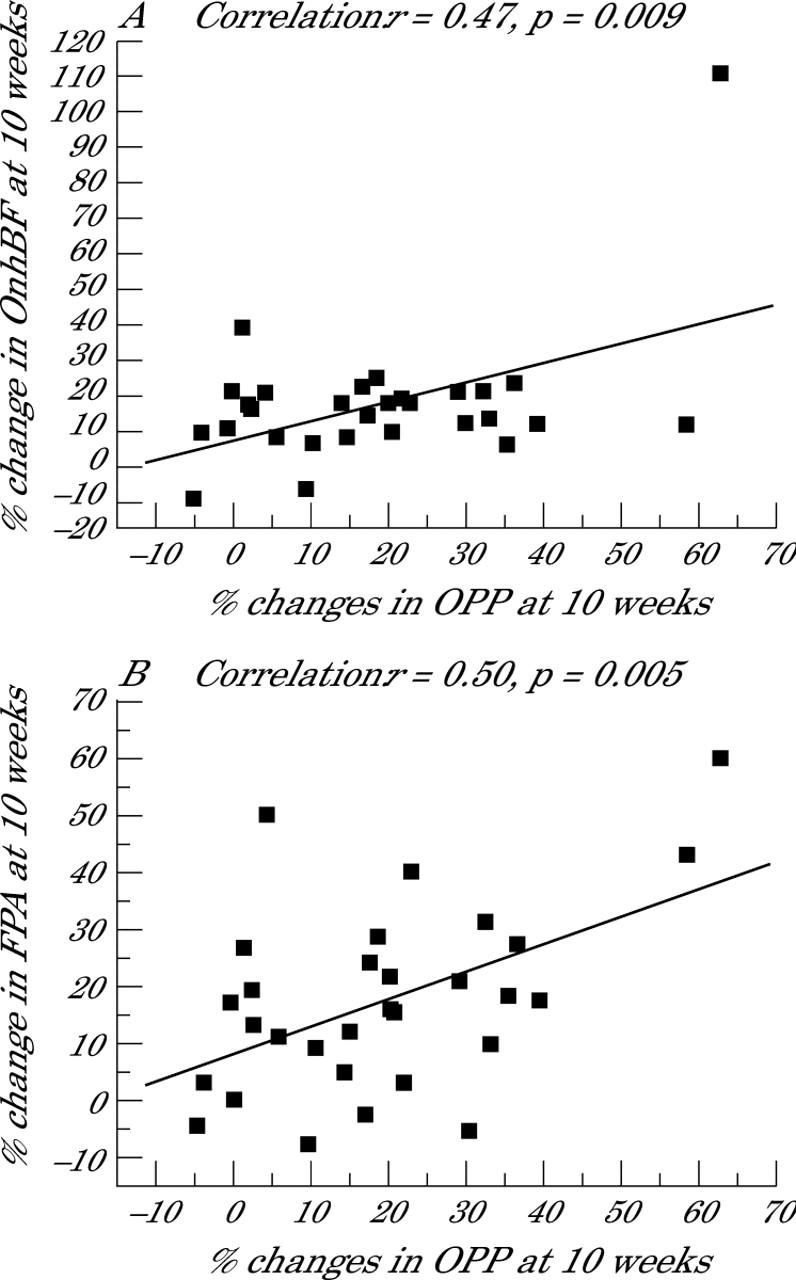
The association between percentage changes in OPP and percentage changes in OnhBF (A), and percentage changes in OPP and percentage changes in FPA (B) at 10 weeks after trabeculectomy (n = 30).
DISCUSSION
In the present study ocular haemodynamics in patients with POAG were investigated before and after trabeculectomy. A significant increase in OnhBF and FPA in the macula, indicating increased pulsatile ocular blood flow, was observed postoperatively.
Previous results concerning the effect of trabeculectomy on ocular perfusion are contradictory. Our results are comparable to those reported by Trible and colleagues,2 who found that trabeculectomy resulted in significant increase in blood velocities in retrobulbar vessels. A study by James3 found an increase of POBF following trabeculectomy, which was attributed to an increase in OPP. An increase in POBF was also reported in a retrospective study in 23 patients with normal pressure glaucoma following trabeculectomy.10 Our results are contrary to the findings of Cantor,4 who reported that surgical IOP reduction does not alter OnhBF assessed with SLDF or flow velocities in retrobulbar vessels in glaucoma patients. In contrast with the present study, however, a washout period for topical antiglaucoma medication was scheduled before surgery. Another study reporting a lack of ocular haemodynamic changes after trabeculectomy was performed with the laser speckle technique.11
When comparing the results of these studies several differences between the study designs and the methodology used need to be taken into account. On the one hand the inclusion/exclusion criteria may determine to which degree autoregulation is altered in glaucoma patients. Evidence of decreased autoregulative capacity in glaucoma patients has been provided by several investigators (for review see Flammer et al1), but little is known about the potential loss of autoregulation with progression of the disease. In the present study there was a correlation between the increase in OPP and the increase in ocular haemodynamic variables 10 weeks after surgery indicating that at least part of the ocular blood flow response is due to the decrease in IOP.
Another factor, which could contribute to the increase in ocular blood flow parameters after trabeculectomy in the present study, is that patients did not have a washout period for antiglaucoma medication. Only one previous study reported effects of trabeculectomy on ocular blood flow after withdrawal of antiglaucoma medication before surgery4 and the results were negative. Accordingly, one may speculate that in the present study cessation of topical antiglaucoma therapy may have contributed to the observed increase in ocular blood flow parameters. On the other hand the results obtained were independent of the antiglaucoma therapy and previous reports on ocular haemodynamic effects of antiglaucoma drugs are largely contradictory.12
In conclusion, the results of our study suggest that trabeculectomy not only lowers IOP, but also improves ocular blood flow in patients with chronic POAG.
Abbreviations
DBP, diastolic blood pressure
FPA, fundus pulsation amplitude
HRF, Heidelberg retina flowmeter
IOP, intraocular pressure
MAP, mean arterial blood pressure
OnhBF, optic nerve head blood flow
OPP, ocular perfusion pressure
POAG, primary open angle glaucoma
POBF, pulsatile ocular blood flow
RBCs, red blood cells
SBP, systolic blood pressure
SLDF, scanning laser Doppler flowmetry
REFERENCES
- 1.Flammer J, Orgul S, Costa VP, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res 2002;21:359–93. [DOI] [PubMed] [Google Scholar]
- 2.Trible JR, Sergott RC, Spaeth GL, et al. Trabeculectomy is associated with retrobulbar hemodynamic changes. A color Doppler analysis. Ophthalmology 1994;101:340–51. [DOI] [PubMed] [Google Scholar]
- 3.James CB. Effect of trabeculectomy on pulsatile ocular blood flow. Br J Ophthalmol 1994;78:818–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cantor LB. The effect of trabeculectomy on ocular hemodynamics. Trans Am Ophthalmol Soc 2001;99:241–52. [PMC free article] [PubMed] [Google Scholar]
- 5.Michelson G, Schmauss B, Langhans MJ, et al. Principle, validity, and reliability of scanning laser Doppler flowmetry. J Glaucoma 1996;5:99–105. [PubMed] [Google Scholar]
- 6.Schmetterer L, Lexer F, Unfried C, et al. Topical fundus pulsation measurement. Opt Eng 1995;34:711–16. [Google Scholar]
- 7.Nicolela MT, Hnik P, Drance SM. Scanning laser Doppler flowmeter study of retinal and optic disk blood flow in glaucomatous patients. Am J Ophthalmol 1996;122:775–83. [DOI] [PubMed] [Google Scholar]
- 8.Strenn K, Menapace R, Rainer G, et al. Reproducibility and sensitivity of scanning laser Doppler flowmetry during graded changes in PO2. Br J Ophthalmol 1997;81:360–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmetterer L, Dallinger S, Findl O, et al. A comparison between laser interferometric measurement of fundus pulsation and pneumotonometric measurement of pulsatile ocular blood flow. 1. Baseline considerations. Eye 2000;14:39–45. [DOI] [PubMed] [Google Scholar]
- 10.Poinoosawmy D, Indar A, Bunce C, et al. Effect of treatment by medicine or surgery on intraocular pressure and pulsatile ocular blood flow in normal-pressure glaucoma. Graefes Arch Clin Exp Ophthalmol 2002;240:721–6. [DOI] [PubMed] [Google Scholar]
- 11.Tamaki Y, Araie M, Hasegawa T, et al. Optic nerve head circulation after intraocular pressure reduction achieved by trabeculectomy. Ophthalmology 2001;108:627–32. [DOI] [PubMed] [Google Scholar]
- 12.Costa VP, Harris A, Stefansson E, et al. The effects of antiglaucoma and systemic medications on ocular blood flow. Prog Retin Eye Res 2003;22:769–805. [DOI] [PubMed] [Google Scholar]


